The Fetal Chest
INTRODUCTION
The examination of the fetal chest in the first trimester includes the assessment of the right and left lung, the bony and cartilaginous thoracic cage, the diaphragm, and the heart with surrounding vasculature. Because of the importance and prevalence of cardiac anomalies, normal and abnormal anatomy of the heart and surrounding vasculature are presented in Chapter 11. Normal and abnormal appearance of lungs, diaphragm, and rib cage in the first trimester are discussed in this chapter. Pentalogy of Cantrell, involving a sternal defect, and ectopia cordis are discussed in Chapter 12.
EMBRYOLOGY
The respiratory diverticulum or lung bud is first seen around day 22 from fertilization as a ventral outgrowth of the primitive foregut. As the lung bud grows, it is surrounded by mesoderm, which gives rise to the lung vasculature, connective tissue, and muscle within the bronchial tree. The lengthening lung bud bifurcates on day 28 into the right and left lung buds, which gives rise to the right and left lung, respectively. Growth and bifurcation of the lung buds along with the surrounding mesenchyme continues throughout pregnancy. The terminal bronchioles are seen by the 28th week of gestation (menstrual) and the terminal sacs are formed by the 36th week of gestation. Maturation of the alveoli occurs between the 36th week of gestation and term. Alveolar growth continues into early childhood.
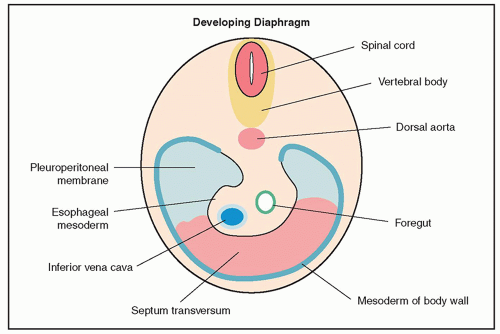
The four embryonic structures—septum transversum, pleuroperitoneal membranes, mesoderm of body wall, and the esophageal mesoderm—coalesce to form the diaphragm (Fig. 10.1). The central tendon of the diaphragm is primarily formed from the septum transversum. The diaphragm is completely formed by the end of the 10th to 11th week of gestation.
In the sixth week of embryogenesis, the sternum arises from the somatic mesoderm as paired longitudinal sternal bars. These bars fuse in the midline to form a cartilaginous sternum at around the 10th week. Sternal ossification starts at day 60 in a segmental arrangement. The xiphoid process does not ossify until after birth. The vertebral bodies and ribs are also derived from the paraxial mesoderm.
NORMAL SONOGRAPHIC ANATOMY
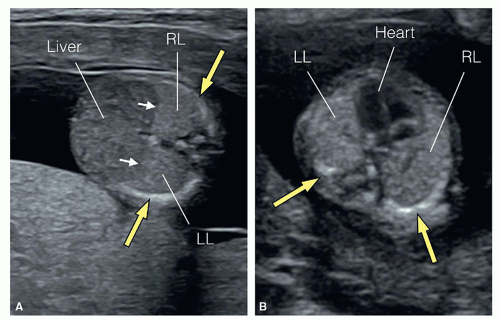
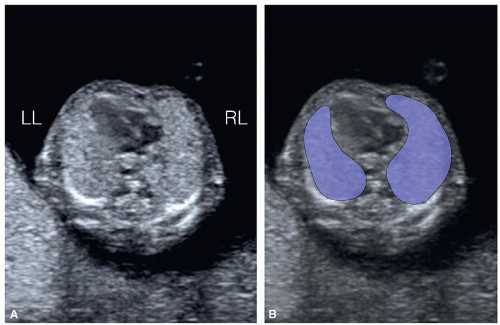
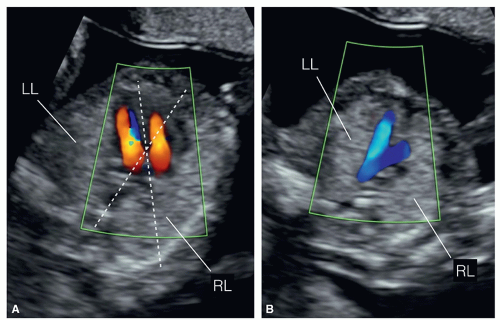
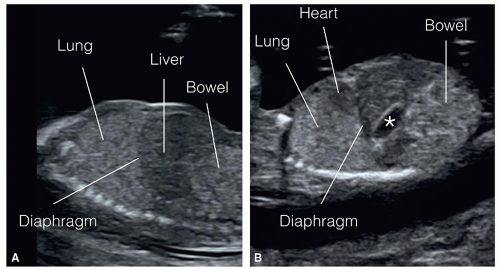
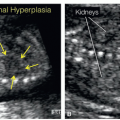
The systematic visualization of the fetal chest in the first trimester is generally achieved from multiple sonographic planes. Axial views, at the level of the upper abdomen (Fig. 10.2A), the chest (Figs. 10.2B, 10.3, and 10.4A), and mediastinum
(Fig. 10.4B), allow for the evaluation of the diaphragm, right and left lungs, midline structures such as the esophagus, trachea/bronchi, and the thymus gland. In the normal fetus, the lungs appear slightly more echogenic than the liver and cardiac muscle (Fig. 10.2). At the four-chamber view plane, the right and left lungs are seen and the rib cage assessed (Figs. 10.2B, 10.3 and 10.4A). Comprehensive evaluation of the lungs in axial views requires the assessment at the level of the four-chamber view (Figs. 10.2B, 10.3 and 10.4A) and superiorly into the upper mediastinum at the three-vessel-trachea view (Fig. 10.4B). Assessment of cardiac position and axis in the chest (Fig. 10.4A) is helpful in the identification of lung abnormalities.
(Fig. 10.4B), allow for the evaluation of the diaphragm, right and left lungs, midline structures such as the esophagus, trachea/bronchi, and the thymus gland. In the normal fetus, the lungs appear slightly more echogenic than the liver and cardiac muscle (Fig. 10.2). At the four-chamber view plane, the right and left lungs are seen and the rib cage assessed (Figs. 10.2B, 10.3 and 10.4A). Comprehensive evaluation of the lungs in axial views requires the assessment at the level of the four-chamber view (Figs. 10.2B, 10.3 and 10.4A) and superiorly into the upper mediastinum at the three-vessel-trachea view (Fig. 10.4B). Assessment of cardiac position and axis in the chest (Fig. 10.4A) is helpful in the identification of lung abnormalities.
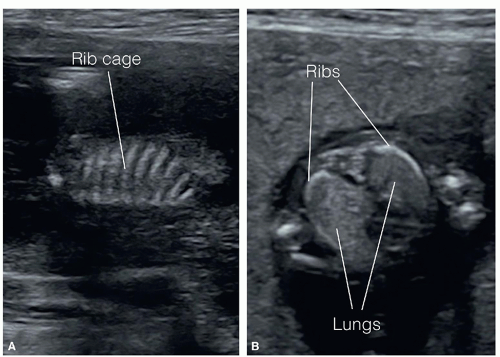
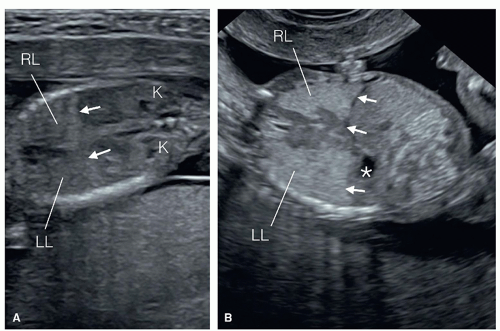
The right (Fig. 10.5A) and left (Fig. 10.5B) parasagittal views of the fetal chest are important for assessment of individual lung lobes, the diaphragm, and the rib cage (Fig. 10.6A). The
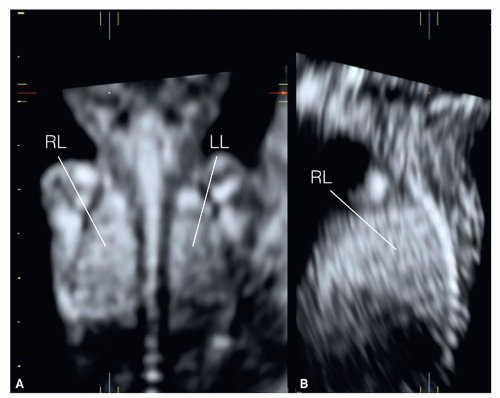
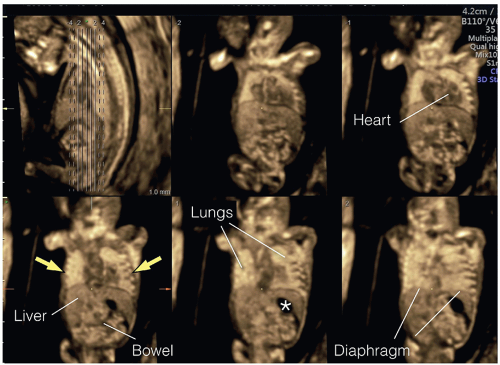
ribs can also be assessed from an axial plane of the chest at the level of the four-chamber view (Fig. 10.6B). In our opinion, the evaluation of the diaphragm is best achieved in coronal views (Fig. 10.7), starting from the posterior coronal view of the spine and moving more anteriorly toward the sternum. In these planes the diaphragm muscle and tendon on the right and left chest can be well visualized. The transvaginal approach improves visualization of all chest structures due to higher resolution (Fig. 10.7B). Three-dimensional ultrasound in a surface (Fig. 10.8) or tomographic display (Fig. 10.9)
can help in demonstrating various chest structures, especially in transvaginal scanning where transducer manipulation is limited. Clear visualization of the lungs can be achieved from about the 12th week of gestation onward.
ribs can also be assessed from an axial plane of the chest at the level of the four-chamber view (Fig. 10.6B). In our opinion, the evaluation of the diaphragm is best achieved in coronal views (Fig. 10.7), starting from the posterior coronal view of the spine and moving more anteriorly toward the sternum. In these planes the diaphragm muscle and tendon on the right and left chest can be well visualized. The transvaginal approach improves visualization of all chest structures due to higher resolution (Fig. 10.7B). Three-dimensional ultrasound in a surface (Fig. 10.8) or tomographic display (Fig. 10.9)
can help in demonstrating various chest structures, especially in transvaginal scanning where transducer manipulation is limited. Clear visualization of the lungs can be achieved from about the 12th week of gestation onward.
CHEST ABNORMALITIES
Hydrothorax/Pleural Effusion
Definition
Hydrothorax (pleural effusion) is the accumulation of fluid in the pleural space between the lungs and the thoracic cage. Hydrothorax may occur unilaterally or bilaterally and may be primary or secondary. Primary hydrothorax is a diagnosis made after excluding causes of hydrothorax, which are many, and involve fetal lung or cardiovascular malformations, fetal arrhythmias, infections, chromosomal aneuploidy, and others. In a prospective study between 7 and 10 weeks of gestation, hydrothorax was found in 1.2% of embryos.1 The presence of bilateral hydrothorax in the first trimester is associated with a poor prognosis. Follow-up of 14 fetuses with bilateral hydrothorax diagnosed in the first trimester showed only one survivor. A high incidence of chromosomal aneuploidy, including monosomy X, was also reported.1 Isolated unilateral hydrothorax with no other fetal abnormality may be a transient finding with disappearance of the effusion upon follow-up ultrasound in the second trimester.
Ultrasound Findings
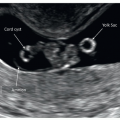
Accumulation of fluid around the lungs is relatively easy to detect on ultrasound on axial (Figs. 10.10, 10.11, and 10.12A), coronal, or sagittal views (Fig. 10.12B). A typical sign for hydrothorax involves the presence of fluid between the lateral borders of the lungs and the ribs (Figs. 10.10, 10.11 and 10.12). This sign allows for differentiating hydrothorax from pericardial effusion, which can be difficult in some cases. In pericardial effusion, the fluid surrounds the heart and is on the medial aspects of the lungs (Fig. 10.13). The presence of severe hydrothorax results in lung compression with the typical “butterfly” appearance of the lungs. The association of hydrothorax with fetal hydrops is easily seen and is commonly noted with increased nuchal translucency (NT) and genetic abnormalities (Figs. 10.10 and 10.11). Diagnostic or therapeutic thoracocentesis is typically reserved for the second or third trimester of pregnancy. Figure 10.12 shows a fetus with an isolated unilateral hydrothorax that resolved by the second trimester of pregnancy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree