Improvement in both hardware and software has opened up new opportunities in magnetic resonance (MR) imaging of the shoulder. MR imaging at 3-T has become a reality, with the prospect of 7-T imaging on the horizon. The art of MR arthrography continues to improve, aided by the use of novel imaging positions. New techniques for three-dimensional imaging, the reduction of metal artifact, and biochemical imaging of cartilage hold great promise.
Magnetic resonance (MR) imaging with its exquisite soft tissue discrimination and multiplanar capabilities is the imaging modality of choice in the evaluation of the painful shoulder. In many cases, the study is ordered to evaluate for shoulder pain of unknown cause. Conversely, when the source of symptoms is already clear based on physical examination and plain radiography, the examination is ordered to exclude any concomitant condition that would preclude surgery, dictate an alternative surgical approach, or could be addressed at the time of surgery. MR imaging has proved to be invaluable, particularly when addressing issues regarding the rotator cuff, articular cartilage, and labroligamentous structures.
Since the initial use of MR imaging, there has been continued progress with respect to the hardware and software, as well as innovations in the use of contrast agents and patient positioning. This article reviews the present state of MR imaging of the shoulder, highlighting recent advances and discussing controversies with regard to their relative strengths and weaknesses when appropriate. Specifically, we address the use of 3-T MR imaging, arthrography, unique positions adapted for evaluating different portions of the joint capsule, imaging of hardware in the postoperative patient, three-dimensional (3D) imaging techniques, and functional imaging.
Is bigger really better?
Imaging at 3-T
Clinical 3-T MR imaging has been one of the fastest growing sectors of the MR imaging market since 2003. This is in large part because of the advantage afforded by the inherent increase in signal-to-noise ratio (SNR) at 3-T and the potential to increase diagnostic accuracy through improved image quality. This improvement may come in the form of higher spatial resolution, speed, or optimization of contrast.
Signal and SNR increase linearly with field strength at frequencies less than 250 MHz. Thus, with all other parameters unchanged, going from 1.5- to 3-T results in a 2-fold increase in SNR. This advantage is particularly advantageous when imaging the shoulder joint, a deep portion of anatomy that is difficult to position at the isocenter of the magnet. However, as with many things in MR imaging, there are trade-offs. These include the need to minimize the increased energy deposition or specific absorption rate at greater field strengths and countering the artifacts, which can be more prominent at 3-T compared with 1.5-T.
Artifacts are also accentuated at a higher magnet strength, including chemical shift. The frequency shift between water and fat responsible for chemical shift artifact is increased from 224 Hz at 1.5-T to 448 Hz at 3-T. With respect to the images produced, this frequency shift is translated to a pixel shift. To maintain the same pixel shift at 3-T compared with 1.5-T, doubling the receiver bandwidth is indicated. This strategy increases the range of frequencies in each pixel and decreases the size of the pixel shift. Because SNR is inversely proportional to the square root of the receiver bandwidth, this results in a decrease of SNR by 44%.
Another important factor to be considered is that when the field strength increases the T1 of many tissues also increases. Longer T1 values imply that at a given time of repetition (TR), the degree of saturation increases, resulting in a loss of signal. It is thus necessary to increase the TR in most cases when using a 3-T magnet to maintain adequate T1 contrast. Because most sequences used in evaluation of the shoulder rely on intermediate weighting, this phenomenon at 3-T is not so critical.
The development of phased array coils with a greater number of elements and more flexible designs that allow positioning closer to the anatomy of interest has provided a method for gaining increased signal. The increased signal available at 3-T and with the use of phased array coils has opened the way to the use of parallel imaging of the shoulder. Parallel imaging involves the use of the individual elements in a coil to achieve spatial localization, thus reducing the number of phase encoding steps and providing adequate K space filling. However, the trade-off occurs in the form of SNR, because the information from the various coil elements is used independently as opposed to being combined. This situation results in a decrease of SNR proportional to the square root of the temporal resolution. This decreased SNR limits the use of parallel imaging to situations in which there is adequate signal, such as the use of phased array coils and 3-T magnets.
The early results on MR imaging of the shoulder at 3-T have been promising. Magee and Williams retrospectively evaluated 100 MR images of the shoulder at 3-T. Comparing the results with arthroscopy, they found a sensitivity of 90% and specificity of 100% for the detection of SLAP (superior labrum from anterior to posterior) tears. The sensitivity and specificity for tears of the anterior labrum was 89% and 100% and for posterior labral tears was 86% and 100%. These results are comparable and, in many cases, better than those previously reported for the sensitivity and specificity for detecting labral tears at 1.5-T (44%–100% and 66%–100%, respectively).
Regarding rotator cuff lesions, Magee and Williams retrospectively reviewed 150 shoulder MR images at 3-T for the assessment of supraspinatus tendon tears. Comparing with arthroscopy, they found a sensitivity and specificity for detection of full-thickness tears of 98% and 96% and for partial-thickness tears of 92% and 100%. Previous studies have shown conventional MR imaging of the shoulder at 1.5-T to have a sensitivity and specificity in the range of 84% to 100% and 86% to 98% for detection of full-thickness supraspinatus tendon tears and sensitivity and specificity in the range of 35% to 92% and 85% to 97% for partial-thickness tears. This seems to imply comparable performance with respect to full-thickness tears and an improvement with respect to the detection of partial-thickness tears. However, to our knowledge, there is no controlled study showing a significant diagnostic improvement of 3-T over 1.5-T for shoulder lesions.
In our experience, the increased signal afforded by the use of 3-T imaging has allowed for finer matrices and increased in-plane resolution, resulting in better overall image quality and more detailed evaluation of fine intra-articular structures, creating greater diagnostic confidence, particularly with respect to labral ( Fig. 1 ) and chondral lesions ( Fig. 2 ) as well as partial rotator cuff tears.


Table 1 summarizes the protocol for shoulder MR imaging at 3-T at our institution.
| Sequence | TR (ms) | Echo Time (ms) | Slice (mm) | Matrix (%) | Field of View (mm) |
|---|---|---|---|---|---|
| Axial proton density | 3030 | 33 | 2.0 | 256 × 100 | 140 × 140 |
| Coronal T2 fat-saturated | 3500 | 72 | 3.0 | 256 × 151 | 140 × 140 |
| Coronal proton density | 4500 | 32 | 2.0 | 320 × 75 | 140 × 140 |
| Sagittal T2 fat-saturated | 5000 | 62 | 2.5 | 320 × 75 | 140 × 140 |
| Sagittal T1 | 600 | 11 | 2.5 | 320 × 90 | 140 × 140 |
To inject or not to inject
The Arthrography Question
Over time, it has become the standard of practice at many imaging centers to request MR arthrographic examinations, particularly in the postoperative patient or when evaluating for undersurface tears of the rotator cuff as well as when the presence of intra-articular bodies and lesions of the glenoid cartilage and labroligamentous structures is suspected. Arthrography can be performed using direct or indirect techniques.
Direct MR arthrography (D-MRA) of the shoulder is an invasive procedure that is well tolerated by most patients. It involves the injection of a contrast solution into the shoulder joint to distend the capsule and outline the intra-articular structures, thereby improving their delineation and evaluation at subsequent MR imaging ( Fig. 3 ).

Most arthrographic examinations involve the injection of dilute gadolinium (Gd) solution in a concentration of 1 to 2 mmol/L. Needle placement for intra-articular contrast injection is usually achieved with fluoroscopic or sonographic guidance. Iodinated contrast can be included in the solution to confirm needle placement and confirm an intra-articular injection. Many radiologists choose an anterior approach for evaluation of suspected lesions of the posterior labroligamentous structures and a posterior approach when the symptoms point to involvement of the anterior labrum and capsule. This strategy is used to prevent inadvertent extravasation injection of contrast material, thus obscuring important findings. The rotator interval approach has been advocated by others as an alternative anterior mode of access, resulting in a lower probability of injury to key intra-articular structures. Ultrasonography has been used to guide both posterior and rotator interval approaches.
Indirect MR arthrography (I-MRA) is based on the principle that intravenous contrast material diffuses into the joint space over time, producing an arthrographic effect. In I-MRA, Gd-based contrast in a concentration of 0.1 mmol/kg is injected intravenously and MR imaging is performed after a delay. Intravenous Gd diffuses from the capillary bed into the interstitial space of the synovium and then leaks into the joint space. The arthrographic effect is dependent on the permeability of the synovial membrane, which is increased in inflammatory conditions, such as rheumatoid arthritis and infection, as well as in the setting of trauma or previous surgery. Factors affecting passage of contrast material between the blood vessels and synovial fluid include a pressure differential between these spaces and the viscosity of the intra-articular fluid. Effusions under tension or those with fluid of increased viscosity (eg, hemorrhagic or purulent material) result in a decreased rate of contrast diffusion into the joint. Other factors that can lead to suboptimal I-MRA include lack of joint effusion, synovial fibrosis, premature scanning time, or extravasation.
Increasing the dose of contrast material administered intravenously may increase the diffusion gradient, but has been shown to have a limited effect. Other methods of promoting blood flow to the joint, including exercise, have been used. When a traditional technique is used, a delay of 15 minutes is sufficient. In the presence of a tense or viscous joint effusion, delay times should be increased.
With I-MRA, there can be enhancement of vessels and extra-articular structures, including synovial lined spaces such as tendon sheaths and bursae. Another potential drawback of the method is the lack of adequate capsular distention.
For both D-MRA and I-MRA, the subsequent MR imaging protocol usually consists of T1-weighted fat-suppressed sequences in various planes as well as at least 1 fluid-sensitive fat-suppressed sequence for detection of marrow edema or extra-articular fluid collections. T1-weighted imaging without fat suppression may also be used to capitalize on the signal of the Gd solution and allow for superior contrast in areas delineated by high signal fat.
With respect to clinical performance, D-MRA has been shown to have sensitivity and specificity for detection of labral tears in the range of 80% to 100% and 50% to 100%, respectively, regardless of tear location. Chandnani and colleagues found sensitivities for MR imaging and D-MRA of 93% and 96%, respectively, but found the D-MRA better at detecting detached labral fragments (96% vs 46%). Waldt and colleagues found the sensitivity and specificity for detection of all labral tears with D-MRA to be 88% and 91% and Magee and colleagues reported the detection of 9 labral tears in a population of 20 athletes not noted on conventional MR imaging. D-MRA has performed particularly well with respect to SLAP tears, with sensitivities of 90% to 100% reported.
With regard to the rotator cuff, D-MRA has performed well with respect to full-thickness tears with sensitivities close to 100%. D-MRA has also proved more accurate in the detection of partial-thickness undersurface tears of the supraspinatus, with sensitivities and specificities of 80% to 84% and 96% to 97%, respectively.
D-MRA is believed to be particularly useful in the postoperative patient. Probyn and colleagues studied a population of 40 patients with recurrent instability after previous capsular repair. Their results indicated sensitivity and specificity in diagnosis of labral tears of 96.2% and 81.8%, and in detecting rotator cuff injury of 94.1% and 81.8%, respectively.
Additional benefits that have been reported for D-MRA include better depiction of the structures of the rotator interval and accurate depiction of lesions involving the proximal biceps tendon.
There are not so many reports addressing the clinical efficacy of I-MRA. Wallny and colleagues reported sensitivity and specificity in the diagnosis of labral injuries of 90% and 89%, respectively, compared with 79% and 67% for noncontrast MR imaging. Dinauer and colleagues compared I-MRA with MR imaging with respect to superior labral tears and found it to be more sensitive (84%–91% vs 66%–85%) but less specific (58%–71% vs 75%–83%), with a slightly improved overall accuracy (78%–86% vs 70%–83%). Yagci and colleagues reported sensitivity and specificity for detection of all rotator cuff tears at I-MRA as 100% and 77.8% to 88.9%, respectively, compared with 73.3% to 80% and 66.7% to 88.9% for MR imaging.
A search of the literature revealed only 1 direct comparison between D-MRA and I-MRA of the shoulder. The investigators found no statistically significant difference between the 2 modalities in the evaluation of tears of the labrum and rotator cuff.
The increased use of 3-T imaging has raised the question of whether arthrography is necessary at higher field strengths. Magee retrospectively evaluated 150 conventional MR imaging and D-MRA examinations at 3-T in the same patients. Using arthroscopy as the gold standard, Magee found that D-MRA showed a statistically significant ( P <.05) improvement in sensitivity for detection of partial articular-sided supraspinatus tears, anterior labral tears, and SLAP tears. Major and colleagues compared conventional MR imaging and D-MRA at 3-T with arthroscopy for detection of labral tears in 22 patients and found a sensitivity of 67% and 83% for the MR imaging and D-MRA, respectively.
To inject or not to inject
The Arthrography Question
Over time, it has become the standard of practice at many imaging centers to request MR arthrographic examinations, particularly in the postoperative patient or when evaluating for undersurface tears of the rotator cuff as well as when the presence of intra-articular bodies and lesions of the glenoid cartilage and labroligamentous structures is suspected. Arthrography can be performed using direct or indirect techniques.
Direct MR arthrography (D-MRA) of the shoulder is an invasive procedure that is well tolerated by most patients. It involves the injection of a contrast solution into the shoulder joint to distend the capsule and outline the intra-articular structures, thereby improving their delineation and evaluation at subsequent MR imaging ( Fig. 3 ).
Most arthrographic examinations involve the injection of dilute gadolinium (Gd) solution in a concentration of 1 to 2 mmol/L. Needle placement for intra-articular contrast injection is usually achieved with fluoroscopic or sonographic guidance. Iodinated contrast can be included in the solution to confirm needle placement and confirm an intra-articular injection. Many radiologists choose an anterior approach for evaluation of suspected lesions of the posterior labroligamentous structures and a posterior approach when the symptoms point to involvement of the anterior labrum and capsule. This strategy is used to prevent inadvertent extravasation injection of contrast material, thus obscuring important findings. The rotator interval approach has been advocated by others as an alternative anterior mode of access, resulting in a lower probability of injury to key intra-articular structures. Ultrasonography has been used to guide both posterior and rotator interval approaches.
Indirect MR arthrography (I-MRA) is based on the principle that intravenous contrast material diffuses into the joint space over time, producing an arthrographic effect. In I-MRA, Gd-based contrast in a concentration of 0.1 mmol/kg is injected intravenously and MR imaging is performed after a delay. Intravenous Gd diffuses from the capillary bed into the interstitial space of the synovium and then leaks into the joint space. The arthrographic effect is dependent on the permeability of the synovial membrane, which is increased in inflammatory conditions, such as rheumatoid arthritis and infection, as well as in the setting of trauma or previous surgery. Factors affecting passage of contrast material between the blood vessels and synovial fluid include a pressure differential between these spaces and the viscosity of the intra-articular fluid. Effusions under tension or those with fluid of increased viscosity (eg, hemorrhagic or purulent material) result in a decreased rate of contrast diffusion into the joint. Other factors that can lead to suboptimal I-MRA include lack of joint effusion, synovial fibrosis, premature scanning time, or extravasation.
Increasing the dose of contrast material administered intravenously may increase the diffusion gradient, but has been shown to have a limited effect. Other methods of promoting blood flow to the joint, including exercise, have been used. When a traditional technique is used, a delay of 15 minutes is sufficient. In the presence of a tense or viscous joint effusion, delay times should be increased.
With I-MRA, there can be enhancement of vessels and extra-articular structures, including synovial lined spaces such as tendon sheaths and bursae. Another potential drawback of the method is the lack of adequate capsular distention.
For both D-MRA and I-MRA, the subsequent MR imaging protocol usually consists of T1-weighted fat-suppressed sequences in various planes as well as at least 1 fluid-sensitive fat-suppressed sequence for detection of marrow edema or extra-articular fluid collections. T1-weighted imaging without fat suppression may also be used to capitalize on the signal of the Gd solution and allow for superior contrast in areas delineated by high signal fat.
With respect to clinical performance, D-MRA has been shown to have sensitivity and specificity for detection of labral tears in the range of 80% to 100% and 50% to 100%, respectively, regardless of tear location. Chandnani and colleagues found sensitivities for MR imaging and D-MRA of 93% and 96%, respectively, but found the D-MRA better at detecting detached labral fragments (96% vs 46%). Waldt and colleagues found the sensitivity and specificity for detection of all labral tears with D-MRA to be 88% and 91% and Magee and colleagues reported the detection of 9 labral tears in a population of 20 athletes not noted on conventional MR imaging. D-MRA has performed particularly well with respect to SLAP tears, with sensitivities of 90% to 100% reported.
With regard to the rotator cuff, D-MRA has performed well with respect to full-thickness tears with sensitivities close to 100%. D-MRA has also proved more accurate in the detection of partial-thickness undersurface tears of the supraspinatus, with sensitivities and specificities of 80% to 84% and 96% to 97%, respectively.
D-MRA is believed to be particularly useful in the postoperative patient. Probyn and colleagues studied a population of 40 patients with recurrent instability after previous capsular repair. Their results indicated sensitivity and specificity in diagnosis of labral tears of 96.2% and 81.8%, and in detecting rotator cuff injury of 94.1% and 81.8%, respectively.
Additional benefits that have been reported for D-MRA include better depiction of the structures of the rotator interval and accurate depiction of lesions involving the proximal biceps tendon.
There are not so many reports addressing the clinical efficacy of I-MRA. Wallny and colleagues reported sensitivity and specificity in the diagnosis of labral injuries of 90% and 89%, respectively, compared with 79% and 67% for noncontrast MR imaging. Dinauer and colleagues compared I-MRA with MR imaging with respect to superior labral tears and found it to be more sensitive (84%–91% vs 66%–85%) but less specific (58%–71% vs 75%–83%), with a slightly improved overall accuracy (78%–86% vs 70%–83%). Yagci and colleagues reported sensitivity and specificity for detection of all rotator cuff tears at I-MRA as 100% and 77.8% to 88.9%, respectively, compared with 73.3% to 80% and 66.7% to 88.9% for MR imaging.
A search of the literature revealed only 1 direct comparison between D-MRA and I-MRA of the shoulder. The investigators found no statistically significant difference between the 2 modalities in the evaluation of tears of the labrum and rotator cuff.
The increased use of 3-T imaging has raised the question of whether arthrography is necessary at higher field strengths. Magee retrospectively evaluated 150 conventional MR imaging and D-MRA examinations at 3-T in the same patients. Using arthroscopy as the gold standard, Magee found that D-MRA showed a statistically significant ( P <.05) improvement in sensitivity for detection of partial articular-sided supraspinatus tears, anterior labral tears, and SLAP tears. Major and colleagues compared conventional MR imaging and D-MRA at 3-T with arthroscopy for detection of labral tears in 22 patients and found a sensitivity of 67% and 83% for the MR imaging and D-MRA, respectively.
Putting a new twist on things
Novel Imaging Positions
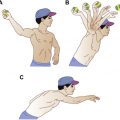
The use of various shoulder positions at MR imaging has been extensively discussed in the literature. These positions have been used for the most part in conjunction with MR arthrography because there seems to be an additive effect with respect to displacing otherwise occult labral tears away from the glenoid rim. The abducted externally rotated (ABER) position ( Fig. 4 ) has been shown to place the anterior band of the inferior glenohumeral ligament under tension, facilitating inspection of the anteroinferior capsulolabral complex. Cvitanic and colleagues retrospectively assessed the integrity of the anterior glenohumeral ligament in 256 patients using both conventional axial and ABER positions at D-MRA at 1.5-T and correlated the results with findings at surgery. These investigators found a sensitivity and specificity of 89% and 95% for the ABER view compared with 48% and 91% for the conventional positions, with an even greater sensitivity and specificity of 96% and 97% when both were used. Borrero and colleagues studied the usefulness of the ABER position at D-MRA for the detection of a posterosuperior labral peel back injury, an injury described in the overhead athlete, and found a sensitivity of 73% and specificity of 100%. Sugimoto and colleagues reported the usefulness of the ABER view at D-MRA in showing detachment of the anteroinferior capsular structures in postoperative patients.