“Starting in Wuhan, China, followed quickly in the United States in January 2020, an outbreak of a novel coronavirus, or COVID-19, escalated to a global pandemic by March. Significant disruptions occurred to breast imaging, including deferred screening mammography, triaging diagnostic breast imaging, and changes in breast cancer care algorithms. This article summarizes the effect of the global pandemic—and efforts to curtail its spread—on both breast cancer care and on breast imaging practices including effects on patients, clinical workflow, education, and research.”
Key points
- •
The COVID-19 pandemic starting in the United States in 2020 has had practice-changing effects on cancer care, clinical workflow, education, research, and radiology finances.
- •
Significant volume reductions and delays occurred to breast imaging, with screening mammography being the hardest hit.
- •
Long-term outcomes from changes in breast cancer management algorithm during the pandemic are yet to be determined.
- •
Increased telehealth and telecommuting will likely continue after the pandemic is over in some fashion.
- •
Radiology practices and hospitals sustained large financial ramifications from the effects of the pandemic.
Introduction
Starting in Wuhan, China, followed quickly in the United States in January 2020, an outbreak of a novel coronavirus, or COVID-19, escalated to a global pandemic by March. Significant disruptions occurred to breast imaging, including deferred screening mammography, triaging diagnostic breast imaging, and changes in breast cancer care algorithms. This article summarizes the effect of the global pandemic—and efforts to curtail its spread—on both breast cancer care and on breast imaging practices including effects on patients, clinical workflow, education, and research.
Initial response: routine health care deferred
The approach to the handling of COVID-19 has been fluid, as understanding of the pathophysiology, clinical spectrum and severity of illness, and possible preventions and treatment of the virus have evolved. ,
Early Response: Concerns for Mammography in COVID-19
Shortly after the first outbreaks in the United States on the Diamond Princess Cruise Ship, in Seattle and New York, on the heels of large outbreaks in China and Italy, the main prevention strategy of “social distancing” was adopted by the World Health Organization. By April 2020, 33 states had state mandated “stay-at-home-orders.” The Centers for Disease control (CDC) issued recommendations to reschedule nonurgent patient care and delay screenings in an effort to minimize risks to patients and health care workers (HCWs). Although social distancing measures varied regionally, most of the school systems, churches, and businesses were closed in March or April 2020, often moving to virtual encounters. Leaders in breast imaging and radiology departments discussed the best ways to protect patients, protect HCWs, and conserve personal protective equipment (PPE) and ventilators to be used for patients with COVID-19. Many sites began rescheduling screening mammography patients, some diagnostic or biopsy cases, or even delaying breast surgeries in an ad hoc fashion. Varied interpretations of the CDC, WHO, and the varied state policies led to nonuniform disruptions in patient care, in some cases varying within the same large cities.
On March 24th, news reports of potential danger to mammography technologists from work exposures were released, with a death of a mammography technologist in Georgia from COVID-19, a possible work exposure. HCWs were confirmed to be high risk for COVID-19 infections (up to 10%) from initial data in early outbreaks in China, Italy, and Spain. The National Comprehensive Cancer Network (NCCN) issued guidelines for health care worker safety early in the pandemic, based on WHO recommendations. In a study rating different professions’ risk of contracting COVID-19 from work, radiology technologists were one of the highest (a score or 84 out of 100), and then sonographers (80 out of 100). Mammography technologists likely have an even higher risk, as they are unable to maintain social distancing (2 m or 6 feet) during positioning.
Quickly, breast radiologists and technologists had palpable concerns regarding the need to protect HCWs and patients during screening, and firm statements were released by national organizations with the American Society of Breast Surgeons (ASBrS) and American College of Radiology (ACR) Joint Statement on Breast Screening Exams During the COVID-19 Pandemic and the Society of Breast Imaging Statement on Breast Imaging during the COVID-19 Pandemic, all released later in March, 2020, and recommending to “postpone all breast screening exams (to include screening mammography, ultrasound, and MRI) effective immediately” as well as to discontinue routine and nonurgent breast health appointments. ,
Moreover, shortages of PPE existed, and so technologist and radiologists could not uniformly be masked, with only 35.3% (60 of 170) of radiology practices stating they had an adequate supply and 29.4% reporting that PPE supplies were low and needed to rationed.
A More Standardized Approach to Deferred Care
By March, the Canadian Society of Breast Imaging and Canadian Association of Radiologists Joint Position Statement on COVID-19 recommended that all screening mammography and MR imaging be deferred for at least 6 to 8 weeks and suggested triaging the diagnostic cases, deferring ones that were not highly suspicious for cancer. The Society of Breast Imaging followed suit with a statement that was broader and less prescriptive but also recommended delaying screening by “several weeks or a few months.” Other international societies published similar statements. ,
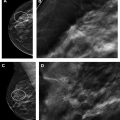
Multidisciplinary care algorithms changed the management of breast cancer during the pandemic in response to need to balance the urgency of care against the risks to patients and HCWs secondary to potential COVID-19 exposures. Surgeries were postponed both to limit COVID-19 transmission as well as to preserve resources such as ventilators, PPE, and hospital beds. The American College of Surgeons (ACS) and the Society of Surgical Oncology released triage guidelines recommending an interim cancellation of most routine surgeries, while still performing breast surgeries for those in more urgent cases. , Some centers, such as Magee-Breast Cancer Program and Johns Hopkins published multidisciplinary algorithms of how best to triage patients with breast cancer, broken down by subtypes. , Other published tools suggested risk-stratifying patients for breast surgery with the purpose of causing few deleterious effects in patients recommended for postponement.
In early April, a multidisciplinary group of breast cancer experts in the United States formed the COVID-19 Pandemic Breast Cancer Consortium and released its recommendations for prioritization, treatment, and triage of patients with breast cancer during the COVID-19 pandemic. The panel represents a joint collaboration from the ASBrS, the National Accreditation Program for Breast Centers (NAPBC), the NCCN, the Commission on Cancer, and ACR. The main goals of the Consortium recommendations were to “preserve hospital resources for virus-inflicted patients by deferring BC treatments without significantly compromising long-term outcomes for individual BC patients”. Patients were placed into categories based on severity of symptoms or illnesses with algorithms for chemotherapy and surgery outlined based on disease process.
Reopening of routine care
By July 2020, as the pandemic proved lasting and PPE supplies improved nationwide, consensus guidelines shifted to avoid delays in care and focused instead on how to better protect patients and workers. Leaders in breast cancer made evidence-based pleas to cease labeling patients with cancer as a high-risk population in order to avoid delays in their diagnosis and treatment. Numerous consensus statements and guidelines regarding how to best balance the risks of COVID-19 transmission to patients and HCWs against the risks of delaying care have been published. The European Society for Medical Oncology Guidelines include increasing telehealth appointments (noting in person visits are needed for new patients with cancer or urgent infections/postoperative complications) and specific guidance for management and advised that the risk/benefit balance for most patients favored continued administration of systemic therapies and chemotherapies, with additional precautions when possible (eg, choosing less immunosuppressive therapies, regimens requiring fewer appointments). Numerous other guidance documents have emerged fluidly including from American Society of Clinical Oncology (ASCO) and an online resource from ASCO, and others globally. ,
Although the recommendations for the management of breast cancer change the order and timing of breast cancer treatments, the goals have remained to change these algorithms in ways that do not affect long-term outcomes or chances for a cure. For example, surgery should remain the primary option for small triple-negative breast cancers that did not require chemotherapy based on pre-COVID-19 algorithms. In addition, patients with progressive disease on medical therapy should have surgery. Further patients who are competing their neoadjuvant regimens or patients who did not respond to neoadjuvant therapy should receive surgery.
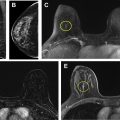
Prophylactic measures were implemented with guidance from the CDC, for protecting patients and HCWs, including social distancing where possible, masking both patients and HCWs, decreasing the number of scheduled patients, increasing space in waiting areas, and implementing disinfection protocols. Nearly all imaging centers implemented preappointment screening for symptoms of COVID-19, most requiring temperature screening at some point during the pandemic and a few even required COVID-19 negative testing before a breast interventional procedure (although many centers required COVID-19 negative testing before breast surgeries).
Changes in Food and Drug Administration inspections during COVID-19
Initially, the FDA halted inspections of mammography facilities required by the Mammographic Quality Standards Act in mid-March, 2020. In addition, the ACR granted automatic extensions and halted in-person inspections for sites where accreditation was expiring. As the reopening phase began, the FDA announced that it would restart inspections at facilities in locations that were not as affected by the pandemic on July 20th, although it did not actually start them then. It recommended that state inspections could start based on individual state guidance at the end of June 2020, guided by an advisory system to take into account the extent of the outbreak in that location combined with how critical the inspection would be.
Breast cancer as a comorbidity for COVID-19 severe outcomes/fatalities
Initially, concern existed that patients with breast cancer, especially advanced or metastatic breast cancer, may be more susceptible to severe outcomes with COVID-19. Many of the most common chemotherapy regimens used to treat breast cancer are known to cause immunosuppression. Further, patients undergoing cancer care have more visits and therefore more exposures to HCWs and patients, potentially making them more at risk of being infected with COVID-19. , Initial studies from Wuhan, China showed worse outcomes from COVID-19 in patients with cancer and suggested caution with cancer care during the pandemic. In one study of 1524 patients from the Wuhan outbreak, patients with cancer had more than double the risk of contracting COVID-19 than patients without (odds ratio [OR], 2.31; 95% confidence interval [CI], 1.89 to 3.02). In another early study from the Wuhan experience, the relative risk of dying or being admitted to the intensive care unit with COVID-19 in patients with cancer was 5.4 (95% CI 1.8–16.2). Moreover, patients with cancer had a higher relative risk of requiring intubation, across all age ranges. The mortality rate of COVID-19 in patients with cancer has ranged from 11% to 28% in reported studies, compared with the 1.4% mortality rate reported in the general population from the initial Wuhan studies. However, not all patients with cancer have the same risks, as a patient with an early stage breast cancer may not have the COVID-19 risks as a patient with end-of-life stage IV breast cancer. This was confirmed by one study of 900 patients with cancer and COVID-19 that found that having active cancer that was progressing (as opposed to remission) and having a worse performance status were associated with increased risk of mortality.
As the pandemic has unfolded, registries for patients with cancer and COVID-19 have been developed in an attempt to better understand the risk to patients with cancer, as initial reports on outcomes were limited to single institutional or smaller studies. An international database was established to study the risks of COVID-19 on patients with cancer from the United States, Canada, and Spain with underlying cancer (the COVID-19 and Cancer Consortium Database or CCC19). And ASCO developed its own registry to be able to share data rapidly and contribute to evidence-based decision-making for patients with cancer during the pandemic.
Initial reports from mid-March through mid-April of the CCC19, including more than 900 patients with cancer (21% breast cancer) and COVID-19 found that although the 30-day all-cause mortality for the entire population with cancer and COVID-19 was high, associated with both general and cancer-specific risk factors, the actual risk in patients with solid tumors (ie, breast cancer) was not significantly higher. This study also confirmed recent cancer surgery did not affect the mortality rate from concurrent infections with COVID-19. A large cohort study of 800 patients with cancer with COVID-19 in the United Kingdom (UK Coronavirus Cancer Monitoring Project), at a similar time frame of the pandemic, found that although the mortality rate was 28%, when adjusted for age and other comorbidities, the presence of cancer alone did not increase the mortality from COVID-19. Importantly, the use of chemotherapy before COVID-19 infection did not affect mortality, neither did the use of hormonal, targeted, and, immune therapies, or radiation.
Thus, although it may be possible that some patients with cancer have a propensity toward worse outcomes with COVID-19, it does not seem likely that cancer treatments such as chemotherapy, hormonal therapy, radiation, and surgery predispose patients to more serious outcomes from COVID-19. If care is taken for protective measures for the patients and HCWs as outlined in different care algorithms, breast cancer treatment should continue during the pandemic, especially in light of the unknown timeframe of the crisis.
Effects of delaying care on patients with breast cancer
Not only did multidisciplinary care algorithms force patients into delaying care during the pandemic but patients also self-selected to delay care. Nearly 4 out of 10 patients said the economic changes from the pandemic affected their ability to pay for medical care. A survey by ACEP demonstrated almost one-third of patients (29%) delayed or avoided going to the emergency room in March/April 2020 in order to avoid COVID-19 exposures. Four out of five patients were fearful of contracting the virus from a patient or HCW if they did go. Greater than 81% of survey participants acknowledged practicing social distancing. In an Italian study, during the height of the outbreak, there was a significant increase in patients refusing to undergo diagnostic appointments and breast biopsies at a major cancer center.
In another 600 breast care patients surveyed, almost 80% stated they had routine and follow-up appointments delayed, two-thirds had reconstruction surgery delayed, and 60% had delayed diagnostic imaging. Therapies that required in-person visits to the hospital (radiation, chemotherapy infusion, and surgical lumpectomies) were more likely to be delayed than those that could be obtained through telehealth appointments or a prescription pick-up. Medicare and Medicaid Services and private insurers expanded telehealth benefits to patients covering increased virtual visits. On average, about 30% of patients experienced delays in the mainstays of breast cancer treatment including lumpectomies, radiation therapy, and chemotherapy. Breast cancer surgeries declined significantly during the early parts of the global pandemic. In data from 55 breast centers in 27 states, it was noted that the average decline in breast surgery clinic appointments over the first few weeks was 21% with a nadir of 40% from baseline and a near 20% decline in new breast cancer surgery consultations in the surgery clinics. Similarly, breast cancer genetics appointments declined, ranging between 25% and 30%. In one study from Wuhan, China, more than half of the patients receiving radiation therapy were unable to complete their regimens during the lockdowns. The pandemic increased the use of neoadjuvant and hormonal therapies before surgery, as well as increased genotypic profiling, secondary to deferrals of surgeries. In another study from the Netherlands one-third of patients noted that the pandemic affected their cancer care, with most of these noting a shift to telehealth consultations. Chemotherapy was also affected in about one-third of these patients.
The long-term physical and psychosocial ramifications of these delays remain to be determined. One study demonstrated that more than half of the patients with cancer were concerned the delays or discontinuation of care during the pandemic affected their outcomes. Oncologic patients noted anxieties regarding whether they were at increased risk of worse outcomes with COVID-19, as well as anger and worry from delays or interruptions in their care during COVID-19. Some patients even stated that the changes in their care encountered sounded “like a death sentence” or made them “feel like my care and health aren’t important to you”. These patient perceptions, whether accurate or not, will need to be addressed as the pandemic unfolds. ,
The mental health effects of limiting care during this pandemic, and potentially in future crises, on both cancer specialists and patients, who are used to unlimited resources for health care, may be far reaching. Having consensus guidelines to guide fair decision-making and developing empathic communication with regard to these issues is important. Education and shifts in mindsets to prioritize the maximum health benefit for the community over the individual may be necessary in a country used to unlimited resources. Guidelines have been developed for low resource communities that may prove useful. ,
It is unclear what effects these COVID-19 provoked changes in cancer screening and management will have on long-term cancer outcomes. In the United States, an estimated additional 87,001 deaths occurred in March and most of April 2020 compared with the last 6 years, of which 35% (30,755) were not directly attributable to COVID-19 (and in 14 states, >50% of excess deaths frame were not attributable). Almost half (48%) of US people surveyed had a family member who had delayed medical care during the pandemic, with 10% stating that that member’s medical condition worsened during the delay. One modeling study of 6281 new stage 1 to 3 cancer cases in the United Kingdom who were delayed multidisciplinary workup during the pandemic suggested that an additional 181 lives and 3316 life years would be lost with a conservative estimate of only 25% of cases backlogged for 2 months.
During the early phases of the pandemic, the number of new cancers diagnosed decreased. , This drop was likely secondary to patients not presenting for care and not a true drop in incidence. Thus, these cancers will come to the radar eventually at a greater size or stage than they would have with earlier detection, which may affect prognosis. A model that assumed only a 6-month disruption of care during the pandemic estimated the potential excess deaths from breast and colorectal cancer secondary to the pandemic disruptions in care demonstrates an excess of more than 10,000 deaths in the next decade, peaking in the first few years. This model does not account for the increased morbidity, with possible more extensive surgeries including more mastectomies or more need for chemotherapy secondary to later presentations of disease.
Previous studies have demonstrated worsened outcomes during economic downturns, and in times of stress, and so it is likely the effects on breast cancer detection and management combined with the economic and societal effects of the pandemic will lead to effects on long-term outcomes. It is also plausible that if there are not measurable deleterious effects from these delays, then reimbursements for care may be renegotiated or guidelines may shift to reduce care.
Effects on hospitals and radiologists of changes in care
The COVID-19 pandemic has had marked economic effects on the health care system, academic radiology departments, and radiology practices. A survey conducted by ACR and the Radiology Business Management Association reported that 97.4% of 228 radiology practices (urban, academic, and rural) experienced declines in imaging volume in March/April 2020, with a drop of greater than 90% of elective procedures and 60% of urgent procedures. One-third of academic radiology chairs reported a near two-thirds decrease in volume with some reporting an 80% drop in hard hit areas. Greater than 82% of chairs had at least a 50% decrease in total radiology volume at the nadir.
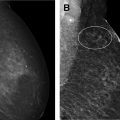
Breast imaging was disproportionately affected by postponed cases. The largest health care system in New York reported a drop of 88% affecting all modality types, with mammography use plummeting by 94%, MR imaging 74%, and ultrasound 64%. In another study of 6 academic medical centers across the United States, 3 centers in regions with lower rates of COVID-19, radiology volumes declined steeply from calendar week 11 to 16 with a range of 40% to 70% total volume drop at the lowest drop. Of those drops, screening mammography was among the most significant drop, as well as slowest in recovering. The reduction in screening mammography went as far as 99% in weeks 15 and 16. Diagnostic mammography volumes did not drop as dramatically, however still hit a low of 85% volume decrease at the nadir in week 16.
On gradual reopenings of care (in May–July in most centers), a significant backlog of past studies had built. In addition, significant changes in scheduling with increased evening or weekend hours, changes in protocols for shorter MR imaging scan times, and off-loading studies from hospitals and cancer centers to protect higher risk patients were required to allow for more spacing. Changes to patient registration and check-in, prescreening for symptoms, PPE requirements, and disinfection protocols were instituted briskly. One hundred percent of academic radiology departments reported reorganizing the waiting rooms and dressing areas to comply with social distancing mandates.
Radiology practices restructured reading rooms and implemented home PACS. Some practices shifted rapidly to home PACS, moving from100% of radiologists onsite to 80% reading from home within a few weeks. However, for breast imaging, this process is more complicated and expensive due to quality compliance requirements, the need for high-resolution monitors, and the need to be on site for diagnostic and interventions and happened at much lower levels. Telehealth increased in general, for patient surgery, oncology, and genetics appointments, as well as for virtual multidisciplinary tumor boards, leading to fewer in person multidisciplinary consults. Educational conferences and lectures moved to virtual platforms such as Webex, Microsoft Teams, and Zoom. , The effect of increased telecommuting and telehealth remain unclear. Telecommuting may increase radiologist morale, flexibility, and even potentially productivity, or alternatively it may decrease collaborations, interfacing with multidisciplinary colleagues, educational value, or productivity. About half of the radiologists surveyed nationwide believed that teleradiology would continue and lead to increased efficiency.
The marked reductions in volume have devastating financial implications to practices. Half of the health care practices in California furloughed or laid off employees and almost two-thirds reduced staff hours. , In academic practices, a quarter had furloughed or laid off staff. Significant reductions in radiologist and staff incomes (in about 50% of practices in one survey), personal and academic protected time, research endeavors, workload, hours, professional funds, bonuses and financial incentives, and retirement allocations occurred amid hiring freezes and workspaces changes. In a survey of 228 practices from across the country, there were mean reductions in both receipts and gross charges on average about 50%, and greater than 70% of respondents reported applying for some sort of governmental financial relief. Although emergency governmental funds for financial relief were dispensed to hospitals and health care organizations through The Coronavirus Aid, Relief, and Economic Security Act and the Paycheck Protection Program and Health Care Enhancement Act (on the order of nearly $200 billion dollars), these funds are likely not enough to prevent lasting financial implications from the significant disruptions in volume and care. , Although practices are recovering, some near fully, as of September 2020, the anticipated time to full recovery remains unknown.
Effects on radiologist’s mental health through this crisis have been significant. More than 60% of 600 radiologists in 44 states rated their anxiety as a 7 out of 10 during the pandemic. In addition to having work and economic worries, some radiologists and staff were redeployed in the early days in hotspots to better serve COVID-19 patient care. In addition, many radiologists have had increased burdens at home with unexpected need to provide childcare and teaching duties for virtual schooling amid school and childcare care closures. In addition, more than one-third of radiologists thought that they did not have adequate teleradiology capabilities during the pandemic, and about half said they did not have adequate PPE for themselves or their patients. Mental stress regarding personal and family health, disruptions to travel and schedule, and family members with lost jobs or decreased income also affects the potential for long-term burnout in radiologists to increase, and mitigation strategies for burnout should be used.
Delays in clinical research education and academic meetings
Radiology education has also been significantly disrupted during the COVID-19 pandemic, including the need for redeployment, changes to reading rooms and social distancing, and cessation of in person conferences and didactic learning. Some radiologists, especially residents early in training, were redeployed to other areas, particularly hard-hit urban environments such as New York and Boston, with some medical students even graduating early to join the front lines in caring for COVID-19–infected patients. Approximately 40% of radiologists in one survey thought that the shift to socially distant interpretations and conferences had a deleterious effect on resident and fellow education.
Hundreds of scientific and medical conferences including dozens of radiology conferences were canceled or moved to virtual formats. Significant impacts on networking, collaboration, committee work, vendor marketing, scientific presentations, and sharing of research are likely that may affect scientific progress as well as career choices. Many radiologists were placed on institutional or state travel bans. Virtual grand rounds and virtual interviews both for education and for hiring were implemented during the pandemic. The cost and time savings of such virtual practices may prove to be practice changing after the pandemic is over.
Initially, most academic centers and universities suspended research, especially all trials involving patients or in-person interactions. Guidance on how best to preserve clinical trials, and maintain integrity for those interrupted, was offered by the senior editorial staff at JAMA. The FDA offered direction for those trials that may be disrupted. Additional suggestions on how to avoid overestimation of disease-free survival if patients skip assessments and to report results from data during the pandemic separately from date before the pandemic continue to be offered. , In contrast, the National Cancer Institute intentionally kept functioning at 100% and stressed the importance of maintaining research to allow patients to have access to clinical trials and to maintain scientific progress, as well as to study the effects of COVID-19 in patients with cancer. The National Cancer Institute (NCI) showed increased flexibility for prior minor infractions (such tests as a missed blood draw), recognizing that they may be necessary during COVID-19 to help maintain social distancing best practices for the patient. Some of the flexibility extended to clinical trials during the pandemic such as virtual, instead of in-person, visits for enrollment or assessments, the ability to receive tests and laboratory draws at sites closer to the patient that are not part of the trial sites, and decreases in the administrative tasks required prepandemic may carry over to the postpandemic world, perhaps making clinical trials more accessible to the general population.
Of note, the pandemic led to the creation of unique opportunities for the creation of collaborative, crowdsourced research endeavors and databases, including the COVID-19 and Cancer Consortium, among others, collecting real-time data for observational trials.
Long-term ramifications and rebuilding
The final economic costs of the pandemic on the health care industry will likely be colossal. One study proposes the direct medical costs will approach $165 billion dollars if only 20% of the population is infected (53.8 million symptomatic cases) and would continue to cost up to a total of almost $215 billion in indirect costs in the year after discharge. This figure will increase if the percent infected increased greater than that. Nationally, there has been significant deleterious effects on the economy including almost 17 million Americans filing for unemployment in a 3-week period over March/April alone, although with claims decreasing continually since that peak. , Whether or not COVID-19 will continue to circulate in the population with annual or seasonal outbreaks or whether this will be an outbreak that has mostly cycled through the population with a return to closer to normal by 2022 or so remains unclear and debated yet at the time of this writing.
What is clear is that without a vaccine and other treatments, social distancing and PPE with masks and other protections for HCWs are likely to remain the primary weapons against the virus and will likely continue to play a part in daily life and in radiology practices and patient care in breast imaging centers for a while yet to come. What the future looks like on the other side of the pandemic remains unclear but will involve significant effects on both COVID-19– and non-COVID-19–related health outcomes, mental health outcomes, the national and global economy, radiology practices and breast centers, and on cancer outcomes, screening rates, and cancer management and treatment protocols.
Clinics care points
- •
If care is taken for protective measures for the patients and HCWs as outlined in different care algorithms, breast cancer treatment should continue during the pandemic, especially in light of the unknown timeframe of the crisis.
- •
It is unclear what effects these COVID-19 provoked changes in cancer screening and management will have on long term cancer outcomes.
- •
Radiology volumes dropped drastically during the early weeks of the pandemic, with the most dramatic reductions in screening mammography which came to a near complete halt for a few weeks in most places.
- •
Mental stress and workload changes increase the potential for long term burnout in radiologists to increase and mitigation strategies for burnout should be employed.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree