Hip Checklists
 1
1
Radiographic examination
Hip
AP pelvis
AP hip
Frog leg-view hip
Groin lateral hip
Femur
AP hip
AP femoral shaft and condyles
Lateral femoral shaft and condyles
Oblique femoral shaft
 2
2
Common sites of injury in adults
Elderly – low-impact trauma (fall from standing height)
Femoral neck
Intertrochanteric
Greater trochanter
Pelvic fractures presenting as hip fractures
Pubic rami
Iliac wing
Adult – R/O pathologic fracture
Basicervical fractures
Lesser trochanteric avulsions
Transverse subtrochanteric fractures
Adult – high-impact trauma (MVC)
Posterior hip dislocation
Femoral neck
Subtrochanteric
Femoral shaft
 3
3
Hip fractures rare in children and adolescents
Pelvic fractures about hip common
Pubic rami
Iliac wing
Occasional
Femoral neck
Posterior dislocation
Proximal femoral epiphyseal separation rare
Slipped capital femoral epiphysis (SCFE)
 4
4
Injuries likely to be missed
Low-impact trauma – elderly
Fine, subtle fractures
Femoral neck
Intertrochanteric
High-impact trauma – all ages
Proximal injuries of the hip in association with femoral shaft fractures
Posterior dislocation of hip
Fracture of acetabulum
Fracture of femoral neck
 5
5
Where else to look when you see something obvious
| Obvious | Look for |
|---|---|
| Fracture of femoral shaft | Posterior dislocation of hip |
| Fracture of acetabulum | |
| Fracture of femoral neck | |
| Fracture of distal femur (condyles) | |
| Fracture of patella | |
| Fracture of greater trochanter | Intertrochanteric extension (MRI) |
 6
6
Where to look when you see nothing at all
Search for alternative diagnoses, fractures of
Iliac crest
Pubic rami
Acetabulum
Greater trochanter of proximal femur
Need to rule out obscure/not apparent femoral neck or intertrochanteric fracture
If questionable radiographic findings noted – CT often sufficient
If x-rays negative – MRI required
Hip – The Primer
 1
1
Radiographic examination
Hip
AP pelvis
AP hip
Frog leg-view hip
Groin lateral hip
Femur
AP hip
AP femoral shaft and condyles
Lateral femoral shaft and condyles
Oblique femoral shaft
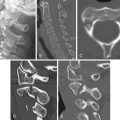
A radiographic examination of the traumatized hip should include the four standard views listed above. An AP of the pelvis ( Fig. 9-1 A ) is included to survey the surrounding bony pelvis for fractures (i.e., pubic rami and iliac wings), which can mimic hip fractures. The AP view of the hip ( Fig. 9-1 B ) should be obtained with the hip in internal rotation to place the femoral head and neck in profile. If the patient’s foot is in external rotation and he or she is unable to rotate the foot, the AP view should be taken as the patient lies, because with displaced fractures of the femoral neck the hip is typically held in external rotation. If this view shows no evidence of hip fracture, the toes should be brought together by wrapping the forefeet in a towel to place the hip in internal rotation, and a repeat AP view should be obtained. The frog leg-view ( Fig. 9-1 C ) is obtained with leg abducted and externally rotated, in effect, resulting in a modified lateral view of the proximal femur. The groin lateral ( Figs. 9-1 D and 9-1 E ) is an optional view of the femoral head and neck that better demonstrates posterior rotation of the femoral head in the presence of subcapital fractures.

The AP view with slight internal rotation of the hip ( Fig. 9-2 A ) best profiles the head and neck junction, which facilitates identification of fractures of the femoral neck and intertrochanteric femur. With a displaced fracture of the femoral neck the distal fragment lies in external rotation, and the femur is drawn proximally ( Fig. 9-2 B ). External rotation of the hip on the AP view in the absence of a femoral neck fracture is, unfortunately, a common occurrence ( Fig. 9-2 C ). External rotation of the hip foreshortens the femoral neck, and the underlying greater trochanter obscures the femoral head and neck junction. Fractures of the femoral neck are difficult to identify on such views.

Subcapital fractures, particularly nondisplaced fractures, are obscured and readily overlooked ( Fig. 9-3 A ) with external rotation. A repeat PA view should be obtained with slight internal rotation of the femur ( Fig. 9-3 B ). Note that an impacted subcapital fracture is now visible. An even more striking example of difficulty in seeing fractures on the AP view with external rotation is shown in Fig. 9-4 . On the initial AP view with external rotation no fracture is seen or even suspected ( Fig. 9-4 A ). However, the repeat, properly positioned AP view clearly depicts a widely separated fracture of the greater tuberosity ( Fig. 9-4 B ) that is not apparent on the initial examination.


 2
2
Common sites of injury in adults
Elderly – low-impact trauma (fall from standing height)
Femoral neck
Intertrochanteric
Greater trochanter
Pelvic fractures presenting as hip fractures
Pubic rami
Body of the pubis
Iliac wing
Adult – R/O pathologic fracture
Basicervical fractures
Lesser trochanteric avulsions
Transverse subtrochanteric fractures
Adult – high-impact trauma (MVC)
Posterior hip dislocation
Femoral neck
Femoral shaft
Pattern of search
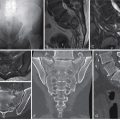
A diagram of the hip ( Fig. 9-5 A ) pinpoints the common sites of fracture in adults as identified by red lines. Your pattern of search should include all sites: subcapital, intertrochanteric, and greater trochanteric.

Fractures of the hip are most commonly encountered in the elderly in association with generalized osteoporosis. They occur in low-impact trauma, usually a fall from a standing height. The most common is a subcapital fracture of the femoral neck. Displaced subcapital fractures are held in external rotation, and the femoral shaft is drawn proximal, shortening the femur ( Fig. 9-5 B ). The groin lateral view ( Fig. 9-5 C ) shows the posterior rotation and displacement of the femoral head. Follow the anterior cortex of the femur to the fracture. Displaced fractures of the femoral neck result in devascularization of the femoral head, and therefore a hemiarthroplasty ( Fig. 9-5 D ) is required.
Subcapital fractures
Most subcapital fractures are impacted; two cases are shown ( Figs. 9-6 A and 9-6 B-E ). The head fragment is usually rolled posterolateral, valgus ( Figs. 9-6 A and 9-6 B ), or, less commonly, posteromedial, varus (see Fig. 9-7 ) and impacted on the femoral neck. Disruption of the medial cortex of the femoral neck ( Fig. 9-6 A ) is variable and often not apparent ( Fig. 9-6 B ). CT confirms the diagnosis in questionable cases ( Fig. 9-6 C , coronal reconstruction, and Fig. 9-6 D , axial). Impacted fractures are treated by screw fixation ( Fig. 9-6 E ) because the majority of the blood supply to the femoral head remains intact and therefore the head is viable.