Testicular Carcinoma
Todd M. Blodgett, MD
Alex Ryan, MD
Carl Fuhrman, MD
Key Facts
Terminology
Germ cell tumors (GCT)
Non-germ cell tumors
Gonadal stromal tumors
Interstitial cell tumors
Sex cord tumors
Imaging Findings
CT or MR for initial staging
FDG PET/CT: Therapeutic response; restaging
For seminoma, sensitivity/specificity of FDG PET are 100% and 80%, of CT are 74% and 70%
FDG PET demonstrates PPV and NPV of 91% and 62% in differentiating tumor from non-tumor lesions in patients with non-seminomatous GCT
FDG PET is the modality of choice to determine therapeutic response/restaging in malignant germ cell tumors
Ultrasonography to localize mass and determine internal structure
Top Differential Diagnoses
Epidermoid Cyst
Lymphoma, Leukemia, Metastases
Focal Orchitis
Diagnostic Checklist
US for primary diagnosis
CT or MR for initial staging
FDG PET/CT for therapeutic response/restaging
Testicular neoplasms may not be FDG avid
May lead to false negative PET; always correlate with CT
TERMINOLOGY
Abbreviations and Synonyms
Germ cell tumors (GCT): 95% of testicular carcinomas
Non-germ cell tumors also referred to as
Gonadal stromal tumors
Interstitial cell tumors
Sex cord tumors
Definitions
Germ cell tumors (GCT): Malignancy arising from germ cell elements
Seminomas
Teratoma/teratocarcinoma (embryonal cell)
Choriocarcinoma
Non-germ cell tumors: Neoplasm arising from non-germ cell elements
Leydig cell tumors (LCT): From interstitial cells
Sertoli cell tumors (SCT): From sustentacular cells lining seminiferous tubules
Granulosa cell tumors: Rare, benign tumors
Gonadoblastomas: Contain both stromal and germ cell elements
IMAGING FINDINGS
General Features
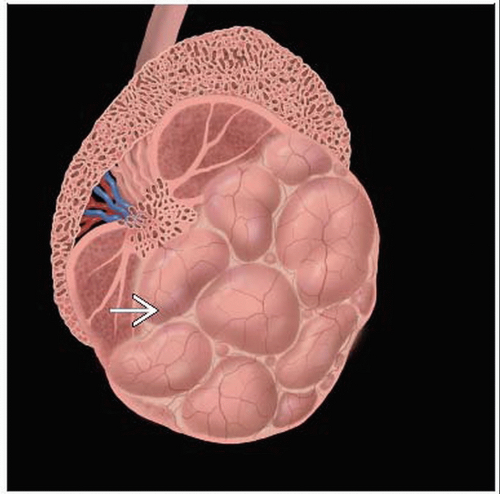
Best diagnostic clue: Palpable, intratesticular, homogeneous or mixed consistency hypoechoic mass on US
Location
Germ cell tumors
Local: Testis, epididymis, spermatic cord
Regional: Retroperitoneal lymph nodes
Distant: Supradiaphragmatic nodes or visceral sites
Most common site of recurrence is retroperitoneum
Non-germ cell tumors: 90% local (benign), 10% metastasize
Rarely bilateral
Size: > 5 cm indicates high stage disease
Morphology
Imaging Recommendations
Best imaging tool
Ultrasonography to localize mass and determine internal structure
CT or MR for initial staging
For stage I, GCT CXR may be used at diagnosis and for follow-up
FDG PET/CT: Restaging and response to therapy
Protocol advice
High frequency linear array US including both testes
CT Findings
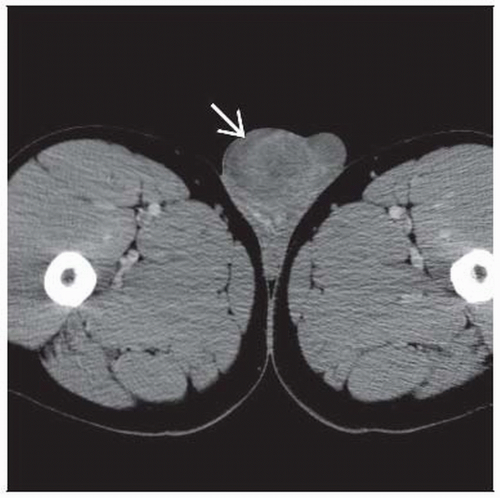
CT indicated for staging of metastasis in retroperitoneum, lymph nodes, and mediastinum/lungs
Insensitive for undiagnosed testicular lesions
Especially useful when metastatic disease in thorax is suspected
Lymphoma and metastatic testicular cancer may have similar appearance
Obtain tissue sample from abnormal testicle
Lymph nodes
Typical locations for malignant involvement include left renal hilus and retrocaval area
Low attenuation, poorly enhancing nodes in these regions suspicious even when small
Residual low attenuation masses after treatment
Lesions > 3 cm 4 weeks after chemotherapy have 30% chance of harboring viable tumor
Surgical resection recommended > 3 cm
Recurrence most common in retroperitoneum; CT may identify “growing teratoma” syndrome
Nuclear Medicine Findings
Initial diagnosis
Limited data on FDG PET evaluation of malignant non-germ cell tumors is available
Sensitivity/specificity for seminoma
FDG PET: 100% and 80%
CT: 74% and 70%
SUV > 3 used as cutoff for suspicion of malignancy in primary testicular tumor
Staging
For initial staging of testicular germ cell tumors, FDG PET offers no statistical advantage over CT
FDG PET demonstrates positive predictive value (PPV) and negative predictive value (NPV) of 91% and 62% in differentiating tumor from non-tumor lesions in patients with non-seminomatous GCT
Negative FDG PET studies may not exclude presence of disease (due largely to presence of teratoma)
Residual masses with negative FDG PET usually still require surgical resection
Additional FDG PET exams are without benefit in cases of elevated tumor markers and tumor progression diagnosed by CT
FDG PET useful for identifying stage IIA in clinical stage I non-seminomatous GCT patients
Restaging
Anterior mediastinum: Normal thymic uptake may be mistaken for disease recurrence
Tumor marker elevation in the absence of CT changes should prompt PET scan for possibility of salvage surgery
Overall, FDG PET is the best predictor of viable seminoma in residual masses after chemotherapy
Also useful in non-seminomatous GCT patients
Masses with residual malignancy may appear negative on PET 10-14 days after chemotherapy (“stunned” tumor)
Post-therapy non-seminomatous GCT
Difficult to differentiate mature teratoma from necrosis or scar
Both entities have low FDG uptake
Non-standard dynamic imaging: Kinetic parameter for FDG transport in mature teratoma higher than those for necrosis/scar
Longitudinal follow-up required for late relapse patients, even with negative FDG PET scan
In complicated multiple-relapse seminoma patients, use of FDG PET has been shown to change decision on therapy in 57% of cases
Response to therapy
FDG PET is the modality of choice for determining therapeutic response/restaging in malignant germ cell tumors
Best predictor of viable residual seminoma in post-chemotherapy masses
Negative FDG PET excludes presence of viable tumor for lesions > 3 cm
Sensitivity 80%, specificity 100%, PPV 100%, NPV 96%
Compares to 74%, 70%, 34%, 92% for CT
Lesions < 3 cm: Sensitivity/specificity 25% and 100%
FDG PET predicts response to therapy of germ cell tumors
Mean SUV of nonresponders: 2.7
Mean SUV of responders: 1.8
PPV/NPV of FDG PET in patients with raised tumor markers and negative CT: 92% and 50%
PPV/NPV for patients with residual mass: 96% and 90%
DIFFERENTIAL DIAGNOSIS
Focal Orchitis
FDG uptake due to infection/inflammation
Presents with pain/tenderness