This review article discusses the basic principles behind the use of flaps and grafts for reconstructive surgery in the head and neck, with a special emphasis on the types of commonly used free flaps, their imaging appearance as well as some frequently encountered postoperative complications. Given the ubiquity and complexity of these reconstructive techniques, it is essential that head and neck radiologists be familiar in distinguishing between the expected evolving findings, complications, and tumor recurrence.
Key points
- •
Surgical management of advanced head and neck cancers requires complex reconstruction techniques after tumor extirpation to preserve preoperative function and cosmesis.
- •
A large variety of flaps and grafts, classified based on their blood supply, anatomic location in relation to the recipient site, and composition are used in such procedures.
- •
Knowledge of the anatomy of flaps and graft, their expected imaging appearance, the various complications (both early and delayed), and patterns of tumor recurrence after such procedures is essential in the interpretation of posttreatment surveillance imaging.
Introduction
The goals of surgical treatment of head and neck malignancy are tumor extirpation, restoration of deglutition, respiration, speech, and cosmesis. To this end, otolaryngologists have at their disposal a variety of reconstructive techniques that have been refined over the years. These techniques encompass a spectrum from simple skin grafts to complex free tissue transfer procedures. The radiologist is often presented with cross-sectional imaging studies in patients who have undergone such procedures whereby the altered anatomy makes image interpretation challenging. This review provides an overview of the more commonly used reconstructive techniques and the imaging findings of expected postoperative changes and the complications that may ensue from such procedures.
Principles and terminology
Mathes and Nahai proposed the concept of a “reconstructive ladder” in the 1970s. The ladder’s rungs described steps of reconstructive techniques of increasing complexity from secondary intention healing, primary closure, delayed closure, simple skin grafts to local, distant, and free flaps (FF). The ladder underwent reassessment in the 1990s. A “reconstructive elevator” was proposed by Gottlieb and colleagues, the principle of which is that the technique chosen must be that which achieves the best long term outcome, however complex it may be, tailored to the patient’s needs and the nature of the clinical problem and that not every problem required a free flap.
Although the terms “flap” and “graft” are sometimes used interchangeably, they represent distinct entities. A flap is tissue with intrinsic blood supply that is, not dependent on the recipient bed for perfusion whereas a graft must derive its blood supply from angiogenesis at the recipient bed. A flap’s blood supply may be derived from intact donor vasculature or may require reestablishment using microvascular techniques.
Flap nomenclature
Flaps may be classified based on their constituent tissues, blood supply, proximity to the recipient site, or the method by which they are transferred (rotation, advancement, and so forth). Several classification schemes exist. Fig. 1 provides a comprehensive overview of one such scheme (with permission from Wei FC and Mardini S. Flaps and Reconstructive Surgery. Elsevier).

Blood supply: Flaps may be “random” whereby they are supplied by unnamed vessels and derived from close proximity to the recipient site or “axial” whereby they are perfused by a named blood vessel. Random flaps are thin, comprised of skin and subcutaneous tissue, and perfused by unnamed subdermal vessels. Axial flaps are based on the “angiosome” concept of three-dimensional blocks of tissue comprised of skin and deeper structures supplied by specific source arteries. The vascular supply of a “pedicled” axial flap remains connected anatomically to its parent vessel throughout transfer while that of a “free” flap requires disconnection and reattachment using microsurgical techniques. Examples of pedicled flaps include the pectoralis major, transverse rectus abdominis myocutaneous (TRAM), and latissimus dorsi flaps. A “perforator” flap, supplied by a transmuscular/fascial leash of blood vessel feeders is comprised only of skin and/or fascial tissue and is a less morbid alternative to a myocutaneous flap. It is technically more demanding, requiring a meticulous dissection of blood vessels through muscles, thereby potentially allowing the preservation of residual muscle function. ,
Proximity: A “local” flap uses tissue that is anatomically contiguous with the recipient bed whereas a regional flap is derived from tissue that is in the vicinity but is not directly contiguous with the recipient site. “Regional” flaps, examples of which are nasoseptal and forehead flaps, used for skull base and nasal tip reconstruction respectively, derive their blood supply from the same anatomic area of the structure to be reconstructed. These may be transferred from the donor site by releasing incisions or by tunneling beneath the skin to reconstruct the recipient bed. A “distant” flap is anatomically remote from the recipient bed and may be free or pedicled. The radial forearm free flap (RFFF), anterolateral thigh (ALT), fibula free flap (FFF), and the scapular free flap are among the more commonly used FF to reconstruct defects in head and neck.
Composition: Flaps may be comprised of skin, fascia, muscle, fat, bone, or a combination of these. The head and neck region can be divided into various subunits that comprise different types of tissue. When a defect of the head and neck is created after tumor extirpation or after traumatic injury, an understanding of the type of tissues that are missing in a particular subunit can help the reconstructive surgeon determine the ideal reconstructive tool to replace the lost tissue. For example, removal of a tumor involving the left body of the mandible and overlying gingiva and adjacent floor of mouth will result in a defect of bone and soft-tissue which must be reconstructed. Flaps in general but especially FF can be categorized as soft-tissue or bone flaps. The bone flaps usually have a soft-tissue component that can be used for reconstruction.
Soft-tissue flaps can be further characterized as skin flaps, fascial flaps, muscular flaps, musculocutaneous flaps, fasciocutaneous flaps, or visceral flaps depending on the soft-tissue components present within the flap. Each of these flaps has a distinct blood supply that supplies the associated soft-tissue. Depending on the type of flap it can either be transferred to the head and neck region in a pedicled fashion (whereby the blood vessels are left intact) or as a free flap with an associated microvascular anastomosis performed to reestablish the flaps blood supply. In addition to recognizing that type of tissue loss that needs to be reconstructed, an understanding of the volume, and surface area needed can assist in determining which flap is the ideal technique for any particular patient. Flaps that have a significant muscular component or often used to reconstruct defects of the head and neck, skull base, and aerodigestive tract. These flaps can be pedicled flaps or free. Commonly used flaps includes the pectoralis major, rectus abdominis, latissimus dorsi, sternomastoid, trapezius, and myocutaneous submental island flaps among others. , The pectoralis major flap, supplied by the pectoral branch of the thoracoacromial artery, can provide coverage over a large defect and is also useful for salvage or emergency reconstruction ( Fig. 2 ). The latissimus dorsi flap, supplied by the thoracodorsal artery via the subscapular system, is a versatile flap with a large surface area and volume and a long pedicle that allows it to reach many regions in the head, neck, and scalp. It can be transferred as either a pedicled flap or a free flap. The rectus abdominis flap, the use of which may be limited in obese patients, is supplied by the deep inferior epigastric artery and provides perhaps the largest skin coverage of any flap used in the head and neck. It can be used as a free flap to reconstruct defects in the scalp, face, skull base, and pharynx. The forehead flap, known to Indian surgeons as early as 600 BCE, containing glabellar and frontalis muscle fibers and supplied by the supraorbital and supratrochlear vessels is a commonly used regional pedicled flap to repair nasal defects.

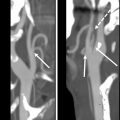
The most common soft-tissue free flap used in head and neck reconstruction include the RFFF ( Fig. 3 ) and the ALT free flap ( Fig. 4 ). The RFFF obtains its blood supply from the radial artery and the associated venae comitantes along with the cephalic vein. This free flap is composed of skin and fascia and can be modified to incorporate tendon and bone. The RFFF may be rolled to create a tube for pharyngoesophageal reconstruction ( Figs. 5 and 6 ). The RFFF may also be modified into an osteocutaneous flap to include the radius for maxillary or mandibular reconstruction ( Fig. 7 ). Approximately 50% of the width of the radius bone can be harvested with an average length of 5 to 12 cm. Benefits of the fasciocutaneous RFFF include thin, smooth, pliant skin, with potential for excellent sensory innervation and a long pedicle. Preoperative Allen’s test to ensure adequate ulnar arterial perfusion of the hand is essential before harvesting the RFFF. , An alternative to the RFFF is the ulnar forearm FF which is a fasciocutaneous flap based on the ulnar artery and its venae comitantes. Some authors arguing that the ulnar forearm free flap rarely results in flap loss, donor site morbidity, or hand ischemia, and may be associated with less hair growth and better outcomes than the RFFF. The ALT flap is based on the descending branch of the lateral femoral circumflex artery. It is a versatile flap in that it can be raised as a subcutaneous, musculocutaneous, fasciocutaneous, adipofascial, myofascial, or myocutaneous flap to reconstruct numerous head and neck defects such as those involving the scalp, skull base, pharynx, tracheal stoma, oral cavity, and oropharynx ( Fig. 8 ). A unique type of soft-tissue flaps are visceral flaps that are used in head and neck reconstruction. These include the free jejunal flap and tubed gastro-omental flap among others. Free jejunal flap transfers are the more frequently performed procedure due to low complication rates and low donor site morbidity. The low ischemic tolerance of the jejunum however may necessitate anastomosing more than one vascular pedicle to minimize postoperative thrombosis. ,






The nasoseptal flap, the workhorse flap for anterior skull base defects, is discussed in a separate chapter in this issue.
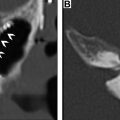
Bone or osseous flaps used in the head and neck are usually derived from the fibula, radius, or scapula. Flaps for head and neck reconstruction, on rare occasion, are derived from the iliac crest, ribs, metatarsals, medial femoral condyle, and humerus. The FFF has the ability to maintain mass over time (despite being subjected to postoperative radiation), it has a long pedicle length and it can provide a long segment of bone that can be cut contoured without impeding weight bearing thus make it the “work horse” flap for mandible reconstruction ( Fig. 9 ) , The fibula flap has specific geometric attributes in terms of how the skin paddle and the bone and the pedicle relate to each other. Given this feature of the FFF the leg that is selected for the reconstruction of a specific defect is important. For example, consider a situation or if you have a left-sided mandibular body and associated adjacent floor of mouth defect with blood vessels available in either neck. In this situation, if you select the ipsilateral leg (left leg) and orient the skin paddle to preferentially sit in the oral cavity, the pedicle will be oriented anteriorly, which will allow the surgeon to either anastomose either in the left neck or the right neck. If you select the contralateral (right) leg and orient the skin paddle to preferentially sit in the oral cavity, the pedicle will be oriented posteriorly, and the surgeon will be limited to anastomose in the ipsilateral (left) neck.

Scapular flaps may be obtained from the lateral scapular border or the tip; these flaps derive their blood supply from the circumflex or thoracodorsal branches of the subscapular artery, respectively. The scapular tip free flap (STFF) is used for shorter mandibular defects and offers the advantage of a long, reliable pedicle derived from the angular branch of the thoracodorsal artery. The FFFs and subscapular flaps provide complementary options for oromandibular reconstruction, with the former preferred for younger patients with extended defects, multiple osteotomies, and limited soft-tissue requirements. The subscapular FFs are excellent options for elderly patients, those with peripheral vascular disease, and for short defects and those requiring large, complex soft-tissue reconstruction.
A summary of the more commonly used flaps in head and neck reconstruction is presented in Table 1 (with permission from McCarty JL, et al. Am J Neuroradiol. 2019 Jan;40(1):5–13).