Table 5.1 • Major Fetal Abnormalities That can Potentially be Easily Identified on First Trimester Ultrasound | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
fetal malformations in early gestation. Undoubtedly, as new information comes about and with technological advances in ultrasound imaging, the approach to the detailed first trimester ultrasound examination will evolve over time.
Table 5.2 • Diagnosis of Fetal Anomalies at 11 to 13 Weeks Scan, after Excluding Detected Aneuploidies (N = 44,859) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
Major Malformation, Clearly Visible: The malformation is easily recognized during a routine first trimester ultrasound or an ultrasound performed for NT measurement, even with limited skills of the examiner.1,13 Table 5.1 summarizes some of the major anomalies that are clearly visible in the first trimester.
Thickened Nuchal Translucency: Many fetal malformations have been reported in association with thickened NT in the presence or absence of chromosomal aneuploidy. When a thickened NT is encountered, invasive genetic testing is typically offered along with an ultrasound examination of the fetus. This approach has led to the first trimester diagnosis of complex cardiac, brain, skeletal, gastrointestinal, and genitourinary anomalies as presented in various chapters in this book. On occasions, the associated fetal malformation is not seen in the first trimester but rather detected in the second trimester or even after birth and the relationship with an increased NT is thus assumed. Table 9.3 in Chapter 9 summarizes fetal malformations that are known to be associated with thickened NT.
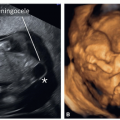
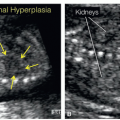
Pregnancies at High Risk for Fetal Malformations: When the pregnancy is at high risk for fetal anomaly due to a prior history of an affected child or due to a known inheritance pattern of a specific malformation, a detailed ultrasound in the first trimester can identify the fetal malformation. Examples include a pregnancy with prior spina bifida, an autosomal recessive inheritance pattern identified in a prior pregnancy, or an autosomal dominant inheritance pattern present in one of the parents. The presence of subtle findings in the first trimester ultrasound can be of significance in such cases such as the presence of abnormal intracranial translucency, polydactyly, echogenic kidneys, skeletal abnormalities, and cleft lip and palate, among others. Several of these subtle findings are discussed in detail in various chapters in this book.
Detailed First Trimester Ultrasound in Low-Risk Pregnancies: The detection of fetal malformations in the first trimester can also be the result of a detailed ultrasound examination that is routinely performed beyond the 11th week of gestation.11,13,19 With increasing skills and expertise in the detailed first trimester ultrasound, sonographers and sonologists may decide to apply this approach to all first trimester pregnancies beyond the 11th week of gestation for fetal anomaly screening. The detailed first trimester ultrasound will thus be an adjunct to the second trimester ultrasound examination. It is important to note however that several limitations currently exist to the detailed first trimester ultrasound examination and it is thus important to list these limitations before its introduction.
For instance, unlike in the second trimester, bilateral renal agenesis is commonly associated with normal amniotic fluid volume in early gestation and open spina bifida does not typically display a lemon or banana sign in the first trimester as is very often seen in the second trimester of pregnancy. Other examples include the absence of hyperechogenicity or cystic changes in lung lesions in the first trimester and the lack of reliance on the abnormal cavum septi pellucidi in several central nervous system (CNS) lesions as commonly used in the second trimester ultrasound. Furthermore, fetal biometric changes and growth restriction that are commonly associated with fetal malformations do not manifest in early gestation and cannot be used as clues to the presence of associated malformations. It is important to note for all these reasons and others that the detailed first trimester ultrasound examination for fetal anatomy survey does not replace the traditional second trimester ultrasound but rather is complementary to it, especially in a high-risk pregnancy. Pregnant women should be informed of these limitations.
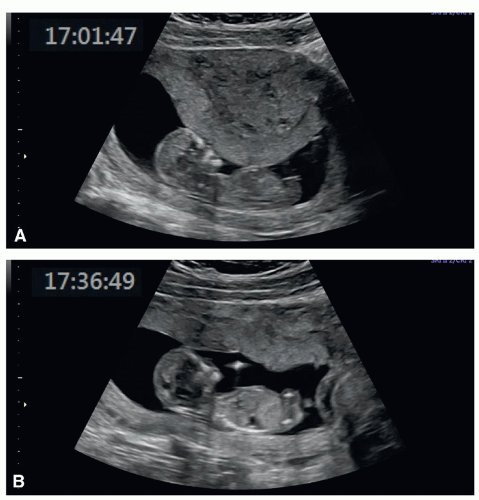
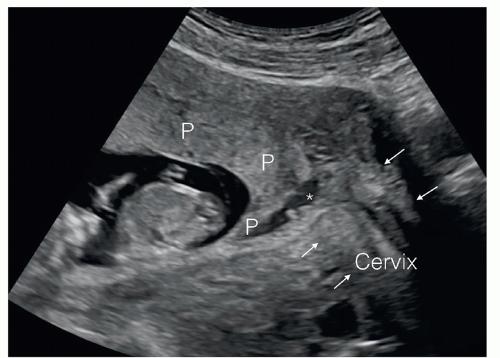
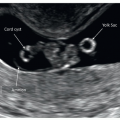
the scar is ideally assessed by transvaginal ultrasound.20 In these pregnancies the location of the gestational sac within the endometrial cavity should be noted and implantations in the lower uterine segment should raise suspicion for increased risk for placenta accreta21,22 (see Chapter 15). Furthermore, implantation of the gestational sac in the cesarean scar (cesarean scar implantation) is of significant importance given its association with placenta accreta and serious pregnancy complications.22,23 In the presence of twins or higher order multiple pregnancy, determining the chorionicity and amnionicity in the first trimester is of paramount importance. The presence and size of any significant subchorionic bleed (Fig. 5.3) should also be reported.
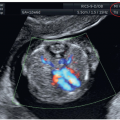
 Figure 5.3: Subchorionic hematoma (arrows) in a pregnancy at 12 weeks of gestation in a patient presenting with vaginal bleeding. See text for details. |
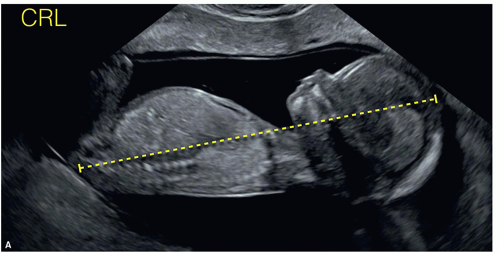
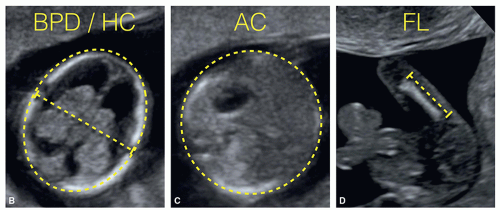
a general anatomic assessment, given that the whole fetus is commonly included in this plane (Fig. 5.5). This midsagittal plane displays several important anatomic landmarks, which are listed in Table 5.4. In this midsagittal plane, the size and proportions of the fetal head, chest, and body are subjectively assessed and the following anatomic regions are recognized: fetal facial profile and midline intracranial structures, the anterior abdominal wall, the fetal stomach, and bladder. By slightly tilting the transducer from the midline to the left and right parasagittal planes, the arms and legs can be visualized. Many of the severe fetal malformations that can be detected in the first trimester (Table 5.1) will show abnormalities in the midsagittal
plane and an in-depth evaluation of fetal anatomic regions, as described in the following sections, will help to confirm the presence or absence of other fetal abnormalities. When clinically indicated, color and pulsed Doppler interrogation of the ductus venosus is also best assessed in this midsagittal plane.
Table 5.3 • General Overview and Fetal Biometry of the Detailed First Trimester Ultrasound | ||||||
|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree