his chapter will review preoperative and postoperative imaging of elbow trauma, joint replacement procedures, and other common orthopaedic disorders for which implants are required.
his chapter will review preoperative and postoperative imaging of elbow trauma, joint replacement procedures, and other common orthopaedic disorders for which implants are required.
 Trauma
Trauma
Fractures and dislocations of the elbow can be complex and difficult to manage. This section reviews specific injuries to the distal humerus, radial head, and proximal ulna with emphasis on injuries that require orthopaedic fixation.
Distal Humeral Fractures
Supracondylar fractures are extra-articular. Most of these injuries occur in children (80%). In children, intracondylar extension and physeal injuries are uncommon. Only approximately 6% of all physeal fractures involve the distal humerus. The second most common group involves insufficiency fractures in elderly patients with osteoporotic bone. Fractures of the elbow account for 7% of adult fractures. Overall, distal humeral fractures in adults account for only 3% of all skeletal fractures. In children, most injuries are related to significant falls or high-velocity injuries such as motor vehicle accidents. In more elderly patients, simple falls result in distal humeral fractures.
The distal humerus comprises medial and lateral columns with a transverse articular surface which includes the capitellum (anterior extension of the lateral column) and trochlea (see Fig. 11-1). Multiple classification systems have been used for distal humeral fractures. Classifications are designed to deal with the difficult reconstruction of the anatomic relationships.
Pediatric supracondylar fractures may be classified by the direction of the distal fragment. These fractures are the most common elbow fracture in children (60% to 80%). Most fractures are due to extension injury (98%) (see Fig. 11-2). Flexion injuries account for only 2% of supracondylar fractures.
Lateral condylar fractures account for 15% to 17% of pediatric elbow injuries. The metaphyseal fracture may enter the joint at the junction of the captellum and trochlea or more medially through the trochlea (see Fig. 11-3).
Fractures of the medial epiccondyle do not involve the articular surface. Most of these injuries (80%) occur during adolescence and are common in throwing athletes (see Fig. 11-4). Complex condylar fractures (T and Y configurations) are rare in children and account for <1% of pediatric elbow fractures (see Fig. 11-5).
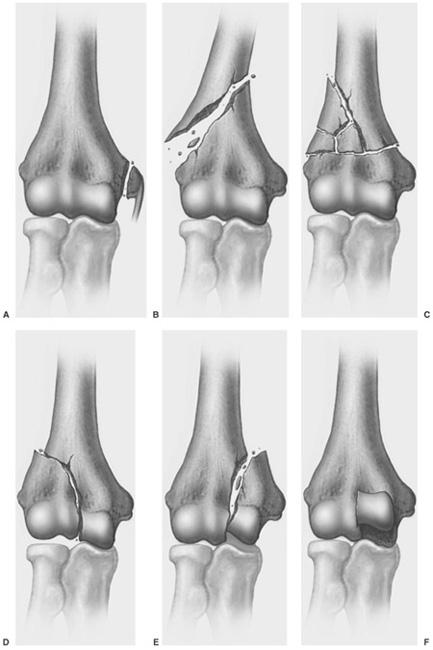
Multiple classification systems have been used for distal humeral fractures in adults. These include the Riseborough and Radin classification developed in 1969, Mehne and Matta classification, AO (Arbeitsgemeinschaft fur Osteosynthesefragen), and in 1996 the Orthopaedic Trauma Association classification (see Fig. 11-6). The last system is more complex and based on fracture location and extent (extra-articular, partial articular, and complete articular). There are three groups with three major categories and subcategories in each (see Figs. 11-7, 11-8, 11-9, 11-10 and also Fig. 11-6).
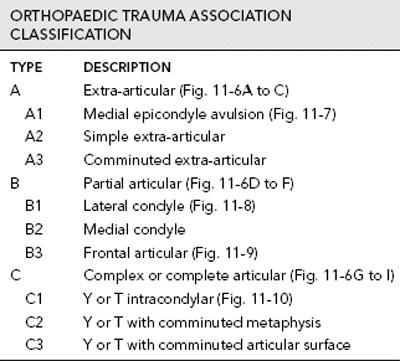
 Fig. 11-1 Anteroposterior (AP) radiograph demonstrating the medial (M) and lateral (L) columns of the distal humerus with the central articular surface bordered by the columns.
Fig. 11-1 Anteroposterior (AP) radiograph demonstrating the medial (M) and lateral (L) columns of the distal humerus with the central articular surface bordered by the columns.
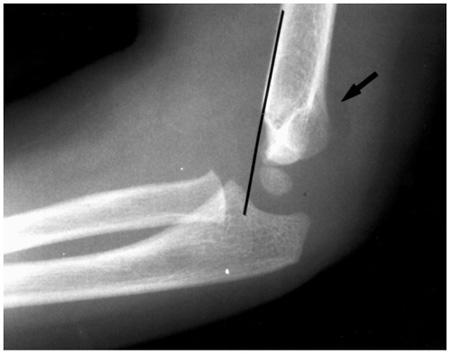
 Fig. 11-2 Supracondylar extension fracture. Lateral radiograph demonstrating posterior displacement of the capitellum in relation to the anterior humeral line. There is a posterior fat pad sign (arrow).
Fig. 11-2 Supracondylar extension fracture. Lateral radiograph demonstrating posterior displacement of the capitellum in relation to the anterior humeral line. There is a posterior fat pad sign (arrow).
SUGGESTED READING
Davies MB, Stanley D. A clinically applicable fracture classification for distal humeral fractures. J Shoulder Elbow Surg. 2006;15:602–608.
Kasser JR, Beaty JH. Supracondylar fractures of the distal humerus. In: Beaty JH, Kasser JR, eds. Rockwood and Wilkin’s fractures in children, 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2001:577–624.
Orthopaedic Trauma Association Committee on Coding and Classifications. Fractures and dislocations compendium. J Orthop Trauma. 1996;10(Suppl):12–14.
Radial Head Fractures
Radial head fractures account for 2% to 5% of all skeletal fractures, with 85% occurring in adults. In children, fractures of the metaphysis and physis are more common. Proximal radial fractures in children are most common between 8 and 12 years of age. Most fractures occur during a fall on the outstretched hand regardless of patient age.
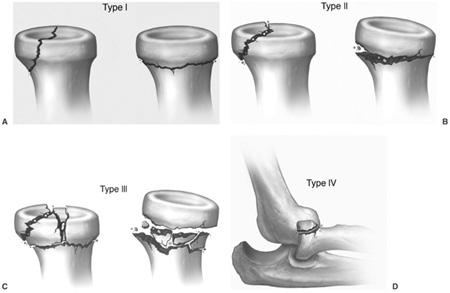
The Mason classification is commonly used for isolated radial head fractures. This system is useful for treatment planning (see Fig. 11-11).
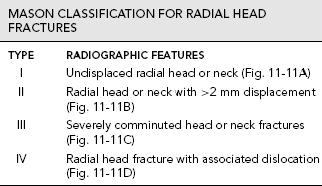
 Fig. 11-3 Lateral (A) and anteroposterior (AP) (B) radiographs demonstrating a lateral condyle fracture entering the joint at the margin of the capitellar epiphysis (arrows). 1-radial head epipysis, 2-olecranon epiphysis, 3-lateral epicondyle, 4-medial epicondyle, 5-trochlear epiphysis, 6-capitellum.
Fig. 11-3 Lateral (A) and anteroposterior (AP) (B) radiographs demonstrating a lateral condyle fracture entering the joint at the margin of the capitellar epiphysis (arrows). 1-radial head epipysis, 2-olecranon epiphysis, 3-lateral epicondyle, 4-medial epicondyle, 5-trochlear epiphysis, 6-capitellum.

 Fig. 11-4 Avulsion of the medial epicondyle. A: Anteroposterior (AP) radiograph demonstrates a displaced medial epicondylar epiphysis in a young baseball pitcher (arrow). B: AP radiograph of a different patient with the medial epicondylar epiphysis displaced into the joint (arrowhead) with widening (broken lines) of the joint space.
Fig. 11-4 Avulsion of the medial epicondyle. A: Anteroposterior (AP) radiograph demonstrates a displaced medial epicondylar epiphysis in a young baseball pitcher (arrow). B: AP radiograph of a different patient with the medial epicondylar epiphysis displaced into the joint (arrowhead) with widening (broken lines) of the joint space.
 Fig. 11-5 Anteroposterior (AP) radiograph demonstrating a complex Y intracondylar fracture (arrows).
Fig. 11-5 Anteroposterior (AP) radiograph demonstrating a complex Y intracondylar fracture (arrows).
Radial head and neck fractures are commonly associated with other elbow fractures including coronoid, olecranon, and capitellar injuries. Up to 50% of capitellar fractures occur in association with radial head fractures. Associated ligament and neurovascular injuries are also common. Monteggia fractures classically demonstrate radial head dislocation with the proximal ulnar fracture. However, associated radial head and coronoid fractures are not uncommon.
SUGGESTED READING
Beaty JH, Kasser JR. The elbow region: general concepts in the pediatric patient. In: Kasser JR, Beaty JH, eds. Rockwood and Wilkins’ fractures in children, 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2001.
Mason MB. Some observations on the fractures of the head of the radius with a review of 100 cases. Br J Surg. 1954; 42:123–132.
Fractures of the Proximal Ulna
The proximal ulna is particularly susceptible to fracture due to its subcutaneous position. Most fractures are intra-articular which can alter joint function and stability (see Fig. 11-12). Fractures with disruption of the triceps fascial expansions tend to displace significantly (see Fig. 11-13). Most olecranon fractures occur from direct blows to the flexed elbow.
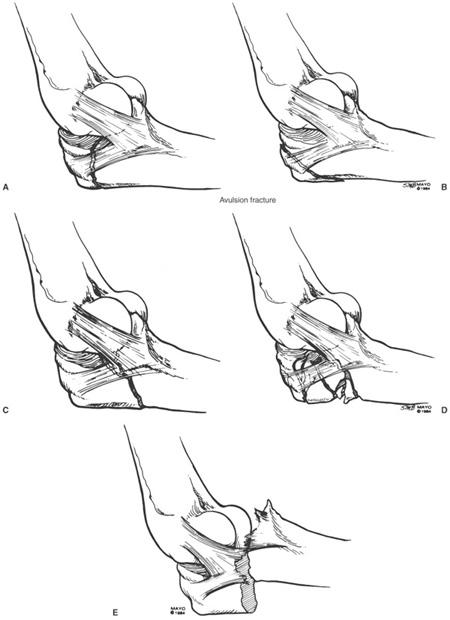
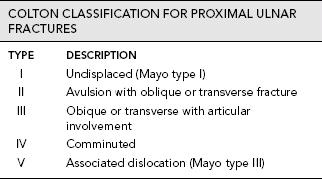
Several classification systems have been used. The Colton classification is commonly used and it is less complex than the Orthopaedic Trauma Association classification (see Fig. 11-14). The Mayo classification is similar, but based on the degree of comminution, displacement, and instability. Type I fractures are minimally undisplaced (separation ≤2 mm) with minimal comminution. These injuries account for 5% of olecranon fractures. Type II fractures are displaced, but stable and account for 85% of olecranon fractures. Type III fractures are displaced and unstable and may be comminuted. The type III fracture is associated with disruption of the medial collateral ligament, of the ulnar part of the lateral collateral ligament, or both. There is associated instability of the distal ulnar fragment.
SUGGESTED READING
Colton CL. Fractures of the olecranon in adults. Classification and management. Injury. 1973;5:121–127.
Morrey BF. Instructional course lectures. Complex instability of the elbow. J Bone Joint Surg. 1997;79A:460–469.
Coronoid Fractures
Isolated coronoid fractures are uncommon. Most are associated with other fractures or dislocations of the elbow. The incidence is 2% to 10% in association with posterior dislocations. Instability is common following coronoid fractures.
Regan and Morrey classified coronoid fractures into three types (see Fig. 11-15). Type I fractures are avulsions of the coronoid tip. Type II fractures involve ≤50% of the coronoid and type III fractures >50% of the coronoid. Subcategories are added to each type depending upon the lack of associated dislocation (type A) or the presence of an associated dislocation (type B).
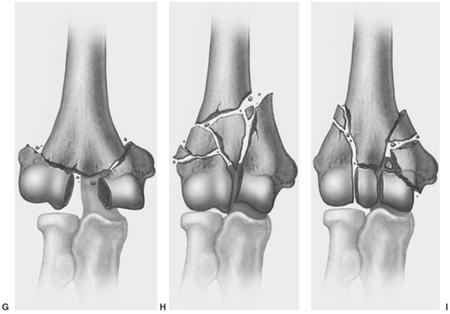
 Fig. 11-6 Orthopaedic Trauma Association classification for distal humeral fractures. A: Type A1—medial epicondyle avulsion, B: Type A2—simple extra-articular, C: Type A3—comminuted extra-articular, D: Type B1—partial articular lateral, E: Type B2—partial articular medial, F: Type B3—partial articular frontal, G: C1—Y or T intracondylar, H: Type C2—Y or T with metaphyseal comminution, I: Type C3—Y or T with comminuted articular surface.
Fig. 11-6 Orthopaedic Trauma Association classification for distal humeral fractures. A: Type A1—medial epicondyle avulsion, B: Type A2—simple extra-articular, C: Type A3—comminuted extra-articular, D: Type B1—partial articular lateral, E: Type B2—partial articular medial, F: Type B3—partial articular frontal, G: C1—Y or T intracondylar, H: Type C2—Y or T with metaphyseal comminution, I: Type C3—Y or T with comminuted articular surface.
SUGGESTED READING
Morrey BF. Current concepts in the treatment of fractures of the radial head, the olecranon and the coronoid. J Bone Joint Surg. 1995;77A:316–327.
Monteggia Fractures
The Monteggia fracture accounts for 7% of proximal ulnar fractures and is associated with dislocation of the radial head. The injury is uncommon, accounting for only 0.7% of elbow injuries. Multiple mechanisms of injury have been described including a direct blow to the ulna, falls on the outstretched hand with the elbow flexed at impact, and hyperextension injuries of the elbow.
The Bado classification is commonly used for adult Monteggia fractures (see Fig. 11-16). Type I fractures demonstrate anterior angulation of the ulnar fracture and anterior dislocation of the radial head (see Fig. 11-17). These injuries account for 50% to 75% of Monteggia fractures. Type I injuries are also common in children. However, fractures are often incomplete. A greenstick fracture or bowing of the ulna may be the only ulnar features.
Bado type II fractures have posterior angulation of the ulnar fracture and posterior or posterolateral dislocation of the radial head (see Fig. 11-18). This injury is more common in adults and accounts for 10% to 15% of Monteggia fractures.
Bado type III injuries have metaphyseal ulnar fractures with lateral or antolateral dislocation of the radial head (Fig. 11-16C). This injury is also common in children and accounts for 6% to 20% of Monteggia fractures.
Bado type IV fractures have proximal fractures of the radius and ulna with anterior dislocation of the radial head (Fig. 11-16D). This is the most uncommon fracture, accounting for approximately 5% of Monteggia injuries.
Jupiter divided Bado type II fractures into four categories. Type IIA where the ulnar fracture involves the distal olecranon and coronoid, type IIB where the ulnar fracture is at the metaphyseal–diaphyseal junction distal to the coronoid, type IIC where the ulnar fracture is diaphyseal and type IID where the fracture extends into the proximal ulna.
SUGGESTED READING
Bado JL. The Monteggia lesion. Clin Orthop. 1967;50:71–86.
Jupiter JB, Leibovic SJ, Bibbans W, et al. The posterior Monteggia lesion. J Orthop Trauma. 1991;5:395–402.
Letts M, Locht R, Weins J. Monteggia fracture-dislocations in children. J Bone Joint Surg. 1985;67B:724–727.
 Fig. 11-7 Anteroposterior (AP) radiograph in an elderly adult with an avulsion of the medial epicondyle (OTA A1).
Fig. 11-7 Anteroposterior (AP) radiograph in an elderly adult with an avulsion of the medial epicondyle (OTA A1).
Dislocations
Dislocations of the elbow are the most common dislocation in children and the second most common dislocation in adults. Most dislocations are posterior (see Fig. 11-19). Anterior dislocations are rare and usually occur in children. The mechanism of injury is a fall on the outstretched hand. The radius and ulna may also separate (divergent dislocation) with disruption of the interosseous membrane. This injury is the result of high-velocity trauma and is quite rare. Fractures are commonly associated dislocations. Fractures of the radial head and neck occur in 5% to 10%, epicondylar avulsions in 12%, and coronoid fractures in 10% of elbow dislocations.
SUGGESTED READING
Cohen MS, Hastings H. Acute elbow dislocation: Evaluation and management. J Am Acad Orthop Surg. 1998;6:15–23.
O’Driscoll SW, Morrey BF, Korineck S, et al. Elbow subluxation and dislocation. A spectrum of instability. Clin Orthop. 1992;280:186–197.
 Imaging of Elbow Injuries
Imaging of Elbow Injuries
Radiographs or computed radiographic (CR) images remain the primary screening technique for elbow fracture/dislocations. Anteroposterior (AP), lateral, and both oblique views account for routine trauma series. These views demonstrate alignment of the radial head with the capitellum regardless of the projection (see Fig. 11-20). The lateral view is useful for evaluating secondary signs of fracture such as displacement of the anterior and posterior fat pads. These structures are intracapsular, but extrasynovial (see Fig. 11-21). The anterior fat pad is normally visualized on the lateral view. The posterior fat pad is normally obscured within the olecranon fossa. When the anterior fat pad becomes elevated and the posterior fat pad (not normally visualized) is identified, a joint effusion is present and subtle fractures should be questioned (see Fig. 11-22). In children with posterior fat pads visualized on the lateral view, the incidence of fracture is approximately 90%. Cross-table lateral views may demonstrate a lipohemarthrosis, which also indicates an intraarticular fracture. The supinator fat stripe is also important to evaluate on the lateral view. Displacement or obliteration of this structure is common with fractures of the radial head and neck (Fig. 11-22). An abnormal fat stripe is also evident in 82% of other elbow injuries.

 Fig. 11-8 Anteroposterior (AP) radiograph demonstrating a partial articular lateral condyle fracture (arrows)(OTA B1).
Fig. 11-8 Anteroposterior (AP) radiograph demonstrating a partial articular lateral condyle fracture (arrows)(OTA B1).
 Fig. 11-9 Lateral radiograph demonstrating a partial articular frontal fracture (white arrows) (OTA B3).
Fig. 11-9 Lateral radiograph demonstrating a partial articular frontal fracture (white arrows) (OTA B3).
Additional views or fluoroscopically positioned spot images or stress views may also be obtained. However, currently, computed tomography (CT) is more commonly performed instead of additional radiographic views to clearly define the extent of the injury and evaluate subtle fractures following reduction of dislocations (see Figs. 11-23 and 11-24). In certain cases, magnetic resonance imaging (MRI) may be indicated to evaluate subtle fractures (see Fig. 11-25), neurovascular structures, the interosseous membrane, and for evaluating soft tissue compartments in patients with suspected compartment syndrome.
SUGGESTED READING
Berquist TH, Trigg SD. The elbow. In: Berquist TH, ed. Imaging atlas of orthopaedic appliances and prostheses. NewYork: Raven Press; 1995:751–816.
Rogers SL, MacEwan DW. Changes due to trauma in the fat plane overlying the supinator muscle: A radiographic sign. Radiology. 1969;92:954.
Yousefzadeh DK, Jackson JH. Lipohemarthrosis of the elbow joint. Radiology. 1978;128:643–645.

 Fig. 11-10 Anteroposterior (AP) radiograph demonstrating a Y intracondylar fracture with subtle comminution of the metaphysic (arrow) (OTA C2).
Fig. 11-10 Anteroposterior (AP) radiograph demonstrating a Y intracondylar fracture with subtle comminution of the metaphysic (arrow) (OTA C2).
 Treatment Options
Treatment Options
Treatment options vary with the type and extent of injury and patient factors. Open reduction and internal fixation is contraindicated in patients with advanced osteoporosis or significant bone loss, patients with neurologic deficit in the involved extremity, and in patients with significant health issues who cannot tolerate surgery. For purposes of discussion treatment of injury categories will be discussed separately.
 Fig. 11-11 Mason classification of radial head fractures. A: Type I—undisplaced radial head or neck fracture. B: Type II—radial head or neck fracture with >2 mm of displacement. C: Type III—comminuted radial head or neck fractures. D: Type IV—radial head fracture with associated dislocation.
Fig. 11-11 Mason classification of radial head fractures. A: Type I—undisplaced radial head or neck fracture. B: Type II—radial head or neck fracture with >2 mm of displacement. C: Type III—comminuted radial head or neck fractures. D: Type IV—radial head fracture with associated dislocation.
Distal Humeral Fractures
As noted in the preceding text, distal humeral fractures may be extra-articular (OTA type A), uniarticular (OTA type B), or complete articular (OTA type C). Unicondylar fractures may involve the medial or lateral column. These fractures are rare in adults and common in children. The lateral column is more frequently involved.
Stable undisplaced fractures may be treated with closed reduction and immobilization. External fixation with hinged or static techniques can be used for open wounds or in patients in whom stable reduction cannot be achieved.
Most displaced fractures require open reduction and internal fixation. Extra-articular fractures and stable unicondylar fractures may be treated with K-wire fixation or lag screws (see Figs. 11-26 and 11-27). Fractures involving the shaft may require plate and screw fixation.
Treatment of complete articular fractures (OTA type C) is more complex. Muscle forces act to displace and rotate the medial and lateral columns (see Fig. 11-28). Therefore, the columns and the distal articular surfaces must be stabilized. This can be accomplished with condylar and transverse K-wires or screws, medial and lateral plate, and screws using reconstruction plates (see Fig. 11-29) or locking plates (Fig. 11-27B), or Y plates (see Fig. 11-30). In certain cases, complex fractures of the distal humerus in older patients may be treated with elbow arthroplasty.
SUGGESTED READING
Anglen J. Distal humeral fractures. J Am Acad Orthop Surg. 2005;13:291–297.
Cobb TK, Morrey BF. Total elbow arthroplasty as a primary treatment for distal humeral fractures in elderly patients. J Bone Joint Surg. 1997;79A:826–832.
Sanchez-Sotelo J, Torchia ME, O’Driscoll SW. Complex distal humeral fractures: Internal fixation with a principle-based parallel-plate technique. J Bone Joint Surg. 2007;89A: 961–969.
Radial Head Fractures
The Mason classification for radial head fractures was reviewed in the previous section. Simple fractures (type I) are undisplaced and have no associated injuries. Type II injuries involve >30% of the articular surface and type III injuries are comminuted. Simple type I fractures, without associated osseous or soft tissue injuries, are managed conservatively. The joint can be aspirated to decompress the hemarthoris.
 Fig. 11-12 Intra-articular fracture of the proximal ulna. A: Lateral radiograph demonstrating an undisplaced fracture of the ulna entering the joint space. Anteroposterior (AP) (B) and lateral (C) radiographs of the wrist demonstrate an associated impacted fracture of the distal radius.
Fig. 11-12 Intra-articular fracture of the proximal ulna. A: Lateral radiograph demonstrating an undisplaced fracture of the ulna entering the joint space. Anteroposterior (AP) (B) and lateral (C) radiographs of the wrist demonstrate an associated impacted fracture of the distal radius.
 Fig. 11-13 Displaced olecranon fracture with disruption of the triceps fascia. A: Lateral radiograph demonstrating a significantly displaced olecranon fracture. Anteroposterior (AP) (B) and lateral (C) radiographs following reduction with K-wires and tension bands.
Fig. 11-13 Displaced olecranon fracture with disruption of the triceps fascia. A: Lateral radiograph demonstrating a significantly displaced olecranon fracture. Anteroposterior (AP) (B) and lateral (C) radiographs following reduction with K-wires and tension bands.
 Fig. 11-14 A and B: Avulsion fractures which may (A) or may not (B) involve the joint space. B is a Colton type II injury. C: Transverse or oblique fractures involving the joint space (Colton type III). D: Comminuted fracture involving most of the olecranon process (Colton type IV). E: Ulnar fracture with displaced distal fragment (Colton type V, Mayo type III). (From Morrey BF. The elbow and its disorders. Philadelphia: WB Saunders; 1985.)
Fig. 11-14 A and B: Avulsion fractures which may (A) or may not (B) involve the joint space. B is a Colton type II injury. C: Transverse or oblique fractures involving the joint space (Colton type III). D: Comminuted fracture involving most of the olecranon process (Colton type IV). E: Ulnar fracture with displaced distal fragment (Colton type V, Mayo type III). (From Morrey BF. The elbow and its disorders. Philadelphia: WB Saunders; 1985.)
 Fig. 11-15 Coronoid fracture classification of Regan and Morrey. Lateral radiograph demonstrating a type I avulsion of the coronoid tip (arrow). Type II fractures involve <50% of the coronoid (white line) and type III fractures involve >50% of the coronoid.
Fig. 11-15 Coronoid fracture classification of Regan and Morrey. Lateral radiograph demonstrating a type I avulsion of the coronoid tip (arrow). Type II fractures involve <50% of the coronoid (white line) and type III fractures involve >50% of the coronoid.
Treatment of displaced fractures (type II) is more controversial. If there is good range of motion, the fracture can be treated with immobilization of the elbow and wrist for 2 to 3 weeks before beginning active range of motion. In younger patients, operative intervention should be considered if range of motion is not satisfactory following conservative management. Small lag screws can be placed to stabilize the radial head fragment and articular surface (see Fig. 11-31). If the radial neck is involved, a miniplate and screws can be used for fixation.
Type III comminuted fractures have been most often treated with resection of the radial head. However, in recent years good results have been obtained with open reduction and internal fixation (see Fig. 11-32).
Radial head fractures are associated with elbow dislocations (type IV) in 10% of patients. The elbow should be reduced and radial articular surface fully evaluated on radiographs or CT. Treatment is similar to isolated fractures, except type III fractures are more commonly treated with resection of the radial head. In patients with instability, radial head prostheses should be considered. Currently, titanium implants are more often used due to problems with earlier silicone implants (see Fig. 11-33).
SUGGESTED READING
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree