Abstract
Tetralogy of Fallot (TOF) is one of the most frequently occurring conotruncal anomalies. It is classically overlooked if the visualization of the outflow tracts is not included in routine cardiac examination. There is a high association with chromosomal defects and extracardiac anomalies. Overall, TOF diagnosed prenatally has a poor prognosis because of a high association with other anomalies. The prognosis in isolated TOF depends on the degree of pulmonary disease, but in pulmonary stenosis it is generally good.
Keywords
congenital heart defect, conotruncal anomaly, tetralogy of Fallot
Disease
Definition
In TOF, there is an anterior-superior and leftward displacement of the outlet septum in relation to the trabecular interventricular septum. It is characterized by an outlet, perimembranous ventricular septal defect (VSD), an overriding aorta over the infundibular septum, and a variable degree of right ventricular outflow tract obstruction, classically in the subpulmonary (infundibular) region ( and ). Right ventricular hypertrophy is uncommon in fetal life because of the variable degree of right ventricular tract obstruction and the relieving effect of the physiologic right-to-left fetal circulatory shunt.
Prevalence and Epidemiology
TOF affects 0.5 : 1000 to 1 : 1000 newborns and is the most common cyanotic CHD in childhood. It accounts for 10% of all CHDs at birth, but only 3% to 6% of prenatally diagnosed CHDs.
Etiology and Pathophysiology
The etiology is multifactorial. TOF has been associated with untreated maternal diabetes, phenylketonuria, and intake of retinoic acid. Chromosomal anomalies occur in 30% of cases and include trisomies 21, 18, and 13 and 22q11 microdeletion, especially in pulmonary atresia and absent pulmonary valve syndrome (APVS, 40% to 50% of cases). Extracardiac anomalies, in particular abdominal and thoracic abnormalities, occur in 25% to 30% of cases. Recurrence risk is 3%.
Prognosis depends on the type of TOF, which is classified based on the pulmonary defect:
- •
Pulmonary stenosis (approximately 60%) is the most frequent prenatal form of TOF.
- •
Pulmonary atresia (approximately 30% to 35%): the degree of pulmonary obstruction can be progressive during fetal life, occasionally evolving from stenosis to atresia.
- •
Absent pulmonary valve (5% to 10%): there is severe dilatation of the pulmonary trunk and branches due to the to-and-fro flow across the absent valve. It is usually associated with agenesis of the ductus arteriosus.
Manifestations of Disease
Clinical Presentation
TOF is usually asymptomatic during fetal life. Postnatal manifestations depend on the severity of the right outflow tract obstruction. Forms with pulmonary stenosis are normally asymptomatic and manifest with a murmur or increasing cyanosis during the first month of life. In pulmonary atresia, there is severe cyanosis at birth, requiring a systemic-to-pulmonary shunt after birth.
Imaging Technique and Findings
Ultrasound.
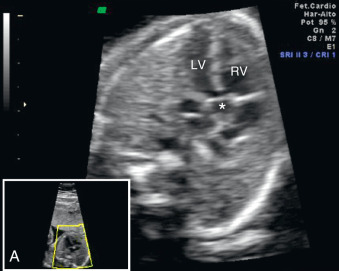
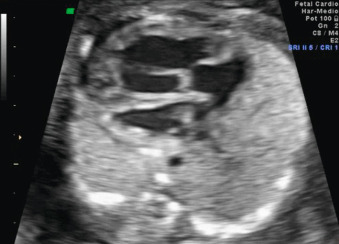
The four-chamber view on ultrasound (US) is typically normal ( Fig. 85.1 ). In some cases, there is levorotation of the heart axis, which should raise suspicion of TOF ( Fig. 85.2 ). Cases with APVS can also be associated with cardiomegaly ( Fig. 85.3 ).


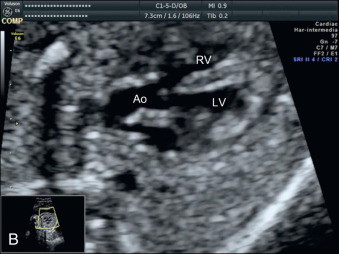
The five-chamber view or long-axis view is critical for the diagnosis. The typical sign of TOF is a perimembranous subaortic VSD with an overriding aorta. Continuity of the infundibular septum with the aorta is lost, and the aorta arises from both ventricles ( Fig. 85.4 ), which is seen with color Doppler as a typical Y sign ( Fig. 85.5 ). Overflow through the aortic root normally causes enlargement of the ascending aorta.