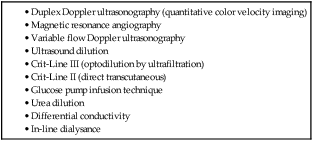
Large numbers of patients depend on hemodialysis for their survival. In the United States, approximately 370,000 individuals were receiving hemodialysis for end-stage renal disease (ESRD) through 2009.1 The increased incidence of diabetes in the U.S. population has led to an increased number of diabetic patients being treated for end-stage renal disease with hemodialysis. Growth in the incident population is particularly marked in the number of patients aged 45 to 64; growth in the population aged 75 and older has grown 12% since 2000.1 Because older patients are less likely to be candidates for renal transplantation, the number of patients on hemodialysis will increase as the population continues to age. Even patients who are transplant candidates will have a significant period of time on dialysis, because median wait times in the United States are more than 2 years and significantly increasing.1 In 2009 there were about 83,000 patients listed for transplants.1 For patients with ESRD either awaiting transplantation or who are not transplant candidates, their hemodialysis access is their “lifeline.” Dialysis access may take the form of dialysis catheters, dialysis grafts, or arteriovenous fistulas (AVFs). The AVF is the preferred access because it provides the greatest chance for long-term function. In the United States, the National Kidney Foundation Disease Outcomes Quality Initiative (NKF KDOQI) guidelines affect all dialysis centers.2 These guidelines have set a goal of 65% of all patients on hemodialysis having a functional AVF (“Fistula First Initiative”) and fewer than 10% of patients having a catheter for permanent dialysis. The rationale behind the encouragement of dialysis fistulas is the fistula’s excellent patency and low rate of complications.2 Synthetic grafts are an alternative to native fistulas, but they do not have the longevity that can be achieved with an endogenous fistula. Primary patency rates at 3 years are reported to be 40% to 60%.3 Secondary patency rates range from 50% to 90%.4 Vascular access function and patency are essential for patients on dialysis. If the access is not functioning properly, the patient will have inadequate dialysis, leading to increased morbidity and mortality.2 Numerous studies have shown a correlation between delivered dose of hemodialysis and patient mortality and morbidity.5 Vascular access–related complications account for 15% to 20% of hospitalizations for patients on hemodialysis.2 Because of the adverse outcomes for dialysis patients, preventing dialysis access dysfunction has become a focus of the KDOQI guidelines. All patients who have hemodialysis fistulas or grafts should have periodic surveillance of the dialysis access flows. The KDOQI guidelines recommend an organized monitoring/surveillance approach with regular assessment of clinical parameters of the dialysis access and hemodialysis adequacy. Data from the clinical assessment and hemodialysis measurements should be collected and tracked as part of a quality assurance program. In the KDOQI guidelines, monitoring refers to examination and evaluation of the vascular access by means of physical examination to detect physical signs that suggest the presence of dysfunction.2 Surveillance refers to periodic evaluation of the vascular access by using tests that may involve special instrumentation, and for which an abnormal test result suggests the presence of dysfunction.2 Diagnostic testing refers to specialized testing prompted by some abnormality or other medical indication and undertaken to diagnose the cause of the vascular access dysfunction. Physical examination should be performed on all fistulas and grafts at least monthly to detect dysfunction. Physical examination is useful, reliable, easily performed and inexpensive.6 A number of techniques may be used for surveillance of grafts. Those preferred include intra-access flow measurements, outlined in Table 114-1 and directly measured or derived from static venous dialysis pressures. In fistulas, recirculation may be measured using a non–urea-based dilutional method. TABLE 114-1 Methods for Measuring Flow in Dialysis Access Based on data from NKF KDOQI Guidelines. Available at http://www.kidney.org/professionals/kdoqi/guidelines.cfm. Early failure is usually due to a technical error in creation of the fistula/graft. Rarely, no underlying anatomic lesion can be identified. These patients may have had excessive postdialysis compression, hypotension, hypovolemia, compression of the graft due to sleeping position, or a hypercoagulable state, any of which may lead to thrombosis.7 Surveillance can be performed in a number of ways (see Table 114-1). Flow decreases by less than 20% until the stenosis is 40% to 50%, and then the decrease in flow is rapid as the degree of stenosis increases to 80%.2 Decreasing flows can be measured by direct flow measurements, most commonly using ultrasound dilution. Graft function can also be evaluated using venous pressure measurements that will slowly increase with the development of stenoses. Recirculation is a very late manifestation of stenosis and a poor predictor of imminent thrombosis, so it is no longer used as a measurement of graft dysfunction in the KDOQI guidelines.2 The KDOQI Venous Access Working Group strongly encourages use of physical examination for monitoring dialysis fistulas and grafts.2 There is a concern that the basic skills of inspection, palpation, and auscultation have been largely abandoned in favor of technology, and the Working Group believes these skills should be taught to all individuals who perform hemodialysis procedures. Physical findings of persistent swelling of the arm, presence of collateral veins, prolonged bleeding after needle withdrawal, or altered characteristics of pulse or thrill in the access suggest the possibility of access dysfunction. Flow through the access can be evaluated by assessing the thrill (vibration) at various points along the access.8 When there is a stenosis present, a “water-hammer” pulse is felt below the stenosis, and above the stenosis the pulse goes away abruptly.6
Surveillance of Hemodialysis Access
Indications
Contraindications
Equipment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine






