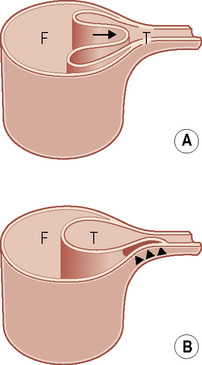
• This occurs as a result of a rapid deceleration injury generating shearing forces at the aortic isthmus • Classification of aortic injuries: (A) intimal haemorrhage • Contributory factors: tethering by the ligamentum arteriosum • 70% of patients die at the scene of the trauma due to a complete aortic rupture • There should be a high index of suspicion with: road traffic accidents (RTAs) at speeds greater than 30mph (particularly involving unrestrained occupants of vehicles or pedestrians involved in an RTA) This is rarely normal with a traumatic aortic rupture • Mediastinal widening: this can be problematical as in the trauma setting the patient is usually imaged in the supine position • Blurring of the aortic arch contours • Filling-in of the aortopulmonary window • A left apical pleural cap: this is due to an extrapleural haematoma • Tracheal or nasogastric tube deviation: to the right • Depression of the left mainstem bronchus • Widening of the right paratracheal stripe (or the presence of paraspinal lines) • Direct signs: pseudoaneurysm formation • Indirect sign: periaortic mediastinal haematoma (haematoma that is not adjacent to the aorta and is without direct signs of an aortic injury can be ascribed to mediastinal venous bleeding) • Minimal aortic injury: this is represented by a small intramural haematoma or an intimal thrombus – these can be treated conservatively • A false-negative result: poor contrast enhancement • A false-positive result: the presence of severe atheroma or a ductus diverticulum • Aortic isthmus: this is the junction between the relatively mobile arch and the relatively fixed descending thoracic aorta • Treatment: traditionally this has been a surgical repair but endovascular stenting is now used with increasing frequency • A dissection is initiated by an intimal tear – this allows blood to penetrate into and split the medial layer in a longitudinal fashion (the cleavage plane is produced between the inner ⅔ and outer ⅓ of the media) • Arterial pressure extends the dissection for a variable distal distance, producing a false channel (or lumen) • The ‘false’ lumen is separated from the ‘true’ lumen by an intimomedial flap • The aetiology is frequently unknown (most dissections are spontaneous) • Intramural haematoma: this results from a hypertensive rupture of the vasa vasorum within the aortic media • Dynamic obstruction: this affects vessels arising from the true lumen – bowing of the dissection flap across the true lumen can cause collapse of the true lumen and restriction of branch vessel ostial flow • Static obstruction: this results from extension of the dissection into a branch vessel without a re-entry point • Chest (± back pain) • A dissection commonly occurs in middle-aged to elderly hypertensive patients Classification systems for aortic dissection
The aorta
AORTIC RUPTURE
TRAUMATIC AORTIC RUPTURE
DEFINITION
 other mechanisms of injury include an AP compression force displacing the heart to the left (a torsion stress)
other mechanisms of injury include an AP compression force displacing the heart to the left (a torsion stress)
 Incomplete rupture: the adventitia remains intact (maintaining the aortic integrity) in the majority of survivors
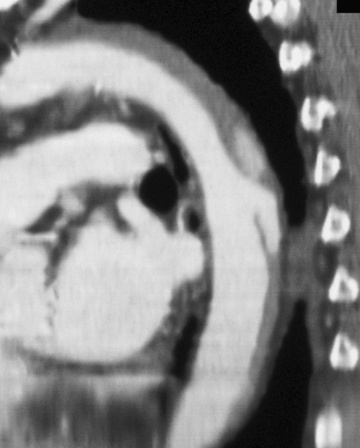
Incomplete rupture: the adventitia remains intact (maintaining the aortic integrity) in the majority of survivors  the saccular outpouching that develops is known as a pseudoaneurysm
the saccular outpouching that develops is known as a pseudoaneurysm
 Complete rupture: the adventitia is disrupted and is normally associated with mediastinal haemorrhage
Complete rupture: the adventitia is disrupted and is normally associated with mediastinal haemorrhage  if the patient survives it may progress to apical pleural capping or a haemothorax
if the patient survives it may progress to apical pleural capping or a haemothorax
 (B) intimal haemorrhage with a laceration
(B) intimal haemorrhage with a laceration  (C) medial laceration
(C) medial laceration  (D) complete laceration
(D) complete laceration  (E) false aneurysm formation
(E) false aneurysm formation  (E) periaortic haemorrhage
(E) periaortic haemorrhage
 an ‘osseous pinch’: compression of the heart and aorta between the anterior chest wall and the thoracic spine during impact
an ‘osseous pinch’: compression of the heart and aorta between the anterior chest wall and the thoracic spine during impact
CLINICAL PRESENTATION
 falls from a height of greater than 10ft (3m)
falls from a height of greater than 10ft (3m)  severe crush injuries to the chest
severe crush injuries to the chest
RADIOLOGICAL FEATURES
CXR
 the signs include:
the signs include:
 signs include:
signs include:
 A mediastinal width above the level of the carina of ≥ 8cm
A mediastinal width above the level of the carina of ≥ 8cm
 The mediastinum forms > 25% of the width of the chest above the level of the carina (i.e. a mediastinal-to-cardiac ratio of 0.25)
The mediastinum forms > 25% of the width of the chest above the level of the carina (i.e. a mediastinal-to-cardiac ratio of 0.25)
 NB: a subjective impression of a wide mediastinum should override these measurements
NB: a subjective impression of a wide mediastinum should override these measurements
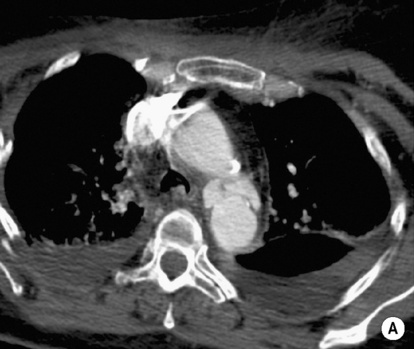
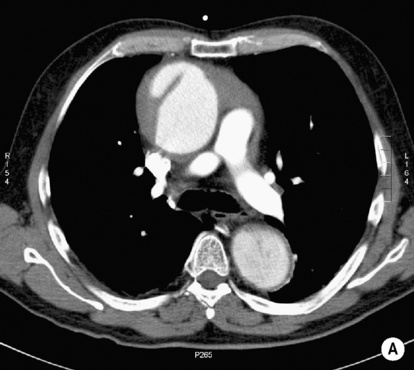
CT
 an intimal flap
an intimal flap  an intramural haematoma
an intramural haematoma  contrast extravasation
contrast extravasation
 partial volume effects
partial volume effects
 young patients with residual thymic tissue
young patients with residual thymic tissue
PEARLS
 it is located just distal to the left subclavian artery and at the site of the ligamentum arteriosum
it is located just distal to the left subclavian artery and at the site of the ligamentum arteriosum
 In clinical series 90% of ruptures occur at the isthmus
In clinical series 90% of ruptures occur at the isthmus
 In autopsy series ascending aortic injuries account for 20–25% of cases
In autopsy series ascending aortic injuries account for 20–25% of cases  as these are usually rapidly fatal (due to exsanguination, haemopericardium, and cardiac tamponade) they only account for 5% of clinical cases
as these are usually rapidly fatal (due to exsanguination, haemopericardium, and cardiac tamponade) they only account for 5% of clinical cases
 stenting requires at least 15mm of aorta proximal to the injury to achieve an adequate seal
stenting requires at least 15mm of aorta proximal to the injury to achieve an adequate seal
AORTIC DISSECTION
AORTIC DISSECTION
DEFINITION
 this can also sometimes occur proximal to the entry tear
this can also sometimes occur proximal to the entry tear
 an additional communication between the 2 lumens can be caused by either shear forces producing re-entry tears in the flap, or by an avulsion of the flap attachment at a branch vessel origin (producing a natural fenestration within the flap)
an additional communication between the 2 lumens can be caused by either shear forces producing re-entry tears in the flap, or by an avulsion of the flap attachment at a branch vessel origin (producing a natural fenestration within the flap)
 The ‘false’ lumen is prone to aneurysmal dilatation due to the reduced elastic tissue within its wall
The ‘false’ lumen is prone to aneurysmal dilatation due to the reduced elastic tissue within its wall
 almost all will originate within the thoracic aorta with extension into the abdominal aorta
almost all will originate within the thoracic aorta with extension into the abdominal aorta  many dissections can occur in non-aneurysmal aortas
many dissections can occur in non-aneurysmal aortas
Potential dissection precursors
 the haematoma may remain localized or propagate and rupture through the intima
the haematoma may remain localized or propagate and rupture through the intima
Mechanisms of branch vessel ischaemia
 the increased pressure or thrombus formation within the branch vessel false lumen produces a focal stenosis (± end-organ ischaemia)
the increased pressure or thrombus formation within the branch vessel false lumen produces a focal stenosis (± end-organ ischaemia)
CLINICAL PRESENTATION
 branch vessel occlusion can lead to neurological deficits as well as blood pressure differences between the extremities (which may ultimately become ischaemic)
branch vessel occlusion can lead to neurological deficits as well as blood pressure differences between the extremities (which may ultimately become ischaemic)
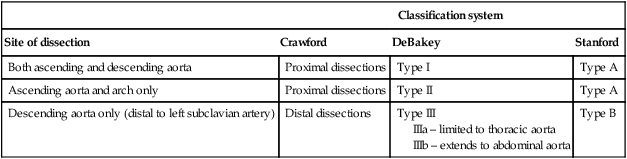
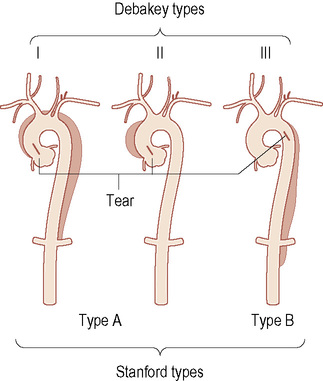
Classification system
Site of dissection
Crawford
DeBakey
Stanford
Both ascending and descending aorta
Proximal dissections
Type I
Type A
Ascending aorta and arch only
Proximal dissections
Type II
Type A
Descending aorta only (distal to left subclavian artery)
Distal dissections
Type III
IIIa – limited to thoracic aorta
IIIb – extends to abdominal aorta
Type B
AORTIC DISSECTION
AORTIC DISSECTION
RADIOLOGICAL FEATURES

 images can be degraded by streak artefact from the shoulders
images can be degraded by streak artefact from the shoulders pseudoaneurysm formation
pseudoaneurysm formation  the presence of an intimal flap
the presence of an intimal flap  aortic dissection
aortic dissection  pseudocoarctation (uncommon)
pseudocoarctation (uncommon) severe aortic atheroma
severe aortic atheroma  double densities from overlapping adjacent vessels
double densities from overlapping adjacent vessels




 aortitis
aortitis  a bicuspid aortic valve
a bicuspid aortic valve  pregnancy
pregnancy  blunt chest trauma
blunt chest trauma  advancing age (± hypertension)
advancing age (± hypertension)  connective tissue disorders (e.g. Marfan’s and Ehlers–Danlos syndromes)
connective tissue disorders (e.g. Marfan’s and Ehlers–Danlos syndromes)

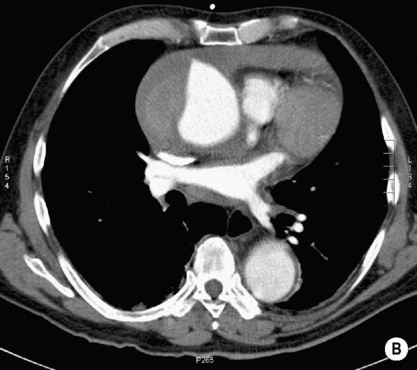
 the dissection flap may be visible as a linear track of high attenuation (from intimal calcification) within the aortic lumen
the dissection flap may be visible as a linear track of high attenuation (from intimal calcification) within the aortic lumen images are acquired just cephalad to the aortic arch and extend inferiorly down to the aortic bifurcation or femoral heads
images are acquired just cephalad to the aortic arch and extend inferiorly down to the aortic bifurcation or femoral heads  avoid injecting via the left arm (as this may cause a potential streak artefact across the aortic arch from the left brachiocephalic vein)
avoid injecting via the left arm (as this may cause a potential streak artefact across the aortic arch from the left brachiocephalic vein)
 posterolateral (descending aorta)
posterolateral (descending aorta)

 it requires high-speed pulse sequences
it requires high-speed pulse sequences it can localize the site of any intimal tears
it can localize the site of any intimal tears  it provides haemodynamic information on the true and false lumen flows
it provides haemodynamic information on the true and false lumen flows  it can assess the functional status of the aortic valve and coronary arterial involvement for type A dissections
it can assess the functional status of the aortic valve and coronary arterial involvement for type A dissections it can demonstrate the entry tear and the extent of the dissection
it can demonstrate the entry tear and the extent of the dissection  it can differentiate between a true and false lumen
it can differentiate between a true and false lumen  it can demonstrate dynamic obstruction
it can demonstrate dynamic obstruction






