Clinical Presentation
The patient is a 42-year-old man who over the course of the past year has been aware of increasing difficulty with bladder control. He describes marked urgency and frequency of micturition and on some occasions has been incontinent. He has also, at times, noticed that voiding may be imperfect and he may struggle to initiate micturition. There is also a long history of episodic fecal incontinence. This dates to childhood and the incontinence tends to occur only when he has diarrhea. There is also a long history of back pain. More recently, he describes episodic sensory symptoms. There are times when he has noticed a feeling of the outer aspects of the feet “going to sleep.” He has not been aware of atrophy of leg muscles but has always noticed that his calve musculature has been poorly developed, this more obvious on the right side. Leg weakness has not been a prominent feature, although his gait appears to have deteriorated over time, this attributed to unequal length of his legs. There are no symptoms in his upper limbs.
Imaging Presentation
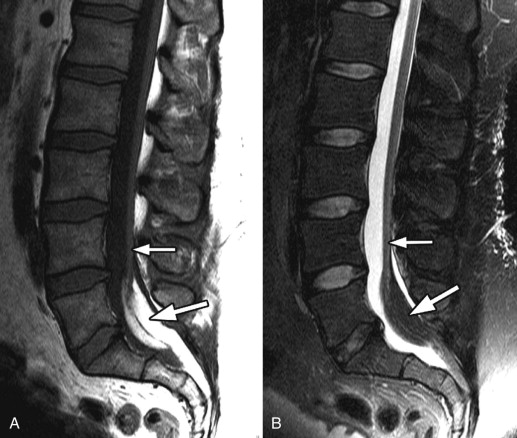
Sagittal T1-weighted and fat-saturated, T2-weighted images demonstrate a low-lying spinal cord terminating and tethered into a large region of increased T1 signal intensity/decreased fat-saturated T2 signal intensity compatible with fat ( Fig. 78-1 ) .
Imaging Presentation
Sagittal T1-weighted and fat-saturated, T2-weighted images demonstrate a low-lying spinal cord terminating and tethered into a large region of increased T1 signal intensity/decreased fat-saturated T2 signal intensity compatible with fat ( Fig. 78-1 ) .

Discussion
The tethered cord syndrome (TCS), also known as tight filum terminale syndrome is a clinical entity by which signs and symptoms are caused by excessive tension on the spinal cord. The majority of cases of tethered cord are related to spinal dysraphism. The concept of the tethered cord has been around for over 150 years; however, it was not until 1953 when Garceau attributed the orthopedic spinal deformities and neurologic dysfunction of three patients to tension on the conus medullaris from a thickened filum terminale, which was found at surgery. All three patients had good clinical results after sectioning of the filum terminale. In 1976, Hoffman coined the phrase tethered spinal cord in patients with an abnormally low conus medullaris and a filum terminale of 2 mm or more in diameter.
The spinal cord forms through three complex processes: neurulation, canalization, and retrogressive differentiation. Retrograde differentiation results in the formation of the filum terminale, cauda equina, and the relative ascension of the conus medullaris in relation to the vertebra column. As the conus ascends because of disproportionate vertebral column to spinal cord growth, the filum terminale elongates and the nerve roots that must exit inferior to the conus elongate in order to pass through their respective foramen, thus forming the cauda equina. There has been debate as to what is considered the normal level of the conus medullaris and when it attains that position. Barson demonstrated in an anatomic study that the conus medullaris is at approximately the L2-L3 interspace at full-term birth and ascends to the L1-L2 level by approximately 2 months of age. Beek and colleagues demonstrated, using ultrasound, that the conus lies at L1-L2 by 40 weeks of gestation. Other investigators have the conus terminating between the T10-T11 interspace and mid-body of L4, with all studies accepting that a conus at or above the L2-L3 level is normal. Kesler and colleagues evaluated the level of the conus medullaris in 100 children after whole-spine magnetic resonance (MR) imaging. This was the first study to count vertebral levels from C2. All other studies counted from the lumbosacral junction up and therefore did not account for transitional vertebrae and did not assess rib-bearing vertebrae. Kesler’s study demonstrated that the conus medullaris terminates most commonly at the L1-L2 interspace and in the absence of cord tethering, never ends below the mid-body of L2.
The filum terminale’s functions are believed to be to fixate, stabilize, and buffer the distal spinal cord from both normal and abnormal cephalic and caudal traction. The filum terminale is a viscoelastic band that allows slight upward and downward movement of the conus medullaris during flexion and extension of the spine. Mechanical causes of cord tethering can arise from thickening of the filum terminale attached to the spinal cord or any other inelastic structures including a fatty filum terminale, lipomas (see Fig. 78-1 ), epidermoid tumors, myelomeningoceles ( Fig. 78-2 ) , lipomyelomeningoceles, granulation tissue, or osseous or fibrous septum ( Fig. 78-3 ) . It is further believed that the inelasticity of the filum terminale causes failure of “ascension” of the conus medullaris to its normal position. The hypothesis is that if there is loss of the viscoelastic properties of the filum terminale, that caudal tension and traction can cause undue stress on the conus medullaris, resulting in TCS. Yamada and colleagues demonstrated that in patients with TCS, the filum terminale elongated by only 10% when stretched, and in those without TCS, the filum terminale elongated by more than 50%. This shows that there is less reserve in patients with TCS and that their spinal cords are preloaded with additional tension so that minor additional stretching can cause severe and permanent damage. Furthermore, Yamada and colleagues demonstrated that caudal traction of the distal cord caused impairment in oxidative metabolism with a corresponding reduction in spinal cord blood flow resulting in hypoxia. There are clinicians who believe that the TCS can occur in patients with normally located distal cords and that the tethering element may still restrict movement and cause traction on the conus.