 he anatomy of the knee is complex. Osseous, cartilaginous, and passive and dynamic restraints must be preserved to ensure optimal function. To this end, numerous orthopaedic devices and prostheses have been designed to maintain a knee that is functional and pain-free. This chapter will review orthopaedic devices and imaging techniques for trauma, joint replacement, and other common surgical procedures about the knee.
he anatomy of the knee is complex. Osseous, cartilaginous, and passive and dynamic restraints must be preserved to ensure optimal function. To this end, numerous orthopaedic devices and prostheses have been designed to maintain a knee that is functional and pain-free. This chapter will review orthopaedic devices and imaging techniques for trauma, joint replacement, and other common surgical procedures about the knee.
 Trauma
Trauma
Preoperative Imaging
Imaging of the knee in patients with suspected trauma is different from certain other indications. Patients may not be able to tolerate special views. Therefore, anteroposterior (AP), lateral, and both oblique views (see Fig. 6-1) are routinely obtained. The lateral view (Fig. 6-1E and F) should be obtained using cross-table lateral technique because a lipohemarthrosis may be the only indication of a subtle intra-articular fracture. Standing views are not usually required. Additional views, such as the notch or patellar views, should be considered if the patient can tolerate the necessary positioning. These views are useful for detection of patellar fracture or alignment abnormalities and osteochondral injuries.
When indicated, computed tomography (CT) is useful to further evaluate suspected fractures or fragment position (see Fig. 6-2). Magnetic resonance imaging (MRI) is also able to detect subtle osseous injuries as well as evaluate the articular cartilage (see Fig. 6-3) and soft tissue supporting structures.
SUGGESTED READING
Berquist TH. Osseous and myotendinous injuries about the knee. Magn Reson Imaging Clin N Am. 2007;15:25–38.
Mui LW, Engelsohn E, Umans H. Comparison of CT and MRI in patients with tibial plateau fractures: Can CT findings predict ligament tear or meniscal injury? Skeletal Radiol. 2007; 36:145–151.
Supracondylar Fractures of the Femur
Supracondylar fractures of the femur are fractures involving the distal 9 to 15 cm, as measured from the articular surface of the femoral condyles. These fractures are relatively uncommon, accounting for only 7% of femoral fractures. Fractures may be impacted, undisplaced, comminuted, and involve the articular surface of the femur. Associated injuries of the tibial plateau, proximal tibia, proximal femur, and soft tissues of the knee are common. Approximately 5% to 10% of supracondylar fractures are open injuries, usually anterior and proximal to the patella.
The mechanism of injury is usually varus or valgus stress with associated axial or rotary forces. Injuries are usually related to high-velocity trauma such as motor vehicle accidents in younger patients or due to more minor trauma in the elderly. There are multiple classification systems based on extra-articular, one or more condyle involvement, the plane of the fracture, and the degree of comminution.
Classification: Orthopaedic Trauma Association (see Fig. 6-4)
Type A: Extra-articular, simple, or comminuted
A1—simple (Fig. 6-4A)
A2—metaphyseal, wedge (Fig. 6-4B) A3—metaphyseal, complex
Type B: Partial articular, one condyle involved (Fig. 6-4C)
B1—lateral condyle, sagittal fracture line
B2—medial condyle, sagittal fracture line
B3—frontal coronal fracture line
Type C: Complete articular, both condyles involved with
“T” or “Y” pattern, or comminuted
C1—both condyles, simple (Fig. 6-4D)
C2—both condyles, multiple metaphyseal fragments (Fig. 6-4E)
C3—both condyles, all segments comminuted
SUGGESTED READING
Schatzker J. Fractures of the distal femur revisited. Clin Orthop. 1998;347:43–56.
Orthopaedic Trauma Association Committee on Coding and Classifications. Fractures and dislocations compendium. J Orthop Trauma. 1996;10(Suppl 1):41–45.
Treatment Options
The goals for treatment are to restore alignment and articular anatomy. Both closed and open techniques may be employed depending on the patient status (i.e., other injuries) and the type of fracture. Reduction may be difficult to maintain due to muscle forces acting on the fragments.
Traction: Traction is a useful temporary approach to comminuted fractures or when patient status will not allow primary definitive fixation. Single or double traction pins may be used. A single pin can be placed in the proximal tibia with the option of a second pin in the distal femoral fragment (see Fig. 6-5). The latter can add problems such as quadriceps scarring.
External Fixation: As noted in previous chapters, external fixation is particularly useful in multitrauma patients, with complex fractures and when there are open wounds that require easy wound access. Fractures that are considered for external fixation fall into the above-mentioned categories and are typically complex nonarticular (OTA A3), and complex bicondylar (OTA C3). Unilateral, ring, or hybrid fixators can be used (see Fig. 6-6). Mean healing time is 4 months. Secondary procedures are required in approximately 20% of cases (Fig. 6-6B and C).
Internal Fixation: Internal fixation can be accomplished using multiple approaches. The type of fracture pattern, other injuries, and surgical preference dictate the approach selected. Extra-articular fractures (OTA type A) and fractures with condylar fragmentation (OTA type C3) can be treated with blade plates or dynamic condylar screws (see Figs. 6-7 and 6-8). Antigrade or retrograde intramedullary locking nails may also be used. In recent years, use of less invasive stabilization system (LISS) plates has become more popular. These plates have screws with threaded heads to lock them to the plate at a fixed angle (see Chapter 2) analogous to external fixation. The construct does not need to contact the bone and can be placed with less invasion of the soft tissue envelope preserving the blood supply (see Fig. 6-9). This system is particularly useful in patients with periprosthetic fractures. In some situations, custom knee prostheses are employed for complex distal femoral fractures.


 Fig 6.1 Routine views of the knee. Anteroposterior (AP) (A) and lateral (B) radiographs of the knee demonstrating a bipartite patella (arrow). Oblique views are obtained in internal (C) and external rotation (D). These views may detect subtle injuries not identified on AP and lateral views. Note the femoral condyle fracture (arrows) on the external oblique radiograph. The normal lateral view may demonstrate an effusion (E) (arrow), but a cross table lateral view (F) is more useful and can demonstrate a lipohemarthrosis (arrows).
Fig 6.1 Routine views of the knee. Anteroposterior (AP) (A) and lateral (B) radiographs of the knee demonstrating a bipartite patella (arrow). Oblique views are obtained in internal (C) and external rotation (D). These views may detect subtle injuries not identified on AP and lateral views. Note the femoral condyle fracture (arrows) on the external oblique radiograph. The normal lateral view may demonstrate an effusion (E) (arrow), but a cross table lateral view (F) is more useful and can demonstrate a lipohemarthrosis (arrows).
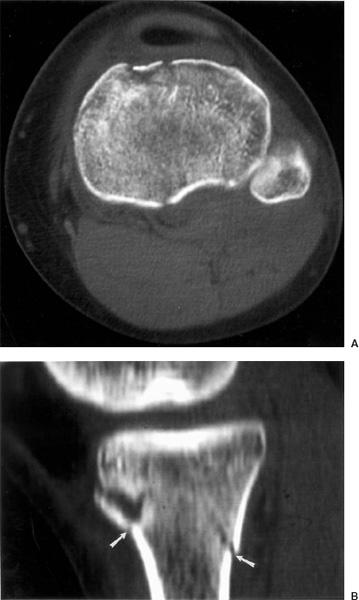
 Fig 6.2 Axial (A) and sagittal reformatted (B) computed tomographic (CT) images demonstrating a tibial plateau fracture with metaphyseal involvement (arrows).
Fig 6.2 Axial (A) and sagittal reformatted (B) computed tomographic (CT) images demonstrating a tibial plateau fracture with metaphyseal involvement (arrows).
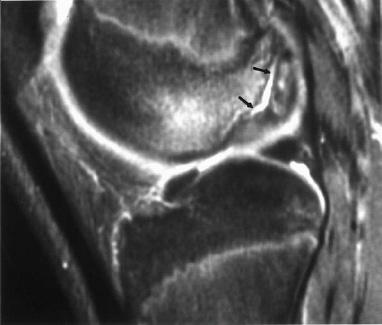
 Fig 6.3 Sagittal T2-weighted magnetic resonance (MR) image demonstrating a separated osteochondral fragment posteriorly (arrows).
Fig 6.3 Sagittal T2-weighted magnetic resonance (MR) image demonstrating a separated osteochondral fragment posteriorly (arrows).
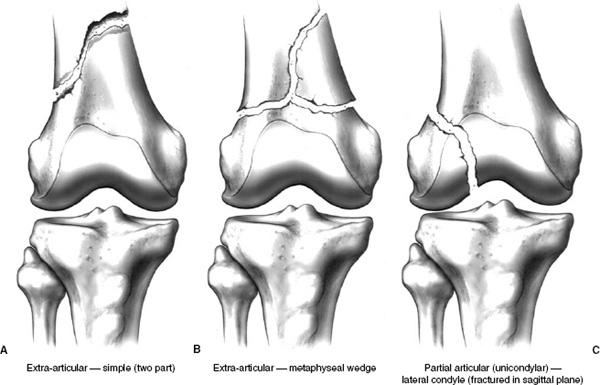
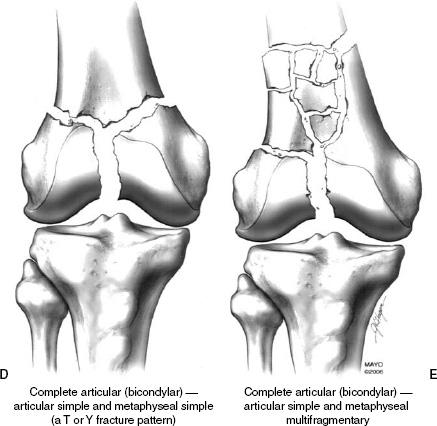
 Fig 6.4 Orthopaedic Trauma Association classification for supracondylar fractures. A: Simple extra-articular type A1. B: More complex extra-articular, in this case a metaphyseal wedge or type A2. C: Partial articular or unicondylar, in this case involving the lateral condyle or type B1. D: Complete or bicondylar type C1. E: Complete bicondylar with metaphyseal comminution or type C2.
Fig 6.4 Orthopaedic Trauma Association classification for supracondylar fractures. A: Simple extra-articular type A1. B: More complex extra-articular, in this case a metaphyseal wedge or type A2. C: Partial articular or unicondylar, in this case involving the lateral condyle or type B1. D: Complete or bicondylar type C1. E: Complete bicondylar with metaphyseal comminution or type C2.
SUGGESTED READING
Arazi M, Memik R, Ogun TC, et al. Ilizarov external fixation for severely comminuted supracondylar and intercondylar fractures of the distal femur. J Bone Joint Surg. 2001;83B:663– 667.
Davila J, Malkani A, Paiso JM. Supracondylar distal femoral fracture nonunions treated with megaprosthesis in the elderly: A report of two cases. J Orthop Trauma. 2001;15:574– 578.
Helfet DL, Lorich DG. Retrograde intramedullary nailing of supracondylar fractures. Clin Orthop. 1998;350: 80–84.
Schultz M, Muller M, Krettek C, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: A prospective multicenter study. Injury. 2001; 32(Suppl 3):48–54.
Patellar Fractures
Patellar fractures account for approximately 1% of all skeletal fractures in both adults and children. They most commonly occur between 20 and 50 years of age and males outnumber females 2:1. The superficial position places the patella at risk for direct trauma. Direct trauma compresses the patella against the femoral condyle resulting in more cartilage damage and comminution although there is less displacement of fragments compared to indirect trauma. Indirect trauma, such as rapid flexion against a contracted quadriceps mechanism, results in less comminution, but greater displacement. In fact most indirect patellar fractures are transverse.
Patellar fractures are classified on the basis of radiographic configuration (see Fig. 6-10). Most fractures are transverse (50% to 80%), comminuted fractures account for 30% to 35%, and vertical 12% to 17% of patellar fractures. Osteochondral fractures may occur with patellar dislocations (see Fig. 6-11). There is often an associated bone bruise of the femoral condyle. Less frequently patellar fractures may follow total knee replacement (0.68%) (see Fig. 6-12) or anterior cruciate ligament (ACL) repairs. The latter are due to stress risers in the patella when patellar tendon graft with bone from the patella and tibial tuberosity (see Fig. 6-13) is used for the ligament graft. Open fractures occur with 7% of patellar fractures and have a more guarded prognosis.


 Fig 6.5 Severely comminuted distal femoral fracture (OTA type A3, extra-articular complex). Anteroposterior (AP) (A) and lateral (B) radiographs obtained during pin placement show the complex fracture with posterior displacement of the distal fragment due to gastrocnemius muscle forces (arrow in B). The traction pin fractured the opposite cortex (white arrow) requiring replacement with double pins above and below the fracture site demonstrated on AP (C) and lateral (D) radiographs. AP (E) and lateral (F) radiographs in traction. This was later converted to a hinged cast brace (G). At 1-year follow-up the fracture has healed (H) with shortening and angular deformity. OTA, Orthopaedic Trauma Association.
Fig 6.5 Severely comminuted distal femoral fracture (OTA type A3, extra-articular complex). Anteroposterior (AP) (A) and lateral (B) radiographs obtained during pin placement show the complex fracture with posterior displacement of the distal fragment due to gastrocnemius muscle forces (arrow in B). The traction pin fractured the opposite cortex (white arrow) requiring replacement with double pins above and below the fracture site demonstrated on AP (C) and lateral (D) radiographs. AP (E) and lateral (F) radiographs in traction. This was later converted to a hinged cast brace (G). At 1-year follow-up the fracture has healed (H) with shortening and angular deformity. OTA, Orthopaedic Trauma Association.
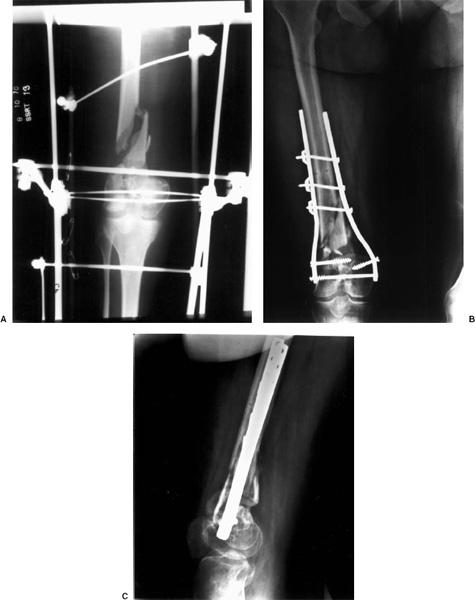
 Fig 6.6 A: Anteroposterior (AP) radiograph of a complex (OTA C3) fracture treated with hybrid external fixation. This was eventually treated with open reduction and internal fixation using bilateral plates and screws with locking bolts (B and C). OTA, Orthopaedic Trauma Association.
Fig 6.6 A: Anteroposterior (AP) radiograph of a complex (OTA C3) fracture treated with hybrid external fixation. This was eventually treated with open reduction and internal fixation using bilateral plates and screws with locking bolts (B and C). OTA, Orthopaedic Trauma Association.

 Fig 6.7 Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating a complex distal femoral fracture treated with open reduction and internal fixation using a dynamic compression plate and blade plate (arrow). The compression plate has been revised with proximal screw remnants and fractures.
Fig 6.7 Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating a complex distal femoral fracture treated with open reduction and internal fixation using a dynamic compression plate and blade plate (arrow). The compression plate has been revised with proximal screw remnants and fractures.

 Fig 6.8 Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating internal fixation with a dynamic condylar screw (white arrow). There is also bone graft (open arrow) and a lag screw (black arrowhead).
Fig 6.8 Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating internal fixation with a dynamic condylar screw (white arrow). There is also bone graft (open arrow) and a lag screw (black arrowhead).

 Fig 6.9 Anteroposterior (AP) (A) and lateral (B) radiographs in an elderly patient with a complex distal femoral fracture with metaphyseal comminution and intra-articular involvement (OTA type C2) treated with an less invasive stabilization system (LISS) plate and screws.
Fig 6.9 Anteroposterior (AP) (A) and lateral (B) radiographs in an elderly patient with a complex distal femoral fracture with metaphyseal comminution and intra-articular involvement (OTA type C2) treated with an less invasive stabilization system (LISS) plate and screws.
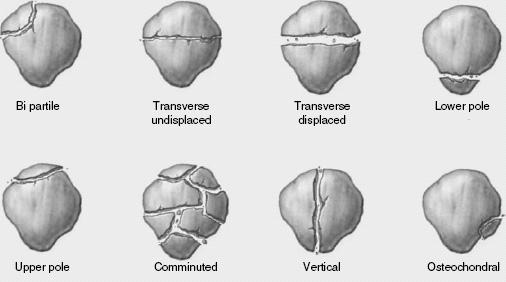
 Fig 6.10 Illustration of the different types of patella fracture including the bipartite patella, which is a normal variant.
Fig 6.10 Illustration of the different types of patella fracture including the bipartite patella, which is a normal variant.
Imaging can be accomplished with AP, lateral, and patellar (Merchant) views. Bipartite patellae are frequently bilateral and should not be confused with a fracture (Figs. 6-10 and 6-1). MRI is useful to fully evaluate osteochondral lesions (Fig. 6-11) and associated soft tissue injuries.
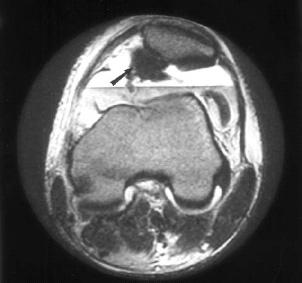
 Fig 6.11 Osteochondral fracture following patellar dislocation and relocation. Axial T2-weighted magnetic resonance (MR) image demonstrates a lipohemarthrosis and large osteochondral fracture (arrow) of the patella.
Fig 6.11 Osteochondral fracture following patellar dislocation and relocation. Axial T2-weighted magnetic resonance (MR) image demonstrates a lipohemarthrosis and large osteochondral fracture (arrow) of the patella.
SUGGESTED READING
Carpenter JE, Arbor A, Kasman R. Fractures of the patella. J Bone Joint Surg. 1993;75A:1550–1560.
Ortigera CJ, Berry DJ. Patellar fracture after total knee arthroplasty. J Bone Joint Surg. 2002;84A:532–540.
Sonin AH, Fitzgerald SW, Bresler ME, et al. MR imaging appearance of the extensor mechanism of the knee: functional anatomy and injury patterns. Radiographics. 1995;15:367– 382.
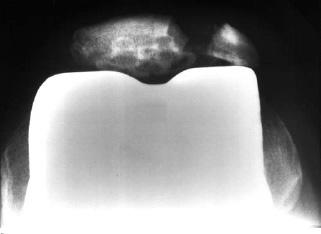
 Fig 6.12 Patellar fracture following total knee replacement. Merchant view demonstrating a displaced lateral patellar fracture.
Fig 6.12 Patellar fracture following total knee replacement. Merchant view demonstrating a displaced lateral patellar fracture.

 Fig 6.13 Anteroposterior (AP) (A) and lateral (B) radiographs following anterior cruciate ligament (ACL) repair with donor sites in the tibial plateau (arrow in B) and patella (arrow in A). This places the patella at increased risk for fracture.
Fig 6.13 Anteroposterior (AP) (A) and lateral (B) radiographs following anterior cruciate ligament (ACL) repair with donor sites in the tibial plateau (arrow in B) and patella (arrow in A). This places the patella at increased risk for fracture.
Treatment Options
Treatment Options Treatment of patellar fractures should achieve the goals of anatomic reduction with realignment of the articular surface and restoration of soft tissue, specifically the retinacula and extensor mechanism. Undisplaced fractures (≤2 mm) with minimal articular irregularity (≤2 mm) may be treated in a cylinder cast (see Chapter 2) for 4 to 6 weeks. Displaced fractures (≥2 mm articular deformity and ≥3 mm of separation) (see Fig. 6-14) should be treated with open reduction and internal fixation. Typically, tension band and K-wires (see Fig. 6-15) or cannulated screws with wires or cables (see Fig. 6-16) are used. For comminuted fractures portions or the entire patella may have to be removed.

 Fig 6.14 Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating a comminuted displaced patellar fracture.
Fig 6.14 Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating a comminuted displaced patellar fracture.
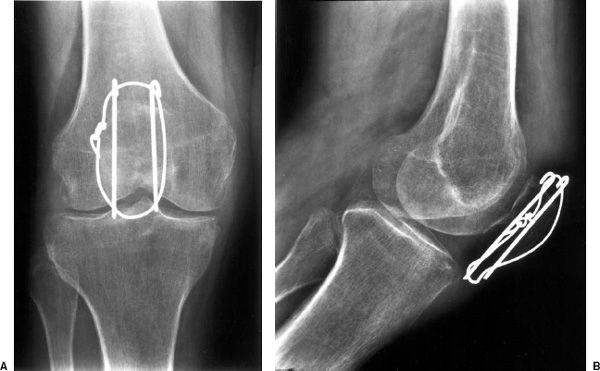
 Fig 6.15 Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating reduction of the patellar fracture with two K-wires and tension band technique. There is minimal articular deformity.
Fig 6.15 Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating reduction of the patellar fracture with two K-wires and tension band technique. There is minimal articular deformity.

 Fig 6.16 Anteroposterior (AP) (A), lateral (B), and Merchant (C) radiographs demonstrate fixation of a comminuted patellar fracture with two cannulated screws and a threaded Dall-Miles cable. There are also two cannulated interfragmentary screws (arrows). There is slight residual articular separation (open arrow in B).
Fig 6.16 Anteroposterior (AP) (A), lateral (B), and Merchant (C) radiographs demonstrate fixation of a comminuted patellar fracture with two cannulated screws and a threaded Dall-Miles cable. There are also two cannulated interfragmentary screws (arrows). There is slight residual articular separation (open arrow in B).
SUGGESTED READING
Carpenter JE, Arbor A, Kasman R. Fractures of the patella. J Bone Joint Surg. 1993;75:1550–1560.
Ray JM, Hendrix J. Incidence, mechanism of injury, and treatment of fractures of the patella in children. J Trauma. 1992;32:464–467.
Proximal Tibial Fractures
Fractures of the proximal tibia in adults may involve the articular surface (osteochondral, tibial eminence, plateau) metaphysis or tuberosity without articular involvement. In children and adolescents, fractures more frequently involve the tuberosity, tibial eminence, or physis. The latter are uncommon and account for <5% of physeal fractures.
Tibial Condyle/Plateau Fractures
Tibial Condyle/Plateau Fractures Tibial condyle fractures result from significant falls or high-velocity trauma. Vertical compression forces may lead to T- or Y-fracture configurations. Varus or valgus forces involve the medial or lateral plateaus, respectively. Internal derangement is common. Rotational forces are also often part of the injury pattern causing a variety of fracture patterns.
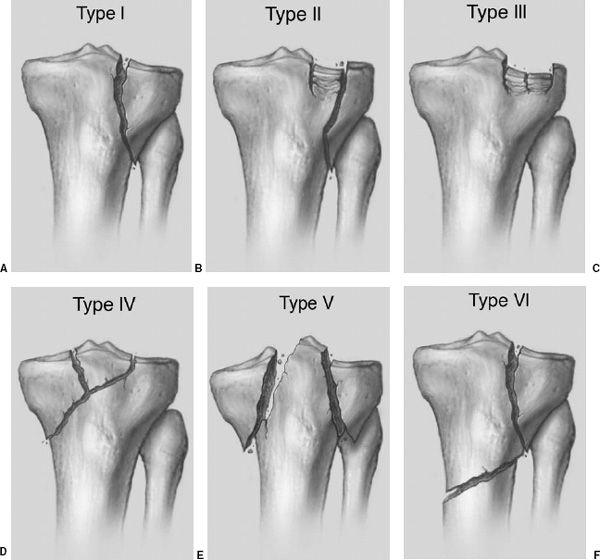
 Fig 6.17 Schatzker classification. A: Type I—pure lateral plateau split. B: Type II—lateral split with depressed plateau. C: Type III—central depression alone. D: Type IV—medial plateau with lateral extension. E: Type V—both plateaus with displacement. F: Type VI—lateral split with metaphyseal fracture.
Fig 6.17 Schatzker classification. A: Type I—pure lateral plateau split. B: Type II—lateral split with depressed plateau. C: Type III—central depression alone. D: Type IV—medial plateau with lateral extension. E: Type V—both plateaus with displacement. F: Type VI—lateral split with metaphyseal fracture.
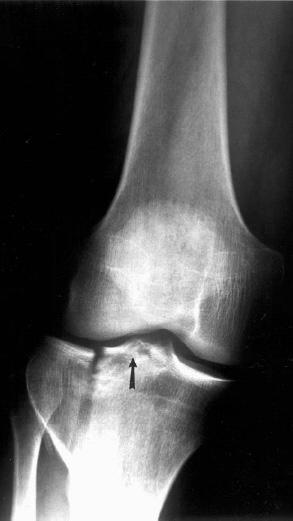
 Fig 6.18 Schatzker type II or OTA type B1.3. Anteroposterior (AP) radiograph demonstrating a lateral plateau split with slight separation and depression and involvement (arrow) of the tibial eminence.
Fig 6.18 Schatzker type II or OTA type B1.3. Anteroposterior (AP) radiograph demonstrating a lateral plateau split with slight separation and depression and involvement (arrow) of the tibial eminence.
Classifications: Multiple fracture classifications have been used for these injuries beginning with the Hohl Classification in the 1960s and followed by the Schatzker, Moore, Honkonen, and Orthopaedic Trauma Association (OTA) in 1996. Classifications are based on radiographic features. The most commonly used patterns are the Schatzker and OTA classifications. These are summarized in the subsequent text.
Schatzker classification: (see Fig. 6-17)
Type I: Lateral plateau split (common in young adults)
Type II: Lateral plateau split with depressed fragment, medial collateral ligament (MCL) injury (see Fig. 6-18)
Type III: Lateral depression only (common in older patients), no instability, may treat conservatively (see Fig. 6-19)
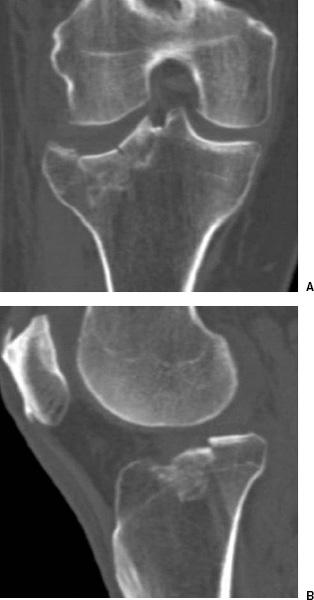
 Fig 6.19 Simple partial depression of the lateral plateau in an elderly female demonstrated on coronal (A) and sagittal (B) reformatted computed tomographic (CT) images.
Fig 6.19 Simple partial depression of the lateral plateau in an elderly female demonstrated on coronal (A) and sagittal (B) reformatted computed tomographic (CT) images.
Type IV: Medial split often involving tibia eminence, associated neurovascular injury
Type V: Bicondylar with severe soft tissue injury
Type VI: Metaphyseal/diaphyseal dissociation, associated compartment syndrome
OTA classification: (see Fig. 6-20)
Type A1: Extra-articular avulsion (Fig. 6-20A)
A1.1—fibular head avulsion
A1.2—tibial tuberosity avulsion
A1.3—cruciate insertion avulsion
Type A2: Extra-articular, simple metaphyseal fracture (Fig. 6-20B)
A2.1—oblique fracture in frontal plane
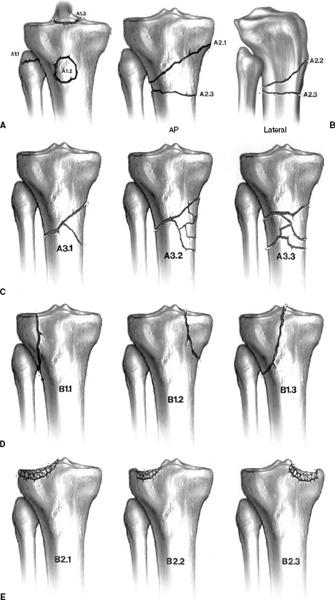
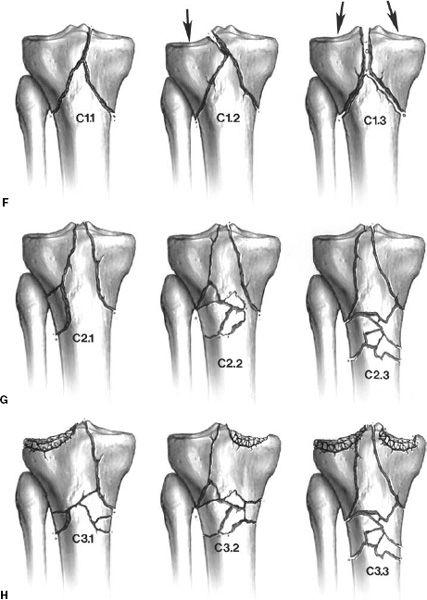
 Fig 6.20 Orthopaedic Trauma Association classification. A: Type A1—avulsion injuries. A1.1—fibular head avulsion, A1.2—tibial tuberosity avulsion, A1.3—cruciate avulsion. B: Type A2—metaphyseal extra-articular. A2.1—oblique frontal plane, A2.2—oblique sagittal plane, A2.3—transverse. C: Type A3—extra-articular comminuted. A3.1—intact wedge, A3.2—fragmented wedge, A3.3—complex. D: Type B1—partial articular, pure split. B1.1—lateral split, B1.2—medial split, B1.3—split involving tibial spines. E: Type B2—pure depression. B2.1—total lateral depression, B2.2—limited depression, B2.3—medial depression. F: Type C1—complete articular. C1.1—slight displacement, C1.2—one condyle displaced (arrow), C1.3—both condyles displaced (arrows). G: Type C2—simple articular, metaphysis complex. C2.1—intact wedge, C2.2—comminuted wedge, C2.3—metaphysis complex. H: Type C3—complex articular and metaphysis. C3.1—lateral complex, C3.2—medial complex, C3.3—both medial and lateral complex.
Fig 6.20 Orthopaedic Trauma Association classification. A: Type A1—avulsion injuries. A1.1—fibular head avulsion, A1.2—tibial tuberosity avulsion, A1.3—cruciate avulsion. B: Type A2—metaphyseal extra-articular. A2.1—oblique frontal plane, A2.2—oblique sagittal plane, A2.3—transverse. C: Type A3—extra-articular comminuted. A3.1—intact wedge, A3.2—fragmented wedge, A3.3—complex. D: Type B1—partial articular, pure split. B1.1—lateral split, B1.2—medial split, B1.3—split involving tibial spines. E: Type B2—pure depression. B2.1—total lateral depression, B2.2—limited depression, B2.3—medial depression. F: Type C1—complete articular. C1.1—slight displacement, C1.2—one condyle displaced (arrow), C1.3—both condyles displaced (arrows). G: Type C2—simple articular, metaphysis complex. C2.1—intact wedge, C2.2—comminuted wedge, C2.3—metaphysis complex. H: Type C3—complex articular and metaphysis. C3.1—lateral complex, C3.2—medial complex, C3.3—both medial and lateral complex.
A2.2—oblique fracture in sagittal plane
A2.3—transverse fracture
Type A3: Extra-articular comminuted (Fig. 6-20C)
A3.1—intact wedge fracture
A3.2—fragmented wedge fracture
A3.3—complex fracture
Type B1: Partial articular, split fracture (Fig. 6-20D)
B1.1—lateral split
B1.2—medial split
B1.3—medial or lateral involving tibia eminence (Fig. 6-18)
Type B2: Partial articular, pure depression (Fig. 6-20E)
B2.1—lateral total articular surface
B2.2—lateral but limited (Fig. 6-19)
B2.3—medial depression
Type C1: Complete articular with simple metaphyseal fracture (Fig. 6-20F)
C1.1—slight displacement
C1.2—one condyle displaced
C1.3—both condyles displaced
Type C2: Complete simple articular with comminuted metaphysic (Fig. 6-20G)
C2.1—intact wedge
C2.2—comminuted wedge
C2.3—complex metaphysic
Type C3: Complex articular, complex metaphysic (Fig. 6-20H)
C3.1—complex lateral plateau
C3.3—complex both plateaus
The significant factors regarding these classifications is the degree of depression or displacement of the articular surface and secondary injuries associated with the categories of injury. A split fracture of the medial plateau (Schatzker IV or OTA B1.2) is associated with vascular injury and peroneal nerve palsy. Schatzker types V and VI or OTA type C fractures involve both condyles, and with tibial fragmentation there is an increased risk for compartment syndrome and soft tissue injury. Obviously, more complex fractures are much more difficult to manage surgically. These concepts will be discussed more fully under treatment options.
SUGGESTED READING
Barei DP, Nork SE, Mills WJ, et al. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg. 2006; 88A:1713–1721.
Martin J, Marsh JL, Nepola JV, et al. Radiographic fracture assessments: Which ones can we reliably make. J Orthop Trauma. 2000;14:379–385.
Orthopaedic Trauma Association Committee on Coding and Classifications. Fractures and dislocations compendium. J Orthop Trauma. 1996;10(Suppl 1):41–45.
Schatzker J, McBroom R, Bruce D. The tibial plateau fracture: The Toronto experience 1968–1975. Clin Orthop. 1979;138: 94–104.
Preoperative Imaging
AP, lateral, and oblique images will usually define the complex fracture of the tibial condyles. A cross-table lateral image may demonstrate a lipohemarthrosis, which may be the only finding in subtle intra-articular fractures. In most cases, CT with reformatting in the coronal and sagittal planes and 3-D reconstructions provide the necessary data for treatment planning (see Fig. 6-21). MRI is useful to evaluate soft tissue injury. In fact, some would argue that MRI can accurately evaluate the extent of both osseous and soft tissue injuries (see Fig. 6-22). It is generally stated that depression of 5 to 8 mm and separation of ≥4 mm indicates the need for open reduction and internal fixation.
SUGGESTED READING
Kode L, Lieberman JM, Motta AO, et al. Evaluation of plateau fractures: Efficacy of MR imaging compared with CT. AJR Am J Roentgenol. 1994;163:141–147.
Treatment Options
Treatment Options Treatment of tibial condyle or plateau fractures depends on the extent of bone and soft tissue injury, patient age, activity status, and whether there are associated injuries. Minimally displaced fractures can be treated conservatively with cast immobilization or bracing. No weight bearing is permitted for 12 to 16 weeks. Schatzker type III or OTA B2 (simple central depression) fractures generally do not require internal fixation.

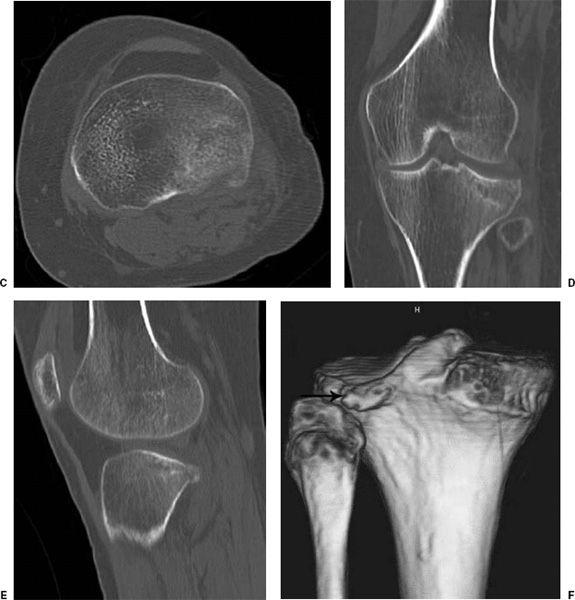
 Fig 6.21 Subtle depression of the lateral tibial plateau. Anteroposterior (AP) (A) and lateral (B) radiographs demonstrate a subtle lateral plateau fracture on the left in A (arrow) and a joint effusion on the lateral radiograph (arrow in B). Axial (C), coronal (D), and sagittal (E) reformatted computed tomographic (CT) images demonstrate a slightly displaced posterior plateau fracture clearly depicted on the 3-D image (F) (arrow).
Fig 6.21 Subtle depression of the lateral tibial plateau. Anteroposterior (AP) (A) and lateral (B) radiographs demonstrate a subtle lateral plateau fracture on the left in A (arrow) and a joint effusion on the lateral radiograph (arrow in B). Axial (C), coronal (D), and sagittal (E) reformatted computed tomographic (CT) images demonstrate a slightly displaced posterior plateau fracture clearly depicted on the 3-D image (F) (arrow).

 Fig 6.22 Coronal T1-weighted (A) and dual echo steady state (DESS) (B) images demonstrating a subtle undisplaced plateau fracture (arrow).
Fig 6.22 Coronal T1-weighted (A) and dual echo steady state (DESS) (B) images demonstrating a subtle undisplaced plateau fracture (arrow).
External Fixation: Most unstable fractures are treated with internal fixation. However, bicondylar fractures (Schatzker types V and VI and OTA type C1 to 3) have been treated with external fixation using ring fixators. Soft tissue infection and wound necrosis are not unusual following internal fixation techniques. Comparison of external fixation and medial and lateral plate fixation had equal anatomic results. External fixation afforded a shorter hospital stay, less blood loss, and earlier ambulation.
Internal Fixation: Open reduction and fixation allows the depressed fragments to be elevated and reduction to be maintained with differing approaches depending on the degree of injury. For split fractures, cancellous screws and washers may be sufficient (see Fig. 6-23). Buttress plates can also be used (see Fig. 6-24). Bicondylar fractures (Schatzker type V and VI and OTA type C) usually require bilateral plates (see Fig. 6-25) and frequently bone graft (see Fig. 6-26) to achieve optimal results. Regardless of the surgical approach, early motion is important to restore function.


 Fig 6.23 Coronal (A) and sagittal (B) computed tomographic (CT) images demonstrate a minimally depressed plateau fracture without significant separation of the fragments. The fragments were elevated and reduction achieved with cannulated screws and washers as seen on anteroposterior (AP) (C) and lateral (D) radiographs.
Fig 6.23 Coronal (A) and sagittal (B) computed tomographic (CT) images demonstrate a minimally depressed plateau fracture without significant separation of the fragments. The fragments were elevated and reduction achieved with cannulated screws and washers as seen on anteroposterior (AP) (C) and lateral (D) radiographs.
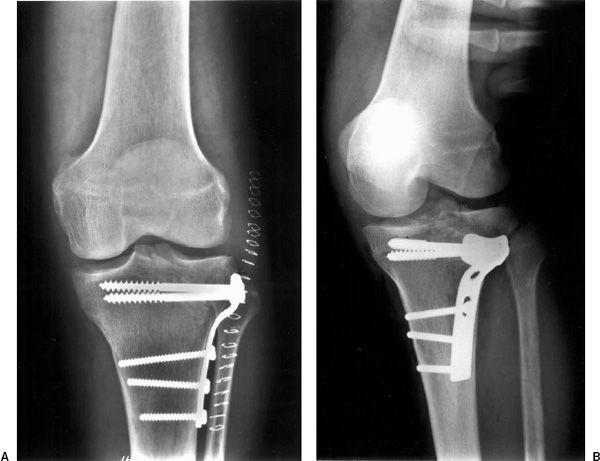
 Fig 6.24 Lateral plateau fracture that enters the eminence. Radiographs in the anteroposterior (AP) (A) and oblique (B) projections demonstrate reduction achieved with a T-buttress plate and screws.
Fig 6.24 Lateral plateau fracture that enters the eminence. Radiographs in the anteroposterior (AP) (A) and oblique (B) projections demonstrate reduction achieved with a T-buttress plate and screws.

 Fig 6.25 Anteroposterior (AP) radiograph following reduction of a complex plateau and metaphyseal fracture with bilateral plate and screws and cancellous screws and washers laterally.
Fig 6.25 Anteroposterior (AP) radiograph following reduction of a complex plateau and metaphyseal fracture with bilateral plate and screws and cancellous screws and washers laterally.
SUGGESTED READING
Barie DP, Nork SE, Mills WJ, et al. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg. 2006; 88A:1713–1721.
Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared to circular fixator application for bicondylar tibial plateau fractures. J Bone Joint Surg. 2006;88A: 2613–2623.
Lachiewicz PF, Funcik T. Factors influencing the results of open reduction and internal fixation of tibial plateau fractures. Clin Orthop. 1990;259:210–215.
Waddell JP, Johnston DW, Neidre A. Fractures of the tibial plateau: A review of ninety-five patients and comparison of treatment methods. J Trauma. 1981;21:376–381.
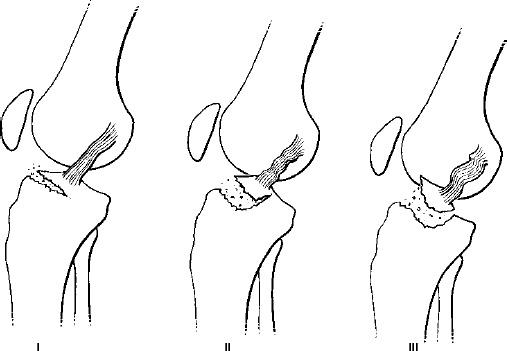
Miscellaneous Tibial Fractures
There are other, often more subtle, fractures about the knee. Some of these are included in the OTA type A1 category, which includes avulsion fractures of the tibial spine (see Fig. 6-27), fibular head, and tibial tuberosity (see Fig. 6-28, also Fig. 6-20). Tibial tuberosity fractures are classified into three simple categories (see Fig. 6-29). Type I fractures may be treated conservatively, whereas types II and III usually require fixation with a cancellous screw and washer.
Tibial tuberosity fractures (Fig. 6-29)
Type I: Small avulsed fragments (39% of fractures)
Type II: Anterior hinging of the entire tuberosity (18%)
Type III: Tuberosity fracture extends into the joint space (43%)
Tibial eminence or spine fractures are similarly classified on the basis of the degree of displacement. Type I and II fractures can be treated conservatively, whereas type III fractures require surgical intervention.
Tibial spine fractures (see Fig. 6-30)
Type I: Undisplaced (16% of fractures)
Type II: Elevated anteriorly (39%)
Type III: Displaced (45%)
A Segond fracture (see Chapter 2) is an avulsion at the insertion of the middle third of the capsular ligament on the proximal lateral tibia. This injury is frequently associated with ACL and meniscal tears (see Fig. 6-31). Bone bruises are also associated with ligament tears. Stress fractures may also occur in the proximal tibia and fibula.

 Fig 6.26 Coronal (A) and sagittal (B) computed tomographic (CT) images demonstrating a lateral split fracture with marked depression. Reduction was accomplished (C and D) with bone graft and screws and washers.
Fig 6.26 Coronal (A) and sagittal (B) computed tomographic (CT) images demonstrating a lateral split fracture with marked depression. Reduction was accomplished (C and D) with bone graft and screws and washers.

 Fig 6.27 Anteroposterior (AP) and lateral radiographs demonstrating an undisplaced (type I) tibial spine fracture (arrow).
Fig 6.27 Anteroposterior (AP) and lateral radiographs demonstrating an undisplaced (type I) tibial spine fracture (arrow).
Physeal fractures about the knee are uncommon. Fractures of the tibial physis account for only 0.5% to 3% of all physeal injuries. Femoral physeal fractures are slightly more common due to the ligament support about the knee. The ligaments extend below the tibial physis providing additional support, but attach to the femur just below the physis (see Figs. 6-32 and 6-33). Radiographic features may be subtle if the fracture is not displaced. MRI is preferred to detect and follow up physeal injuries (Fig. 6-33B).
SUGGESTED READING
Berquist TH. Osseous and myotendinous injuries about the knee. Magn Reson Imaging Clin N Am. 2007;15:25–38.
Dezell PB, Schils JP, Recht MP. Subtle fractures about the knee: Innocuous-appearing yet indicative of internal derangement. AJR Am J Roentgenol. 1996;167:699–703.
Ipsilateral Femoral and Tibial Fractures
Ipsilateral combined injuries of the tibia and femur present significant management issues. The injury has been termed floating knee. These fractures are usually related to high-velocity trauma, such as motor vehicle accidents. Local and distant injuries are common. Approximately 60% of fractures are open further complicating treatment approaches.
Fraser classification: (see Fig. 6-34)
Type I: Shaft fracture without articular involvement (71% of injuries)
Type IIA: Femoral fracture with tibial plateau fracture (16.5%)
Type IIB: Femoral articular and tibial nonarticular fracture (4.5%)
Type IIC: Both articular surfaces (8%)

 Fig 6.28 Lateral radiograph demonstrating a tibial tuberosity avulsion (arrow) with the fracture extending into the joint space (type III).
Fig 6.28 Lateral radiograph demonstrating a tibial tuberosity avulsion (arrow) with the fracture extending into the joint space (type III).
Treatment usually requires internal fixation, though external fixation may be included especially when there are associated open wounds (see Fig. 6-35). See Chapter 5 for review of femoral treatment options.
SUGGESTED READING
Fraser RD, Hunter GA, Waddel JP. Ipsilateral fracture of the femur and tibia. J Bone Joint Surg. 1978;60B:510–515.
Rand JA, Berquist TH. The knee. In: Berquist TH, ed. Imaging of orthopaedic trauma, 2nd ed. New York: Raven Press; 1992:333–432.
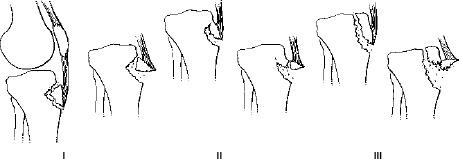
 Fig 6.29 Illustration of tibial tuberosity fractures. Type I—simple avulsion, type II—anterior hinging of the entire tuberosity, and type III—fracture extending into the joint space.
Fig 6.29 Illustration of tibial tuberosity fractures. Type I—simple avulsion, type II—anterior hinging of the entire tuberosity, and type III—fracture extending into the joint space.
Soft Tissue Injuries
Soft tissue injuries about the knee may be associated with obvious or subtle (bone bruises) osseous fractures. This section will focus on those injuries that require some type of fixation device. The ACL is most often injured (39%). Injury may result from multiple mechanisms including forced valgus and external rotation, external rotation and hyperextension, internal rotation with extension, and forward displacement of the tibia. Most patients describe hearing a loud pop and are unable to bear weight. Up to 75% have an acute hemarthrosis. Also, 70% have other associated injuries including the MCL and posterior horn of the medial meniscus. When all three occur together it is termed O’Donoghue’s triad. Combined ACL, MCL, and medial capsular tears account for 30% of soft tissue injuries about the knee. Lateral collateral ligament injuries occur in 19% and posterior cruciate ligament (PCL) tears in 5% of ligament injuries to the knee.
Imaging of patients with suspected soft tissue injury should begin with radiographs. Certain injuries may be evaluated with ultrasound or conventional/CT arthrography. However, in most cases MRI is the technique of choice to evaluate the ligaments, tendons, menisci, and articular cartilage. Following repair, baseline radiographs are important to evaluate the fixation devices and tunnels for ligament repair. A hyperextended cross-table lateral has been included to evaluate the position of the tibial tunnel compared to the condylar roof in patients with ACL repairs (see Fig. 6-36).
Treatment Options
Treatment options for ligament repair include primary repair and reconstruction. With the former, the ligament is repaired by suturing the tear together. This approach may be most useful with ACL avulsions with the bone reattached to the tibia. In most cases reconstruction is preferred because results are superior. Autografts (patellar tendon, hamstring, orother tendon grafts), allografts, and synthetic materials have been used. Depending on the extent of repair the procedure can be done arthroscopically or as an open procedure. Grafts for the cruciate ligament are held in place with interference screws in most cases (see Fig. 6-37). However, staples, screws with variegated washers, and other fixation devices may also be used. It is important that the tunnels for cruciate repair are placed in isometric position (Fig. 6-36).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


