The Fetal Face and Neck
INTRODUCTION
Visualization of the fetal face and neck in early gestation is an important aspect of the ultrasound examination as it has been incorporated in the first-trimester fetal risk assessment for aneuploidy (Chapters 1 and 5). A midsagittal plane of the fetus is part of nuchal translucency (NT) measurement and is also used to assess for the presence or absence of nasal bones. A more detailed assessment of the fetal face and neck in the first trimester allows for the diagnosis of a number of abnormalities with high associations, including aneuploidy and genetic syndromes. In this chapter, we present a systematic approach to the evaluation of the fetal face and neck and discuss in detail major facial and neck abnormalities that can be diagnosed in the first trimester. The posterior fossa in the brain, which is also visualized in the midsagittal plane of the fetus, is separately discussed in Chapter 8 on central nervous system (CNS) anomalies.
EMBRYOLOGY
Embryologic development of the fetal face and neck is a complex process, which involves coordination of multiple tissues including ectoderm, neural crest, mesoderm, and endoderm with involvement of six pairs of pharyngeal arches. The pharyngeal arches play a dominant role in building the face and neck, including its skeletal, muscular, vascular, and nerve structures.
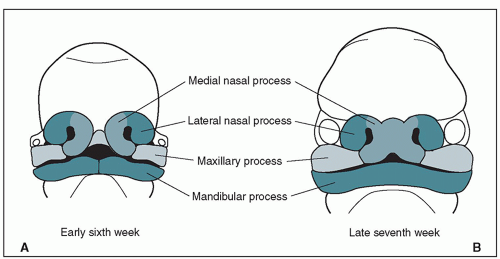
The first evidence of facial development is seen during the third week of embryogenesis with the formation of the oropharyngeal (oral) membrane, which lies at the opening of the foregut and represents the future oral cavity. During the fourth to seventh week of embryogenesis, five facial swellings or processes merge and fuse to form the facial structures. These facial processes include one frontonasal process, arising from crest cells, and two maxillary and mandibular processes, arising from the first pharyngeal arch (Fig. 9.1). The frontonasal process gives rise to two medial and two lateral nasal
processes. Table 9.1 and Figures 9.1 and 9.2 list the various contributions of facial processes to the development of facial structures. Fusion and merging of the medial nasal and maxillary processes form the primary palate, and the secondary palate is formed by fusion of the maxillary processes, which completes facial development by the 12th week of embryogenesis. Facial growth continues during the fetal period with changes in proportions and features of facial structures. Detailed embryologic development of the face and neck is beyond the scope of this book. Failure of development or fusion of facial processes contributes to the majority of facial abnormalities, including clefting, which is discussed later in this chapter.
processes. Table 9.1 and Figures 9.1 and 9.2 list the various contributions of facial processes to the development of facial structures. Fusion and merging of the medial nasal and maxillary processes form the primary palate, and the secondary palate is formed by fusion of the maxillary processes, which completes facial development by the 12th week of embryogenesis. Facial growth continues during the fetal period with changes in proportions and features of facial structures. Detailed embryologic development of the face and neck is beyond the scope of this book. Failure of development or fusion of facial processes contributes to the majority of facial abnormalities, including clefting, which is discussed later in this chapter.
Table 9.1 • Contributions of Embryologic Facial Prominences to Facial Structures | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
The pharyngeal arches contribute to the development of the neck. The third pharyngeal arch forms the skeletal structures of the hyoid bone. The parathyroid glands and the laryngeal cartilages are formed by fusion of the fourth and sixth pharyngeal arches. The thyroid gland originates around the 24th day of embryogenesis from the primitive pharynx and neural crest cells, forming the median and lateral thyroid, respectively. The median thyroid becomes the main thyroid gland. The thyroid descends in the neck until it reaches the front of the trachea in the seventh week of embryogenesis. The thyroid gland is the first endocrine organ to develop, and it starts producing thyroid hormones by the 12th week of menstrual age.
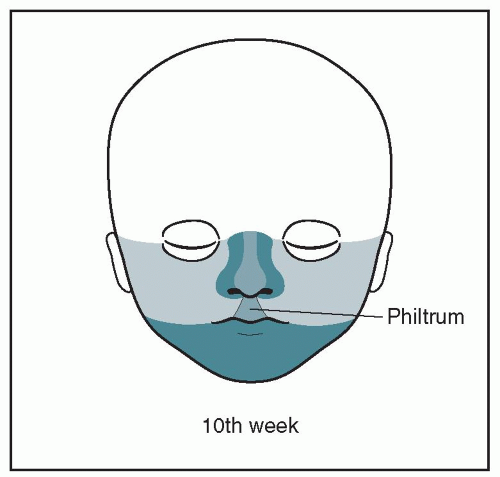 Figure 9.2: Formation of the lower face at 10 weeks of embryogenesis. Note that the face is completely formed, and note the contribution of various processes to the formation of the face. See Figure 9.1 for corresponding colors and text for details. |
NORMAL SONOGRAPHIC ANATOMY
The systematic visualization of the face and neck includes multiple approaches from the midsagittal, coronal, and axial planes. The midsagittal approach allows for the visualization of the facial profile and NT, and the coronal and axial planes allow for visualization of other facial and neck features. Several brain anatomic structures, such as the thalamus, brain stem, fourth ventricle, lateral ventricles, and choroid plexuses, can also be demonstrated in the midsagittal and parasagittal views of the head and face1 and are discussed in detail in Chapters 5 and 8. We will hereby describe normal sonographic features of the face and neck in each anatomic plane.
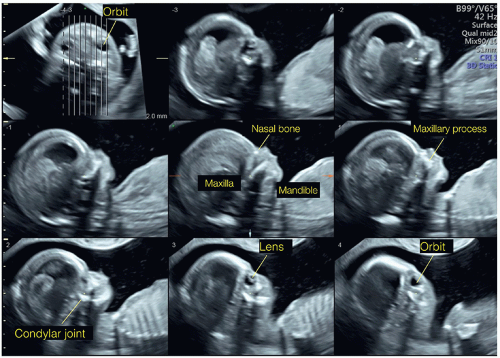
Sagittal Planes
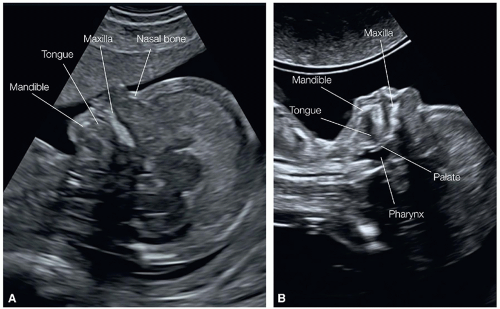
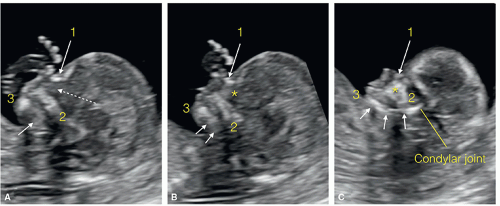
The midsagittal plane of the fetal head (Figs. 9.3 and 9.4), demonstrating the fetal profile in the first trimester, enables the assessment of the forehead, nose with nasal bone, mouth with maxilla, mandible anteriorly, and NT posteriorly. In the first trimester, the fetal head appears slightly larger in proportion to the body than later on in gestation, and in this midsagittal view the forehead shows some normal-appearing “frontal bossing” (Figs. 9.3 and 9.4). At this stage of early gestation, the metopic suture is still wide and the frontal bones are not seen in the midsagittal view. The perpendicular insonation to the nasal structures in the midsagittal plane of the face enables clear visualization of facial structures. The midsagittal plane landmarks are important in order to correctly identify the nasal bone on midsagittal scanning, with the demonstration of the “equal sign” formed by the nasal bone inferiorly and the nasal skin superiorly (Figs. 9.4, 9.5A, 9.6, and 1.1). The maxilla is recognized in the midsagittal plane as a continuous ossified region in the face (Figs. 9.4, 9.5 and 9.6). In the midsagittal plane, the anterior part of the mandible is seen as an echogenic dot under the anterior maxilla (Fig. 9.6A). In parasagittal views, a larger part of the mandible can be seen (Fig. 9.6C) as well as the maxillary process between the nasal bone and the maxilla (Fig. 9.6B). Several facial measurements in the midsagittal view have been proposed in the literature.2, 3, 4, 5, 6, 7, 8 The significance of abnormal facial measurements and anatomic markers is discussed later in this chapter.
In the posterior aspect of the midsagittal view, the neck with NT is also demonstrated. A detailed discussion of NT measurement (Figs. 9.3 and 9.4) and its significance is presented in Chapters 1 and 6. Conditions associated with a thickened NT and cystic hygroma are discussed at the end of this chapter.
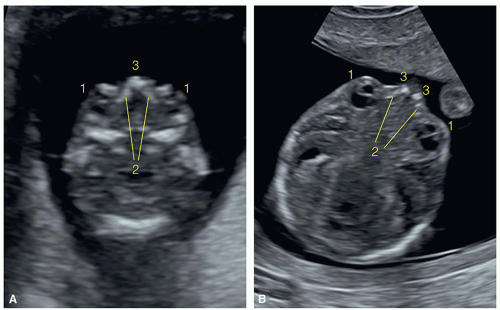
Coronal Planes
A frontal coronal view of the bony face in the first trimester reveals both orbits and eyes and their relationships to the nasal bridge and maxilla (Fig. 9.7) (see Chapter 5). The position, size, and shape of the eyes and orbits are generally assessed in a subjective manner. A coronal view of the face demonstrates
the anterior maxilla (alveolar ridge) (Fig. 9.7). The retronasal triangle is imaged in an oblique plane, between the coronal and axial planes of the face, in the region of the nose and maxilla (Fig. 9.7B)9 (see Chapter 5 and Fig. 5.9). An oblique plane between the maxilla and the mandible normally reveals a mandibular gap (Fig. 9.7B).10 Good visualization of facial structures is typically performed from a 3D surface rendering of the face, ideally obtained transvaginally.
the anterior maxilla (alveolar ridge) (Fig. 9.7). The retronasal triangle is imaged in an oblique plane, between the coronal and axial planes of the face, in the region of the nose and maxilla (Fig. 9.7B)9 (see Chapter 5 and Fig. 5.9). An oblique plane between the maxilla and the mandible normally reveals a mandibular gap (Fig. 9.7B).10 Good visualization of facial structures is typically performed from a 3D surface rendering of the face, ideally obtained transvaginally.
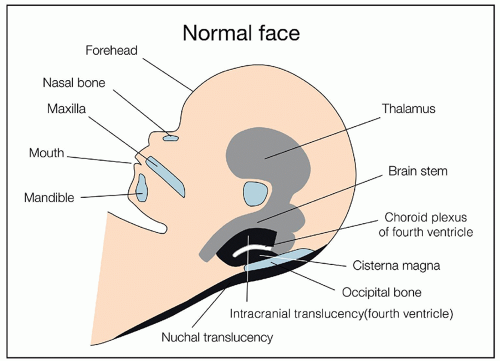 Figure 9.3: Schematic drawing of the midsagittal plane of the fetal head showing the fetal facial profile and displaying important anatomic structures evaluated by the first-trimester ultrasound, including forehead, nasal bone, maxilla, mouth, mandible, midline central nervous system structures, and nuchal translucency. See corresponding ultrasound in Figure 9.4 and text for details. |
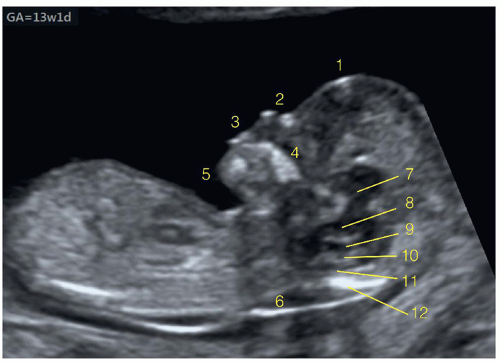 Figure 9.4: Midsagittal ultrasound plane of the fetal head at 13 weeks of gestation showing the profile with the forehead (1), nose with nasal bone (2), mouth (3), maxilla (4), and chin with mandible (5). The posterior aspect of the profile plane displays the nuchal translucency (6) and different anatomic structures of the midline brain to include the thalamus (7), brain stem (8), fourth ventricle as intracranial translucency (9), choroid plexus of the fourth ventricle (10), the developing cisterna magna (11), and the occipital bone (12). See Figure 9.3 for the corresponding schematic drawing. |
Axial Planes
In the experience of the authors, the systematic visualization of the axial planes of the face is of secondary importance to the midsagittal and coronal planes (Chapter 5). As performed in the second trimester, multiple axial planes obtained in the first trimester from cranial to caudal enable the demonstration of orbits, nasal bridge with nasal bones, the maxilla, and the mandible (Fig. 9.8) (Chapter 5). The fetal lips cannot be well identified on transabdominal scanning in the first trimester, and, when needed, imaging of these structures can be obtained transvaginally with high-resolution transducers.
Three-Dimensional Ultrasound of the Fetal Face
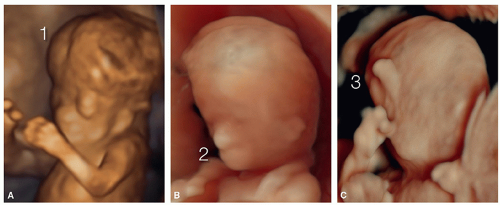
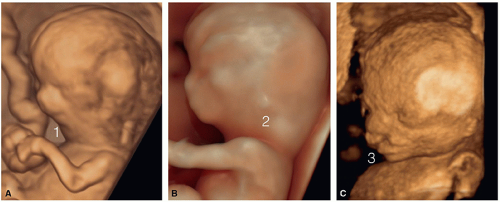
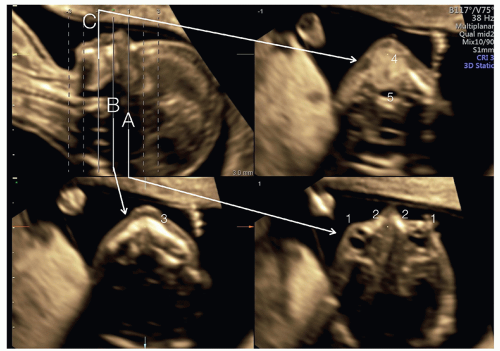
Similar to the use of three-dimensional (3D) ultrasound in surface mode of the fetal face in the second and third trimesters of pregnancy, 3D ultrasound in the first trimester (Fig. 9.9) provides additional information to the 2D midsagittal (profile), frontal, and axial facial views.11 When fetal abnormalities are suspected in the first trimester, 3D ultrasound of the fetal face in surface mode enables a detailed view of facial features, including the forehead, eyes, nose, mouth, chin, and ears (Figs. 9.9, 9.10 and 9.11). Three-dimensional ultrasound of the
fetal face can often be obtained by transabdominal acquisition, but when an abnormality is suspected the transvaginal approach provides for more details and higher resolution. Figures 9.9, 9.10 and 9.11 show examples of normal and abnormal fetal faces on 3D ultrasound in the first trimester of pregnancy. Three-dimensional ultrasound can also be used in multiplanar display with reconstruction of planes for the specific evaluation of target anatomic regions (Figs. 9.12, 9.13 and 9.14) such as the
bony face or the palate in the evaluation of facial anomalies (see later). For more details on the use of 3D ultrasound in the first trimester, refer to Chapter 3 in this book and a recent book on the clinical use of 3D in prenatal medicine.11
fetal face can often be obtained by transabdominal acquisition, but when an abnormality is suspected the transvaginal approach provides for more details and higher resolution. Figures 9.9, 9.10 and 9.11 show examples of normal and abnormal fetal faces on 3D ultrasound in the first trimester of pregnancy. Three-dimensional ultrasound can also be used in multiplanar display with reconstruction of planes for the specific evaluation of target anatomic regions (Figs. 9.12, 9.13 and 9.14) such as the
bony face or the palate in the evaluation of facial anomalies (see later). For more details on the use of 3D ultrasound in the first trimester, refer to Chapter 3 in this book and a recent book on the clinical use of 3D in prenatal medicine.11
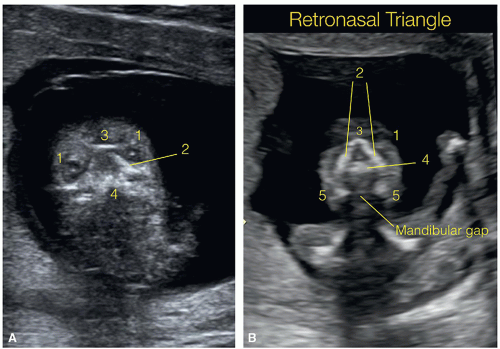 Figure 9.7: Coronal planes in two fetuses (A and B) at 12 weeks of gestation, obtained at the frontal aspects of the bony face. In fetus A, the coronal plane is at the level of the orbits and shows the two eyes (1) with orbits and lenses, between the maxillary processes (2), the nasal bones (3), and the anterior aspect of the maxilla (4) with the alveolar ridge. In fetus B, the plane is oblique and demonstrates the retronasal triangle (see text for details), which is formed by the nasal bones superiorly (3), the frontal processes of the maxilla laterally (2), and the alveolar ridge (primary palate) inferiorly (4). This coronal section (B) is posterior to the tip of the mandible, and therefore the two lateral bodies of the mandible are seen (5) with a normal gap between, called the mandibular gap. The presence of micrognathia results in disappearance of the mandibular gap in the retronasal triangle plane. See Figure 9.14 to help understand the anatomic facial location of the retronasal triangle plane. |
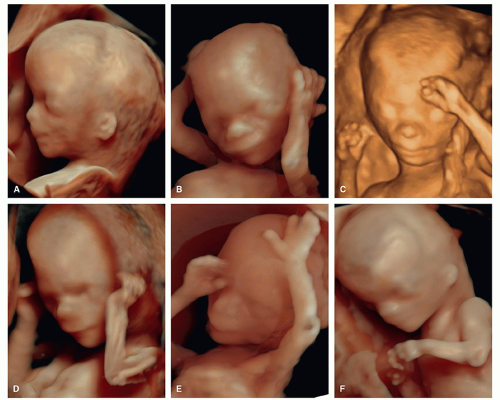 Figure 9.9: Three-dimensional ultrasound images in surface mode of the normal fetal face obtained in six fetuses (A-F) by the transvaginal approach. Note the physiologic frontal bossing and the clear anatomic regions of forehead, eyes, nose, mouth, chin, and ears. Compare with Figures 9.10 and 9.11 obtained in abnormal fetuses. |
BIOMETRIC MEASUREMENTS OF THE FACE
Several biometric measurements are currently published for the assessment of facial features in the second and third trimesters, and some of these are proposed for use in the first-trimester ultrasound screening. These measurements include diameters, ratios, and angles, primarily performed in the midsagittal plane of the fetal profile. They are used mainly in the first trimester in screening for aneuploidies or in the detection of facial clefts and micrognathia. Some of these measurements are discussed in the following sections.
Nasal Bone Length
Reference ranges for nasal bone length in the fetus were reported in the second and third trimesters of pregnancy, and nasal bone has been described to be absent or short in fetuses with trisomy 21.12 This observation was adapted to aneuploidy screening at 11 to 14 weeks of gestation, and Cicero et al.2 demonstrated that nasal bones are hypoplastic or not ossified in the first trimester in the majority of fetuses with trisomy 212 (Figs. 9.15 and 6.1), and in other aneuploidies and syndromic conditions (Figs. 6.6, 6.8, 6.33, and 6.35).13 Assessment of the nasal bone is also used to improve the efficiency of the combined first-trimester screening for Down syndrome.13,14 Table 1.2 in Chapter 1 summarizes the essential criteria for an accurate nasal bone assessment in the first trimester.
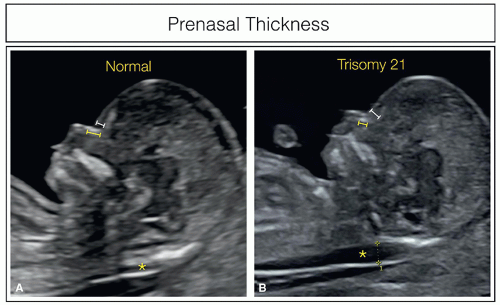
Prenasal Thickness
The observation that the skin of the forehead, called the “prenasal thickness,” is increased in the second trimester in
fetuses with trisomy 2115,16 has led to the use of this marker in the first trimester of pregnancy as well (Fig. 9.16).5,8,17 To reduce the false-positive rate of prenasal thickness measurement, the ratio of the prenasal thickness to nasal bone length was proposed5 (Fig. 9.16). In normal fetuses, the prenasal thickness is small and the nasal bone is relatively long, resulting in a ratio of approximately 0.6.5 In trisomy 21 fetuses in the first trimester, the prenasal thickness increases, whereas the nasal bone length decreases, resulting in a ratio >0.8.5
fetuses with trisomy 2115,16 has led to the use of this marker in the first trimester of pregnancy as well (Fig. 9.16).5,8,17 To reduce the false-positive rate of prenasal thickness measurement, the ratio of the prenasal thickness to nasal bone length was proposed5 (Fig. 9.16). In normal fetuses, the prenasal thickness is small and the nasal bone is relatively long, resulting in a ratio of approximately 0.6.5 In trisomy 21 fetuses in the first trimester, the prenasal thickness increases, whereas the nasal bone length decreases, resulting in a ratio >0.8.5
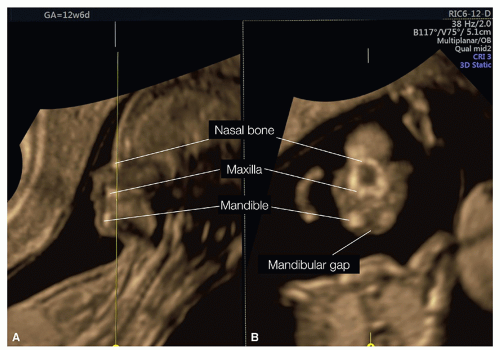 Figure 9.14: Three-dimensional ultrasound volume of the fetal face acquired transvaginally at 12 weeks of gestation and displayed in tomographic mode. In this figure, only two planes are displayed: plane A, showing a midsagittal plane of the head with facial profile, and plane B, obtained as the corresponding coronal plane at the level of the yellow line. Note that plane B shows the retronasal triangle view with the mandibular gap. See Figure 9.7 for details. |
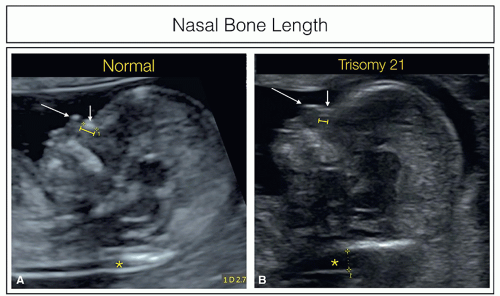 Figure 9.15: Midsagittal views of the fetal face showing the measurement of the nasal bone length in a normal fetus (A) and in a fetus with trisomy 21 (B). In more than half of the fetuses with trisomy 21, the nasal bone is either completely nonossified or, as in this case, poorly ossified, resulting in a short and thin appearance. Long arrows point to the nose tip and short arrows to the nasal skin. Nuchal translucency measurement is also seen (asterisk). Compare with Figure 1.3 in Chapter 1 and with Fig. 9.16. |
Maxillary Length
Fetuses with trisomy 21 have a flat profile due to midfacial hypoplasia, leading to the known feature of a protruding tongue. Measuring the maxillary length between 11 and 14 weeks of gestation is proposed as a method to quantify midfacial hypoplasia.3 The measurement is performed in a slightly parasagittal view of the facial profile and includes the mandibular joint.3 Maxillary length is short in fetuses with trisomy 21.3 Midfacial hypoplasia can also be assessed by the use of the frontomaxillary facial angle, which indirectly includes the maxilla.18 The frontomaxillary facial angle is discussed in the next section.
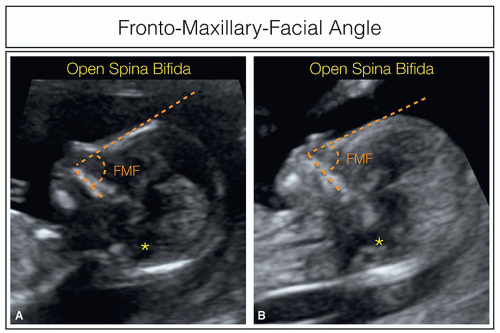
Frontomaxillary Facial Angle
The frontomaxillary facial (FMF) angle is the angle between the maxilla and forehead and in normal fetuses is quantified at 85° (±10°) (Fig. 9.17A).18 A wide FMF angle is reported in fetuses with trisomy 214,19 (Fig. 9.17B), whereas a narrow FMF angle is noted in fetuses with open spina bifida (Fig. 9.18).20 Abnormal FMF angles are also reported in fetuses with trisomy 18 with midfacial hypoplasia and micrognathia21 and in fetuses with trisomy 13 in association with holoprosencephaly.22 Caution should be used, however, in the evaluation of the FMF angle because slightly oblique views will introduce false-positive and negative results. Measurement of the FMF angle using 3D multiplanar rendering has been shown to improve its accuracy.18,23 The wide FMF angle in fetuses with aneuploidies is likely due to the short maxilla, whereas in spina bifida the narrow angle is probably due to the small flat head owing to the posterior shift of the brain and decreased fluid in the ventricles. Another facial angle is the maxilla-nasion-mandible (MNM) angle and uses the nasion as reference point of the intersection of the frontal and nasal bones.8,24 The MNM angle is defined as the angle between the maxilla-nasion line and the mandible-nasion line in the midsagittal plane of the face and can be used to identify fetuses at high risk for aneuploidies, micrognathia, and clefts.8
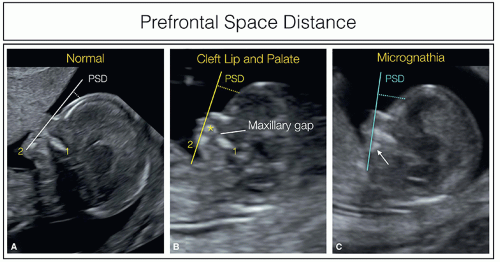
Prefrontal Space Distance
Prefrontal space distance (PSD) is obtained by drawing a line from the anterior aspect of both the mandible and maxilla and extended toward the fetal forehead (Fig. 9.19).6,7 The
PSD is calculated by the distance of the prenasal skin to this extended line (Fig. 9.19). The distance can have positive or negative values.6 PSD is abnormal in fetuses with aneuploidies, such as trisomies 21, 18, and 13,6 as well as in fetuses with micrognathia and clefts7 (Fig. 9.19).
PSD is calculated by the distance of the prenasal skin to this extended line (Fig. 9.19). The distance can have positive or negative values.6 PSD is abnormal in fetuses with aneuploidies, such as trisomies 21, 18, and 13,6 as well as in fetuses with micrognathia and clefts7 (Fig. 9.19).
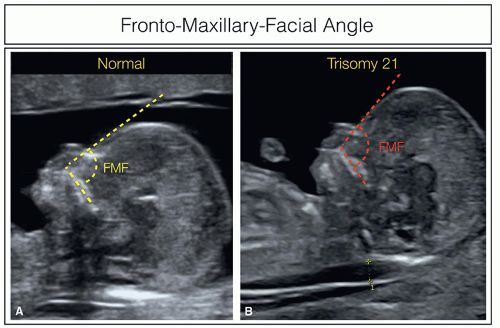 Figure 9.17: Midsagittal views of the fetal face showing the measurement of the fronto-maxillary-facial (FMF) angle in a normal fetus (A) and in a fetus with trisomy 21 (B). The FMF angle is measured in the midsagittal view of the face between the maxilla and the forehead, as shown in A and B. In the normal fetus (A), the angle is approximately 85° (yellow lines), whereas in the fetus with trisomy 21 (B), the angle is wider than 85° (red lines). Nuchal translucency measurement is also seen in fetus B. See also Figure 9.18. |
Orbit Size and Distances
To the best of our knowledge, no charts currently exist on the size of the orbit and the interorbital distances in the first trimester of pregnancy, and such measurements are not obtained routinely. Recently, a paper reported on the interlens distance, starting at 12 weeks of gestation.25
FETAL FACIAL ABNORMALITIES IN ANEUPLOIDIES AND IN CNS MALFORMATIONS
Fetal Profile in Aneuploidies
Trisomy 21 fetuses typically show an abnormal facial flat profile with an absent or hypoplastic nasal bone (Fig. 9.15), a short maxilla, an increased FMF angle (Fig. 9.17), and a thickened prenasal thickness (Fig. 9.16). Similar facial appearance can also be found in trisomy 18 fetuses, in addition to retrognathia and facial clefts. Trisomy 13 fetuses show severe facial anomalies due to their association with holoprosencephaly (Fig. 9.20) and/or with facial clefts. Ultrasound markers of aneuploidies, including facial abnormalities in the first trimester, are discussed in detail in Chapter 6.
Holoprosencephaly
Lobar and semilobar holoprosencephaly is often associated with facial abnormalities such as cyclopia, hypotelorism, proboscis, cebocephaly, agnathia-holoprosencephaly, nasal hypoplasia, and facial clefts.26 In most cases, the profile is severely abnormal, in addition to the abnormal head shape and brain. Figures 9.10 and 9.20 show abnormal profiles in fetuses with alobar holoprosencephaly. Holoprosencephaly is discussed in detail in Chapter 8.
Acrania/Anencephaly/Exencephaly
In acrania/anencephaly/exencephaly, the profile and the frontal view of the face have characteristic abnormalities with the presence of large eyes and small face. Facial profile views in Figure 9.21 show different aspects of the forehead region in acrania. Abnormalities in facial profiles in anencephaly/exencephaly are discussed in detail in Chapter 8.
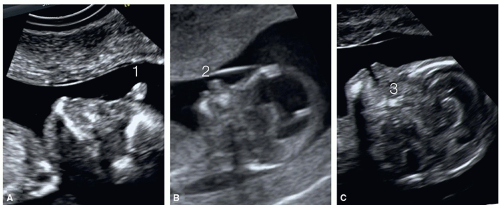 Figure 9.20: Midsagittal views of the fetal face in three fetuses (A-C) with alobar holoprosencephaly at 11, 12, and 13 weeks of gestation, respectively. In fetus A, no normal facial structures are identifiable, and a proboscis (1) can be seen in the midline. In fetus B, cebocephaly with an abnormal nose (2) is seen (compare with 3D image in Fig. 9.10). In fetus C, no maxilla (3) is seen in this midsagittal plane due to the presence of a large midline cleft.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|