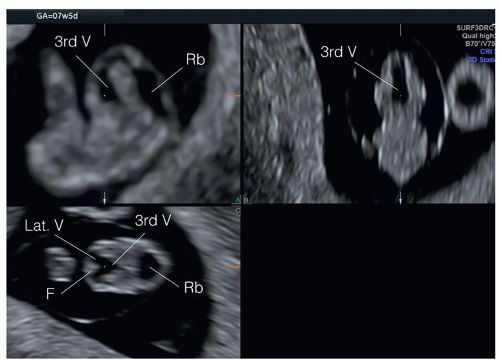
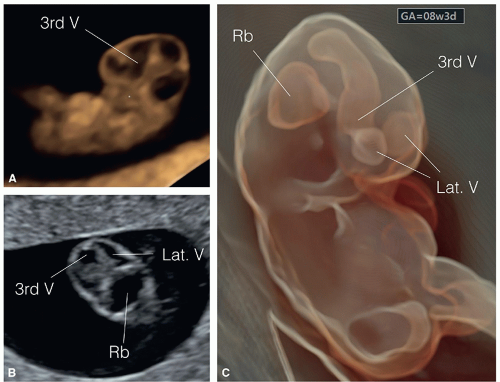
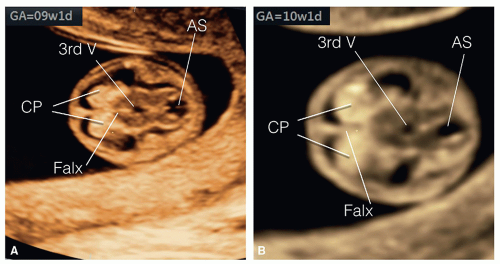
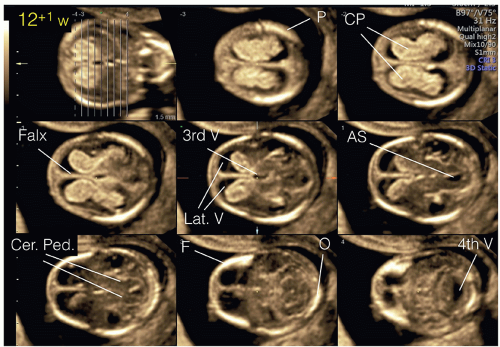
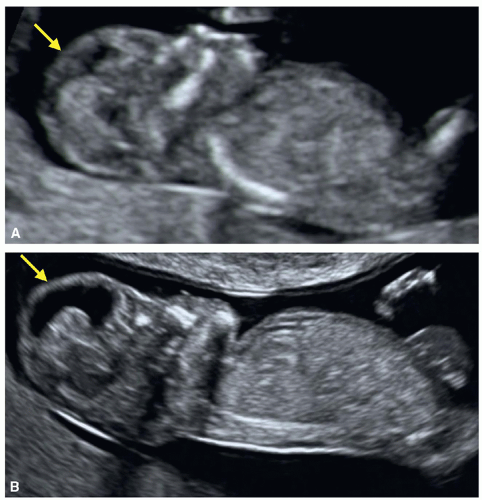
into two equal halves, and the choroid plexuses, which fill the lateral ventricles, are seen on ultrasound by the end of the eighth week and beginning of the ninth week of gestation (Fig. 8.3). The cerebellar hemispheres develop in the rhombencephalon and are completely formed by the 10th week of gestation, thus allowing for evaluation of the posterior fossa with optimal ultrasound imaging (Fig. 8.4). Prior to the 9th week of gestation, the cranium is not typically ossified (Fig. 8.5). Cranial ossification begins around the late 9th, early 10th week and is completed by the 12th week of gestation. Figure 8.5 shows progression in fetal cranial ossification from 9 to 13 weeks of gestation.
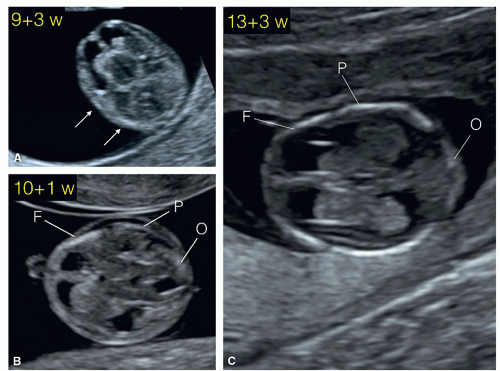 Figure 8.5: Axial planes of the fetal head at 9 (A), 10 (B), and 13 (C) weeks of gestation demonstrating the progression of skull ossification. Note at 9 weeks of gestation (A), the presence of small islands of ossification (arrows). At 10 weeks of gestation (B), partial ossification of the frontal (F), parietal (P) and occipital (O) bones is seen. At 13 weeks of gestation (C), the frontal (F), parietal (P) and occipital (O) bones are clearly seen. The occipital bone (O) is better imaged in a more posterior plane at the level of basal ganglia (see Figs. 8.6 and 8.10). |
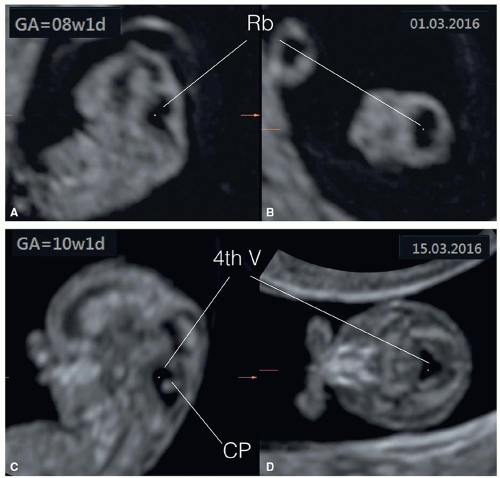
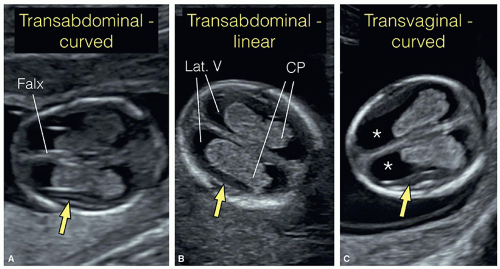
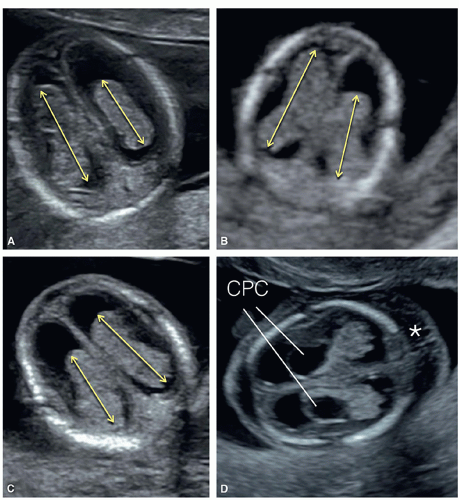
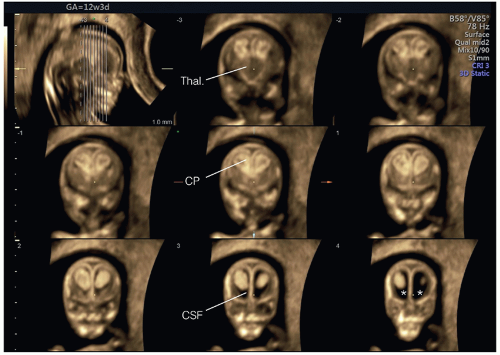
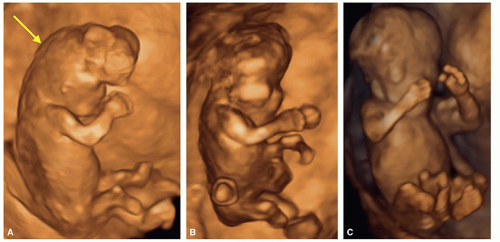
the choroid plexus is described to be similar to a butterfly (Fig. 8.8).2 The left and right choroid plexuses are rarely of similar size and shape, and this difference is considered part of the normal variation (Fig. 8.9).3 A small rim of the developing cortex can be seen laterally surrounding the choroid plexuses (Fig. 8.7). In an axial superior plane of the fetal head, a fluid rim can be seen surrounding the choroid plexus on each side, corresponding to the lateral ventricle (Fig. 8.10A). A more inferior axial plane toward the base of the skull shows the two thalami and the third ventricle, forming the diencephalon
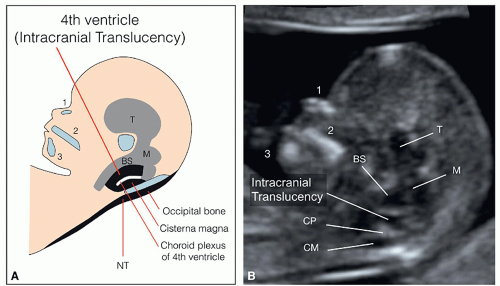
(Fig. 8.10B). Posterior to the thalami, the two small cerebral peduncles are identified surrounding the aqueduct of Sylvius and forming the mesencephalon (midbrain) (Fig. 8.10B). The developing cerebellum is identified in the posterior fossa primarily by transvaginal ultrasound and in an axial plane that is tilted toward the upper spine (Fig. 8.11A). A slightly more inferior plane will show the fourth ventricle, the future cisterna magna, and the hyperechogenic choroid plexus of the fourth ventricle (Fig. 8.11B). Table 8.1 gives an overview of the anatomic landmarks and corresponding malformations that can be visualized in the axial planes of the fetal head in the first trimester.
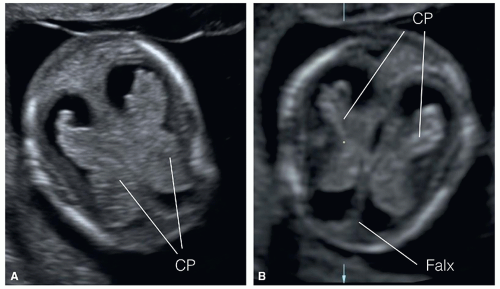 Figure 8.8: Axial view of the fetal head at the level of the choroid plexuses (CP) in a fetus at 11 weeks (A) and at 13 weeks (B) of gestation. Note that the right and left CP resemble the shape of a butterfly and are referred to as the “butterfly sign.” The falx cerebri (Falx) is seen in the midline. Compare with Figures 8.24 and 8.25 obtained from fetuses with alobar holoprosencephaly. |
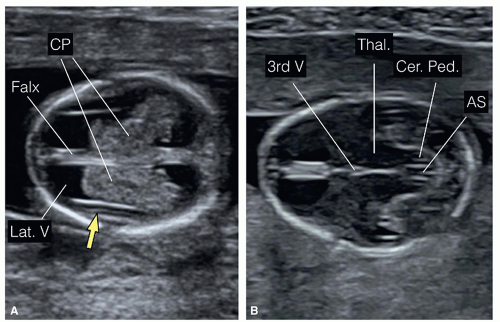 Figure 8.10: Axial views of the fetal head at 13 weeks of gestation obtained superiorly at the level of the lateral ventricles (A) and inferiorly at the level of the thalami (B). In A, the two lateral ventricles (Lat. V), the choroid plexuses (CP), and the falx cerebri (Falx) are seen. In B, the thalami (Thal.) with the third ventricle (3rd V) are recognized and constitute the diencephalon. Posterior to the thalami, the cerebral peduncles (Cer. Ped.) with the aqueduct of Sylvius (AS) can be visualized and form the mesencephalon (see Fig. 8.11). |
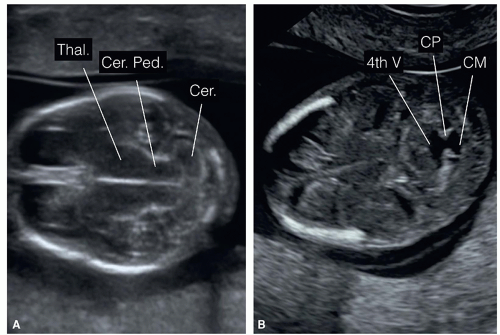 Figure 8.11: Axial view of the fetal head at 13 weeks of gestation obtained at the level of the posterior fossa (inferior to planes A and B in Fig. 8.10). A: At the level of the developing cerebellum (Cer.) and cerebral peduncles (Cer. Ped.). Note the thalami (Thal.) in a more anterior location. B: An oblique, slightly more inferior plane demonstrating the open fourth ventricle (4th V) connecting to the future cisterna magna (CM). The echogenic choroid plexus (CP) of the fourth ventricle can also be seen. |
Table 8.1 • Axial Planes of the Fetal Head and Associated Abnormalities in the First Trimester | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 8.2 • Midsagittal Plane of the Fetal Head and Associated Abnormalities in the First Trimester | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
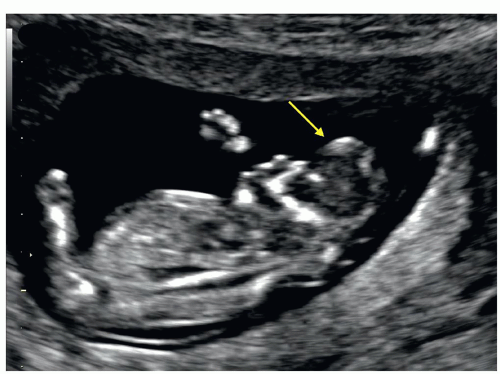
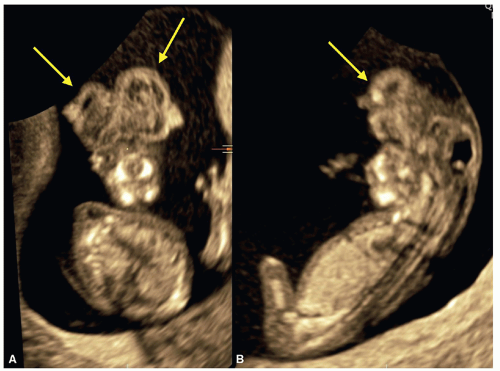
the orbits (Fig. 8.16) and on coronal view of the fetal face, the characteristic “frog eyes” appearance is noted (Fig. 8.16B). By the 12th week of gestation, following complete ossification of the fetal skull, ultrasound diagnosis of exencephaly/anencephaly can be performed by the axial, sagittal, or coronal views of the fetal head.6 In these views, the absent calvarium, the abnormal fetal profile, and the disorganized brain tissue protruding from the fetal head can be demonstrated (Figs. 8.14, 8.15, 8.16, 8.17 and 8.18). On transvaginal ultrasound, the amniotic fluid appears echogenic (Fig. 8.16A). The crown-rump length measurements are often
smaller than expected due to loss of brain tissue. The diagnosis of exencephaly/anencephaly can be occasionally suspected at 9 weeks of gestation.6 A follow-up ultrasound after 10 weeks is recommended in order to confirm the diagnosis, especially if pregnancy termination is being contemplated. On occasions, acrania can be diagnosed in the first trimester by the demonstration of absence of cranium and in the presence of membrane (pia mater) covering the brain tissue (Fig. 8.17). In most cases of acrania, follow-up ultrasound examination into the second trimester demonstrates amorphous brain tissue as shown in anencephaly-exencephaly cases. 3D ultrasound can help in providing a complete picture of face and head in anencephalic fetuses (Fig. 8.18).
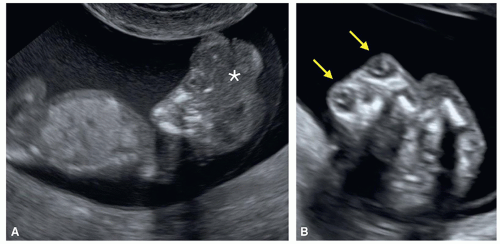
are often associated with abnormal brain anatomy that can be detected in the axial or sagittal views of the fetal head (Figs. 8.19, 8.20, 8.21 and 8.22). The larger the encephalocele, the more brain abnormality is seen on ultrasound. As encephaloceles are often part of genetic abnormalities and syndromes, detailed review of fetal anatomy is recommended.7 Special attention should be given to the presence of polydactyly and polycystic kidneys given the association with Meckel-Gruber syndrome (Figs. 8.21 and 13.31).7 Other autosomal recessive ciliopathies can present with posterior cephalocele, such as Walker-Warburg syndrome or the large group of Joubert syndrome-related disorders (Fig. 8.22). Three-dimensional (3D) ultrasound in surface mode can be of help in showing the extent of the encephalocele. Not all cases of cephaloceles are detectable in the first trimester. Smaller defects and internal lesions are difficult to diagnose. The diagnosis of an encephalocele in the first trimester is commonly performed around 13 to 14 weeks unless a meningocele with a dilated posterior fossa is present, mimicking a Dandy-Walker malformation (DWM) enabling an earlier detection (Figs. 8.22 and 13.31). In isolated cases, an attempt should be made to differentiate between an encephalocele and a meningocele given a much improved prognosis of the latter. The absence of brain tissue in the herniated sac on transvaginal ultrasound along
with normal intracranial anatomy make the diagnosis of a meningocele more likely.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree