Fig. 3.1
A portable ultrasound machine in the operating room
The transducer must have several important characteristics. These include the frequency, the array, and the footprint. The most common transducer used for head and neck ultrasound is a linear array probe. Occasionally, a curvilinear probe may be used for wider field visualization but this is rarely needed in children. The footprint of the transducer must be appropriate to the patient. Given the varied size of the pediatric age group, generally two linear probes are used with different footprints (Fig. 3.2a). This must be balanced against the price of the probes ranging from US $ 5–10,000. If only one probe is possible, then the small “hockey stick” type probe is the most versatile (Fig. 3.2b). Finally, the transducer must have a high frequency for the most detailed pictures. Given the thinness of the neck, a high-frequency probe should be used to optimize the picture. This probe would ideally be 10–15 MHz although some use probes down to 7.5 MHz.
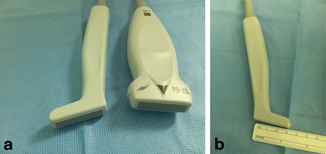
Fig. 3.2
a and b. Two linear probes with different configurations. The “hockey stick” probe
The final, and often overlooked, piece of equipment to be decided upon and used is the documentation system. Without documented images and an interpretation, the highest quality of care is not being ensured. This is both for the individual care and for the quality assurance methodology used in your practice. The capture and documentation may be part of an electronic picture archiving and communication system (PACS) within a hospital or a printer and a handwritten interpretation in an office chart. The principles, however, are the same. Representative images and an interpretation are needed to provide excellent patient care. Figure 3.3a, b demonstrates a patient with thyroiditis showing an enlarged and hypervascular gland. Documentation of these images in the chart is critical for this patient’s ongoing care.
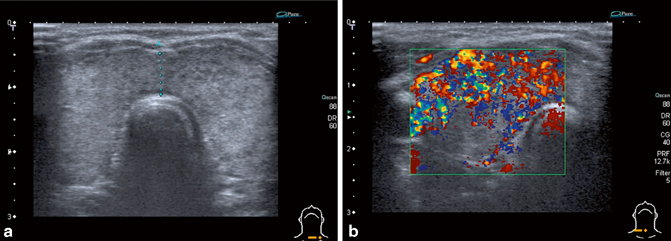
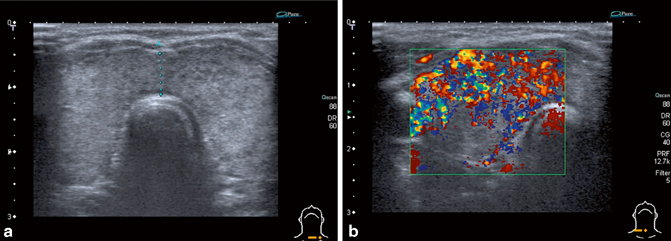
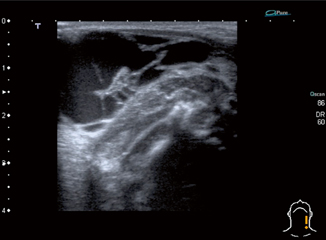
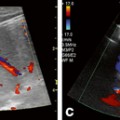
Fig. 3.3
a A 4-year-old girl with a thyroid gland scanned in the transverse plane demonstrating coarse echotexture and edema suggestive of thyroiditis. b The same patient with color Doppler demonstrating hypervascularity
Once the equipment and the patient are prepared, an approach to the patient is necessary. The first fundamental question to be asked is what is the purpose of the ultrasound examination? Are you doing a complete head and neck ultrasound or do you want a limited scan? What is the clinical indication? Is it to assess a mass? Is it to assess the patency of a vein? Is it to assess the thyroid gland? Each of these studies will have a different approach.
A complete examination of the head and neck must cover all anatomic structures and a general screen of the head and neck. There is no standard sequence within the profession [1]. Institutions or individuals must develop their own approach. However, an internal systematic approach must be done the same way every time. This systematic approach ensures that all organs and areas of the head and neck are examined. The complete examination is often done is an ultrasound department as part of a comprehensive examination.
While clinicians can do a comprehensive ultrasound examination, they often perform a focused examination to answer a clinical question and obtain any specific information. Further information may be obtained on ultrasound depending on the initial findings. An example of this is assessment of the lymph nodes when a thyroid mass is detected. Thus, clinicians are able to make a decision of further examination or intervention based on the data obtained real time. Beyond the technical aspects, more timely use of the new information is possible since the performing clinician is often the primary clinical decision-maker for this patient. The scanning technique between a complete and focused examination is the same, it is merely a decision to focus the examination to answer a specific clinical question, such as what is this mass?
One of the most common conditions asked about in pediatric patients is the lump in the neck. The assessment of this involves a detailed history and physical examination, and ultrasound is used to confirm the diagnosis or to answer a specific question such as what is this mass or does lymphadenitis have a liquefied center?
In this chapter, we discuss some of the ultrasound characteristics that are helpful in diagnosing these masses. However, as a clinician the ultrasound is an adjunct. We must never forget that the history and physical examination give us a plethora of information that will guide us to our differential diagnosis. The ultrasound adds more data to this clinical decision-making process.
Following the history and physical examination, one easy approach is to anatomically decide what region the lesion is in. Some lesions are in both. The anatomic location helps differentiate the possible lesions. Table 3.1 presents a differential diagnosis of neck masses based on location being in the anterior neck (medial to the sternocleidomastoid muscle (SCM)) or lateral neck (lateral to the SCM and including the SCM).
Table 3.1
Differential diagnosis of neck masses based on location
Anterior neck | Lateral triangle | |
|---|---|---|
Congenital | Lymphatic malformation | Lymphatic malformation |
Vascular malformation/hemangioma | Vascular malformation/hemangioma | |
Thyroglossal duct cyst | – | |
Brachial cleft cyst | – | |
Acquired | Lymphadenopathy | Lymphadenopathy |
Thyroid mass | Lipoma | |
Parathyroid mass | Paraganglioma | |
Thymus (ectopic or mass) | Torticollis |
The anterior neck contains three normal structures; we will assess as we look at a mass. Masses can come from all three. These organs are the thyroid gland, parathyroid gland, and thymus. The thyroid gland is the easiest of the three to visualize. This bi-lobar structure curves over the trachea in the lower neck. It has an isthmus that projects superior in the midline. Scanning of the thyroid should be assessed in two planes. The probe is easily slid over the lobes and simple maneuvers can allow scanning of the entire gland (Fig. 3.4).
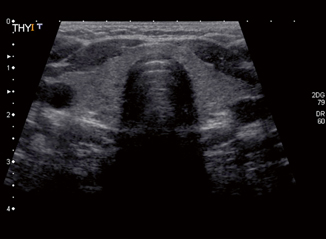
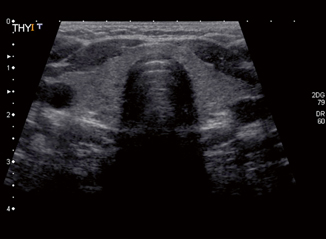
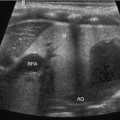
Fig. 3.4
A normal thyroid scanned in the transverse plane
Lesions of the thyroid are easily seen and can be solid or cystic. Often, there are multiple masses. No one characteristic is pathognomonic for neoplasia. However, size greater than 2 cm, microclacifications, and a completely solid lesion were predictive of neoplasia [15]. Given that neoplasia is much higher in the pediatric population, these findings warrant further investigations. If this was the lesion in question, examination can then be expanded to assess lymph nodes in both the anterior and lateral neck, as this is where regional spread would occur. This decision to further scan is made real time given your new information. Further, if the patient was old enough and cooperative, a fine needle aspiration under ultrasound control could be contemplated. The approach to interventional procedures will be discussed below.
The parathyroid glands are more difficult to identify and commonly are not seen. They are 6 × 4 mm in adults and smaller in pediatric patients. The identification of parathyroid glands on ultrasound is suggestive of a pathologic process [13].
The thymus can be found in the inferior–anterior neck. The thymus is normally 2.5 × 3 cm in newborn babies. Its relative size dissipates as the child grows. However, abnormality of organ migration can lead to ectopic thymus. This mass will live in the anterior neck. Ultrasound can easily assess this mass. Thymic tissue has a course echostructure similar to liver . It is easily delineated from the surrounding structures and has normal flow. It can have tissue going into the superior mediastinum. Besides ectopic normal thymus, cysts and occasionally masses will develop . These masses appear markedly different compared to the normal surrounding thymus. They may be solid or cystic.
Besides the three normal organs, a common mass is found in the midline. This midline anterior mass is a thyroglossal duct cyst. This superior cyst comes from the descent of the thyroid in the neck from the foramen cecum at the base of the tongue. Failure of obliteration of the thyroglossal duct can lead to cyst formation. Ultrasound has two roles in this disease process. The first is the diagnosis of the thyroglossal duct cyst. The second is to prove the existence of a normal thyroid since this midline mass may represent an ectopic thyroid and failure of decent. The thyroglossal duct cyst is a thin-walled midline cyst that is anechoic to hypoechoic. There is posterior enhancement present. This enhancement is an artifact from the fluid-filled cyst and is helpful in diagnosing fluid-filled structures (Fig. 3.5).
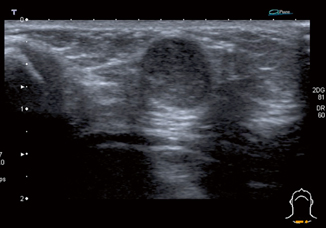
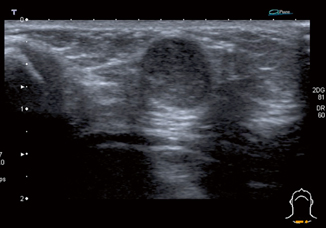
Fig. 3.5
A midline oval thyroglossal cyst in a 1-month-old infant. Note the increased posterior acoustic enhancement deep to the cyst confirming the fluid contents
If the cyst has been infected, the wall is often thicker and the fluid may be more turbid. The location of the cyst is infrahyoid in up to 65 % of the cases; however, it can also be suprahyoid. A small percentage can be intralingular [13]. Movement of the tongue outward causes an upward movement of the cyst both on physical and ultrasound examination. Ultrasound when compared to computed tomography (CT) and magnetic resonance imaging (MRI) is the best imaging modality to diagnose thyroglossal duct cysts [7].
Another common cystic mass in the neck is lymphatic malformations . These are also known as cystic hygromas and lymphangiomas. These lesions can be in any part of the body including in all aspects of the head and neck. They are congenital in nature but may present well after birth with an increase in size due to infection or bleeding. Ultrasound of the neck presents an ideal modality for both diagnosis and treatment of these complex lesions. These lesions present in a continuum from a microcystic relatively solid mass, to a macrocystic fluid-filled and typically multi-septated mass. The ultrasound characteristics vary accordingly; however, some common features do prevail. The cyst of a lymphatic malformation typically demonstrates a hypoechoic or anechoic nature with a simple wall (Fig. 3.6). If bleeding or infection has occurred, the individual or multiple cysts may show debris within rather than a simple anechoic fluid. In the case of bleeding as a presentation, layering of the clotted blood within the cyst may be seen.