Clinical Presentation
The patient is an 81-year-old woman who has a long history of intermittent low back pain for more than 15 years. She states that she has developed difficulty when walking over the last 18 months. In particular, she can walk up to a quarter mile but then feels like she is “walking in water” with a heavy feeling in her posterior thighs extending down to the knees, right greater than left. If she continues to walk past this point, she develops a “back ache” and further heaviness in her legs. Her leg symptoms also occur when standing for any long period of time. She is not symptomatic when sitting or lying down. She does have occasional aching pain in her posterior thighs, particularly when sitting for long periods. The pain is described as aching in quality. It is 2/10 on average, 8/10 at worst when walking or standing, and 0/10 when lying down or sitting still.
Imaging Presentation
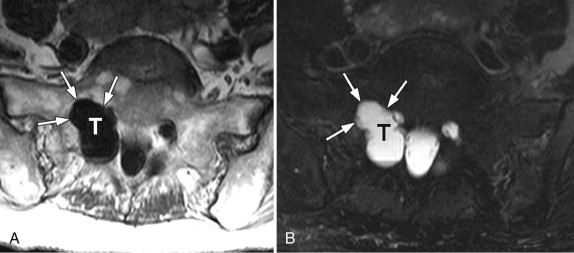
Axial T1-weighted and fat-saturated T2-weighted images demonstrate a large cerebrospinal fluid–filled region in the right S1 lateral recess. The right S1 sacral foramen is enlarged compared with the left secondary to chronic pressure erosion from this large Tarlov cyst ( Fig. 77-1 ) .
Discussion
Tarlov cysts, also known as nerve root cysts , perineurial cysts, or perineural cysts , are cerebrospinal fluid–filled cysts that occur at the junction of the posterior root and dorsal root ganglion. These cysts were originally described by Tarlov in 1938 at autopsy. The cysts are located between the perineurium and endoneurium. They are typically found in the sacral region involving the S2 and S3 nerve roots, but have been found to occur anywhere in the cervical, thoracic, and lumbar spine.
Tarlov went on to distinguish these cysts from meningeal cysts by three main findings. First, the Tarlov cyst does not have an actual communication with the spinal subarachnoid space but rather a potential one. Meningeal cysts, on the other hand, have a direct communication. During myelography, the Tarlov cyst may have delayed filling, whereas the meningeal cyst fills immediately. This delayed filling was more prevalent with the use of oil-based myelographic contrast. Second, Tarlov cysts occur at or distal to the junction of the posterior nerve root and dorsal root ganglion (DRG), whereas meningeal cysts occur proximal to the DRG. Lastly, Tarlov cysts have at least part of their wall composed of nerve fibers or ganglion cells, and meningeal cysts have an arachnoid-lined wall and do not contain nerve fibers. The first finding has been disputed and studies have shown that there is an actual communication between Tarlov cysts and the subarachnoid space. It appears that the defining feature of Tarlov cysts is the presence of nerve fibers in the cyst wall or in the cyst itself. Tarlov cysts have been classified as a Nabors type II cyst. Nabors classification type I cysts are extradural meningeal cysts without spinal nerve root fibers. Nabors classification type II cysts are extradural meningeal cysts with spinal nerve root fibers, and Nabors classification type III cysts are spinal intrudural meningeal cysts.
The pathogenesis of Tarlov cysts is unclear. Some have postulated that trauma with hemorrhage into the subarachnoid space impairs drainage of the veins of the perineurium and epineurium with resultant rupture of these veins and cyst formation. Others postulate a congenital etiology with arachnoid proliferations within the nerve root sleeve and subsequent obstruction of normal cerebrospinal fluid flow and cyst formation.
The prevalence of Tarlov cysts is estimated at 4.6% to 9%. The majority of these cysts (greater than 80%) are asymptomatic; however, they can produce, depending on location, low back pain, radicular pain, perineal pain, coccygodynia, paresthesias, bowel/bladder dysfunction, angina-like symptoms, and headaches. Symptomatic cysts cause predominantly sensory symptoms because of the proximity of the cysts to the dorsal roots and dorsal root ganglion. The patient may describe worsening symptoms on standing, coughing, or other Valsalva maneuvers. These maneuvers force more cerebrospinal fluid (CSF) into the Tarlov cyst from the spinal subarachnoid space through a ball-valve communication into the Tarlov cyst leading to transient compression and/or stretching of local nerve fibers. This ball-valve mechanism and pulsatile forces of CSF are considered to be the major contributing factors to the growth of these cysts.
The difficulty is deciding whether or not a Tarlov cyst is the symptomatic lesion because there are often other radiographic findings, such as disc degeneration, disc protrusions/herniation, and facet degeneration that may be present at the same time. One cannot assume that the mere presence of a Tarlov cyst is the causative agent. Procedures such as image-guided percutaneous cyst drainage usually yield only temporary relief; however, it can be an important diagnostic tool for the surgeon who can perform a more definitive procedure. Some have added fibrin glue after the aspiration to prevent recurrence of the cyst; however, 75% of these patients had aseptic meningitis after the procedure. Others have used high-volume lumbar punctures to attempt to decrease the hydrostatic pressure and thus lessen flow into the cyst thus ameliorating symptoms, although this is more a temporary therapeutic procedure rather than a diagnostic procedure.
Imaging Features
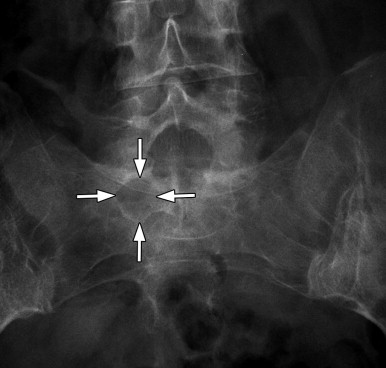
Plain film radiographs may demonstrate long-standing smooth expansile changes of a sacral foramen ( Fig. 77-2 ) , a widened spinal canal, and/or thinned pedicles; however, this is neither sensitive nor specific to a Tarlov cyst or a sacral nerve root. Furthermore, plain radiographs are unable to detect bone changes in the remainder of the spine. On noncontrast computed tomography (CT), Tarlov cysts are isodense to CSF ( Fig. 77-3 ) . The typical bone scalloping is readily identified by CT. Tarlov cysts can be seen to fill with myelographic contrast ( Fig. 77-4 ) . In the past, when oil-based contrasts such as Pantopaque were used, the Tarlov cyst frequently showed delayed filling from hours to weeks. However, with the newer water-soluble agents, a Tarlov cyst may fill as fast as the intrathecal subarachnoid space and appear as a contrast-filled elongation of the nerve root sleeve. Magnetic resonance (MR) imaging is considered to be the preferred imaging method for Tarlov cysts. With MRI, one can readily see the cyst as a rounded structure of decreased T1-signal intensity, increased T2-signal intensity without enhancement ( Fig. 77-5 ) . The nerve is often seen eccentrically located within the cyst on T2-weighted images. MRI is also useful to demonstrate the relationship of the cyst to the neural structures and the volume of the cyst.