The Fetal Urogenital System
INTRODUCTION
The first trimester examination of the fetal urogenital system primarily focuses on the demonstration of a fluid-filled bladder. When technically feasible or in specific high-risk conditions, visualization of both kidneys and fetal gender is attempted. With optimal imaging, and after the 12th week of gestation, evaluation of the fetal urogenital system is possible, but a conclusive diagnosis of normality requires confirmation later on in pregnancy, because some malformations are not visible until the second trimester or beyond. Several major urogenital malformations can be detected or suspected in the first trimester, however, and are discussed in this chapter. In a large prospective screening study for aneuploidies, including basic examination of fetal anatomy performed in 45,191 pregnancies, the detection of anomalies of the urogenital system in the first trimester was reported among the lowest of fetal malformations.1
EMBRYOLOGY
Understanding the embryogenesis of the urogenital system is important as it relates to the evaluation of normal and abnormal anatomy. The urogenital system develops from the intermediate mesoderm, which forms a urogenital ridge on each side of the aorta. The urogenital ridge develops cranially to caudally into the pronephros, mesonephros, and metanephros, respectively, representing three sets of tubular nephric structures. The pronephros, the most cranial set of tubules, develops in the third week of embryogenesis and regresses a week later. The mesonephros, located in the midsection of the embryo, gives rise to the mesonephric tubules and the mesonephric ducts (Wolffian duct). The mesonephric tubules regress, but the mesonephric ducts persist bilaterally and open into the cloaca. The mesonephric ducts give rise to the ureters, renal pelves, and bladder trigone. In the male, the mesonephric ducts also give rise to the vasa deferens, epididymis, and seminal vesicles. An outgrowth of the caudal portion of the mesonephric duct on each side forms the ureteric bud, which grows toward the metanephric blastema, a mesenchymal condensation of metanephros (Fig. 13.1). The definitive adult kidney is formed by the ureteric bud, which gives rise to the renal pelvis, infundibula, collecting ducts, and calyces, and the metanephric tubules, which form the nephrons with capillary invagination. With the growth of the embryo, the kidney ascends from the pelvis into the upper retroperitoneum, and failure of renal migration results in a pelvic kidney.
At about the seventh week of embryogenesis, a urogenital membrane grows caudally, dividing the cloaca into ventral (urogenital sinus) and dorsal (rectum) components. The urethra is derived from the endoderm at the ventral urogenital sinus. An invagination of ectoderm in the most distal part of the urethra in males joins with the endodermal epithelium of the proximal urethra to create a continuous channel. Differentiation of the external genitalia into male and female occurs between the 8th and 11th week of embryogenesis. Detailed
development of the gonads and external genitalia is beyond the scope of this chapter.
development of the gonads and external genitalia is beyond the scope of this chapter.
 Figure 13.1: Schematic drawing of the embryologic development of the urogenital system at around the seventh menstrual week. See text for details. |
NORMAL SONOGRAPHIC ANATOMY
Visualization of the fetal urogenital system in the first trimester is performed by the identification of the bladder and when possible the kidneys, which can be seen on ultrasound as early as 10 weeks of gestation with high-resolution transvaginal transducers.
 Figure 13.3: Axial views of the fetal lower pelvis in three fetuses (A-C) at 13, 13, and 12 weeks of gestation, respectively. Note that the bladder is seen in various stages of filing; with more filling in fetus A as compared to fetuses B and C. The bladder is best demonstrated in this axial view at the level of the pelvis. The addition of color Doppler, as shown in Figure 13.4, improves bladder visualization. |
Urinary Bladder
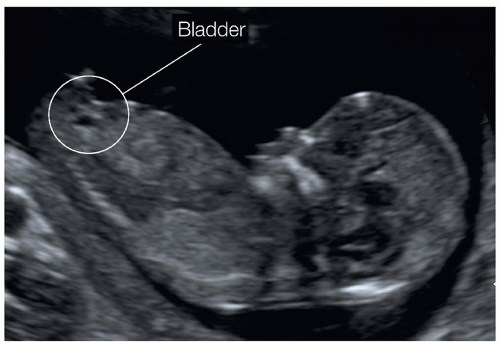
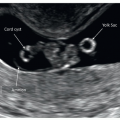
The fetal bladder appears as an anechoic structure in the anterior lower pelvis. The bladder is easily seen in the sagittal view of the fetus, in the same plane used for the crown-rump length (CRL) measurement (Fig. 13.2). The axial plane of the fetal pelvis also demonstrates the fetal bladder in a central-anterior location (Fig. 13.3). Visualization of the bladder in the first trimester is aided by color Doppler ultrasound, with the identification of the surrounding umbilical arteries (Fig. 13.4). Although the fetal stomach is almost always filled with fluid, the fetal bladder is occasionally empty in the first trimester and thus maybe difficult to image. When the fetal bladder is not clearly demonstrated in the first trimester, the ultrasound examiner should reassess for the presence of a bladder few minutes later to allow for bladder filling. The authors therefore recommend that visualization of the fetal bladder is performed at the beginning of the first trimester ultrasound examination in order to allow time for bladder filling if the bladder is not visible then. The longitudinal length of the normal bladder should be less than 7 mm in the first trimester (Fig. 13.5).2,3 The fetal bladder is seen on ultrasound in about 88% of fetuses at 12 weeks of gestation and in 92% to 100% of fetuses at 13 weeks of gestation.3,4
Kidneys and Adrenal Glands
With transabdominal ultrasound, the fetal kidneys are generally difficult to visualize and differentiate from the surrounding bowel in the first trimester. Visualization of the fetal kidneys by the transabdominal approach in the first trimester is improved
with the use of high-resolution transducers along with optimal scanning conditions (Figs. 3.2, 3.4, 13.6, and 13.7). The transvaginal approach substantially improves visualization of the fetal kidneys in the first trimester because of the proximity of the transducer to the fetal abdomen and increased resolution of the probe (Figs. 3.2 and 13.8).4 The fetal kidneys appear in the first trimester as rounded, slightly bright structures in the posterior abdomen lateral to the spine, with the renal pelves noted as anechoic circles, centrally within the renal tissue (Figs. 13.7 and 13.8). Cranial to both kidneys, the slightly hypoechoic and large adrenal glands are seen (Fig. 13.7). The length of the adrenal gland is less than half the length of the kidney.5 Visualization of the fetal kidneys in the first trimester can be achieved in the coronal, sagittal, or axial planes (Fig. 13.9) of the fetal abdomen. The coronal plane of the fetal abdomen is the optimal plane for first trimester imaging of the kidneys in our experience (Figs. 13.7, 13.8B, and 13.10). This coronal plane is also helpful for the demonstration of unilateral or bilateral renal agenesis, and a more anterior view can demonstrate the presence of a horseshoe kidney (see below). Color Doppler can also be added to demonstrate the right and left renal arteries arising from the descending aorta (Fig. 13.10). The fetal kidneys can be identified in 86% to 99% of fetuses at 12 weeks of gestation and in 92% to 99% of fetuses at 13 weeks of gestation.4,6
with the use of high-resolution transducers along with optimal scanning conditions (Figs. 3.2, 3.4, 13.6, and 13.7). The transvaginal approach substantially improves visualization of the fetal kidneys in the first trimester because of the proximity of the transducer to the fetal abdomen and increased resolution of the probe (Figs. 3.2 and 13.8).4 The fetal kidneys appear in the first trimester as rounded, slightly bright structures in the posterior abdomen lateral to the spine, with the renal pelves noted as anechoic circles, centrally within the renal tissue (Figs. 13.7 and 13.8). Cranial to both kidneys, the slightly hypoechoic and large adrenal glands are seen (Fig. 13.7). The length of the adrenal gland is less than half the length of the kidney.5 Visualization of the fetal kidneys in the first trimester can be achieved in the coronal, sagittal, or axial planes (Fig. 13.9) of the fetal abdomen. The coronal plane of the fetal abdomen is the optimal plane for first trimester imaging of the kidneys in our experience (Figs. 13.7, 13.8B, and 13.10). This coronal plane is also helpful for the demonstration of unilateral or bilateral renal agenesis, and a more anterior view can demonstrate the presence of a horseshoe kidney (see below). Color Doppler can also be added to demonstrate the right and left renal arteries arising from the descending aorta (Fig. 13.10). The fetal kidneys can be identified in 86% to 99% of fetuses at 12 weeks of gestation and in 92% to 99% of fetuses at 13 weeks of gestation.4,6
 Figure 13.4: Axial views in color Doppler of the fetal lower pelvis in two fetuses (A and B) at 12 weeks of gestation. Note that the addition of color Doppler shows the umbilical arteries surrounding the bladder. This axial view is helpful for bladder imaging and also for confirming the presence of a three-vessel umbilical cord. Compare with Figures 3.10, 13.33A and 13.34A. |
Genitalia
Although genitalia can be well seen either in an axial view of the pelvis or in the midsagittal view during the measurement of the CRL, reliable differentiation of fetal gender is of limited
diagnostic accuracy in the first trimester. Embryologically, sex differentiation is not fully completed until about the 11th week of gestation, and thus, sex determination on ultrasound is relatively inaccurate before the 12th week of gestation. The ability to identify fetal gender on ultrasound increases with advancing gestation, and the accuracy is enhanced after the 13th week of gestation or with CRL measurements greater than 70 mm. The midsagittal view of the fetus is most reliable for the identification of gender in the first trimester because it shows a caudally directed clitoris in females (Fig. 13.11A and B)
and a cranially directed penis in males (Fig. 13.11C and D). Labia majora and minora appear as parallel lines in females when compared to a nonseptated dome-shaped structure, corresponding to the scrotum in males. Accuracy of fetal gender determination in the first trimester varies from 60% to 100%, being inaccurate before 12 weeks, and reaches >95% after 13 weeks of gestation.7
diagnostic accuracy in the first trimester. Embryologically, sex differentiation is not fully completed until about the 11th week of gestation, and thus, sex determination on ultrasound is relatively inaccurate before the 12th week of gestation. The ability to identify fetal gender on ultrasound increases with advancing gestation, and the accuracy is enhanced after the 13th week of gestation or with CRL measurements greater than 70 mm. The midsagittal view of the fetus is most reliable for the identification of gender in the first trimester because it shows a caudally directed clitoris in females (Fig. 13.11A and B)
and a cranially directed penis in males (Fig. 13.11C and D). Labia majora and minora appear as parallel lines in females when compared to a nonseptated dome-shaped structure, corresponding to the scrotum in males. Accuracy of fetal gender determination in the first trimester varies from 60% to 100%, being inaccurate before 12 weeks, and reaches >95% after 13 weeks of gestation.7
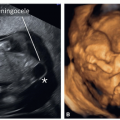
 Figure 13.6: Right (A) and left (B) parasagittal planes of a fetus at 13 weeks of gestation obtained with a high-resolution transabdominal transducer showing fetal kidneys. In the right parasagittal plane (A), the right kidney can be seen and appears as echogenic as the lung and is separated from the diaphragm by the hypoechoic adrenal gland. In the left parasagittal plane (B), the left kidney is seen under the left adrenal gland and stomach. The kidneys can also be imaged in the first trimester in a coronal plane of the abdomen and pelvis (see Figs. 13.7 and 13.8). |
 Figure 13.8: Parasagittal (A) and coronal (B) planes of the abdomen and pelvis, obtained transvaginally in two fetuses at 13 (A) and 11 (B) weeks of gestation, respectively. Note in A and B that the kidneys are better visualized using the transvaginal approach. Fetal kidneys typically appear more echogenic in the first trimester, especially with the transvaginal approach, and thus it is difficult at times to differentiate normal from abnormal kidney echogenicity in early gestation (see Fig. 13.28). |
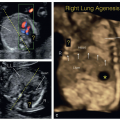
 Figure 13.10: Coronal plane of the fetal abdomen and pelvis with color Doppler in two fetuses at 13 (A) and 12 (B) weeks of gestation. Image in A is obtained transabdominally and image in B is obtained transvaginally. The use of color Doppler in a coronal plane of the abdomen and pelvis, as shown here in A and B, demonstrates the two renal arteries arising from the aorta. This approach is helpful in the presence of suspected unilateral or bilateral renal agenesis as the absence of a kidney is associated with an absence of the corresponding renal artery (see Figs. 13.33 and 13.34). |
UROGENITAL SYSTEM ABNORMALITIES
Megacystis and Lower Urinary Tract Obstruction
Definition
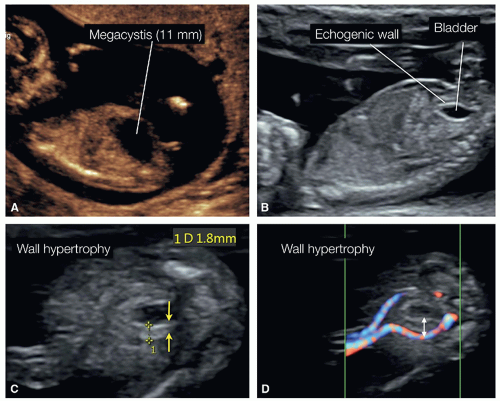
The term megacystis is used to describe an unusually dilated bladder (Figs. 13.12 and 13.13). Megacystis is defined in the first trimester by a longitudinal bladder diameter of 7 mm or more obtained on a midline sagittal plane of the fetus.2,3 Spontaneous resolution of megacystis has been described when the longitudinal bladder length is less than 15 mm and in the absence of associated chromosomal abnormalities.8 In the first large study on megacystis between 10 and 14 weeks,3 145 fetuses with a bladder length ≥7 mm were evaluated: In the group with bladder length between 7 and 15 mm (Fig. 13.12), the incidence of chromosomal defects was 23.6% versus 11.4% for a bladder diameter >15 mm (Figs. 13.13 and 13.14).3 In the remaining group with bladder diameter between 7 and 15 mm and normal chromosomes, 90% showed spontaneous resolution and 10% developed renal problems. In contrast, in all fetuses with a bladder diameter
>15 mm and normal chromosomes, megacystis progressed into obstructive uropathy (Fig. 13.14).3
>15 mm and normal chromosomes, megacystis progressed into obstructive uropathy (Fig. 13.14).3
 Figure 13.15: A: A midline sagittal plane of a fetus at 12 weeks of gestation with megacystis, with a longitudinal bladder diameter of 12 mm. B: The corresponding axial plane at the level of the pelvis at 12 weeks of gestation showing the presence of a keyhole sign, suggesting a posterior urethral valves. The fetus had no additional anatomic or chromosomal abnormalities. C: The follow-up ultrasound at 14 weeks of gestation showing resolution of the megacystis with a longitudinal bladder diameter of 6 mm. D: An axial plane of the pelvis in color Doppler at 18 weeks of gestation showing normal bladder and umbilical arteries with no bladder wall hypertrophy, as evidenced by the proximity of the umbilical arteries to the internal bladder wall (arrows). Resolution of first trimester megacystis is a common event. Compare with Figure 13.16. |
As noted, megacystis in the first trimester can be transient (Figs. 13.15 and 13.16), but can also be a sign of a lower urinary tract obstruction (LUTO). LUTO, previously referred to as bladder outlet obstruction, is an abnormality involving an obstruction of the lower urinary tract at the level of the urethra, resulting from either a membrane-like structure (valves) in the posterior urethra or urethral atresia. LUTO is usually sporadic, and when severe, it is associated with oligohydramnios, pulmonary hypoplasia, and renal damage. Posterior urethral valves (PUV), which represent the most common form of LUTO, affect males almost exclusively with varying degrees of obstruction. Urethral atresia on the other hand occurs in males and females and is extremely rare.
PUV occurs in about 1:8,000 to 1:25,000 of males,9,10 and its etiology is thought to result from either an exaggerated development of the urethral folds (type 1 and 2) or failure to create a continuous channel within the urethra with the persistence of an obstructive urogenital membrane (type 3).10 Prenatal therapeutic interventions with placement of a vesicoamniotic shunt or ablation of the obstructive tissue through cystoscopy is reserved to the second trimester of pregnancy. Transient megacystis and PUV will be the primary focus of discussion in this segment.
Ultrasound Findings
Megacystis is probably the easiest and most commonly diagnosed abnormality of the genitourinary system in the first trimester. It is based on the identification of a large bladder, measuring 7 mm or more in sagittal view (Figs. 13.12, 13.13, 13.14 and 13.15). In some cases of resolving megacystis, a thickened bladder wall may still be observed (Fig. 13.16C and D). The presence of progressive obstructive uropathy is common when the longitudinal bladder length measures greater than 15 mm (Figs. 13.13 and 13.17).3
The sonographic identification of PUV is possible in the first trimester, especially in severe cases (Figs. 13.17 and 13.18). In the first trimester, amniotic fluid is commonly normal in PUV cases, and the diagnosis is typically suspected by the presence of an enlarged bladder (megacystis) (Figs. 13.17 and 13.18). PUV in the first trimester is often associated with hydronephrosis and renal dysplasia in severe cases (Figs. 13.19 and 13.20). PUV markers of poor prognosis, such as the presence of renal cortical cysts and increased renal echogenicity, are already present in the first trimester (Fig. 13.19), but their absence cannot predict a good prognosis. The keyhole sign, related to a dilated proximal urethra, supports the diagnosis of PUV in the first trimester (Figs. 13.15B, 13.17D, 13.20B, and 13.21B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree