, Marilyn J. Siegel2, Tomasz Miszalski-Jamka3, 4 and Robert Pelberg1
(1)
The Christ Hospital Heart and Vascular Center of Greater Cincinnati, The Lindner Center for Research and Education, Cincinnati, OH, USA
(2)
Mallinckrodt Institute of Radiology, Washington University School of Medicine, St. Louis, Missouri, USA
(3)
Department of Clinical Radiology and Imaging Diagnostics, 4th Military Hospital, Wrocław, Poland
(4)
Center for Diagnosis Prevention and Telemedicine, John Paul II Hospital, Kraków, Poland
Abstract
The heart lies in the middle mediastinum within the pericardial sac. The pericardial sac is formed by two layers: the outer layer known as the fibrous pericardium and the inner layer known as the serous pericardium. The serous pericardium contains two layers: visceral and parietal. The inner visceral layer covers the surface of heart and base of the great vessels. At the level of the great vessels, it reflects and becomes the parietal layer, which lines the thick fibrous pericardium. The fibrous pericardium fuses with the base of the great vessels and the diaphragm and it is attached to the sternum by the sternopericardial ligament.
The heart lies in the middle mediastinum within the pericardial sac. The pericardial sac is formed by two layers: the outer layer known as the fibrous pericardium and the inner layer known as the serous pericardium. The serous pericardium contains two layers: visceral and parietal. The inner visceral layer covers the surface of heart and base of the great vessels. At the level of the great vessels, it reflects and becomes the parietal layer, which lines the thick fibrous pericardium. The fibrous pericardium fuses with the base of the great vessels and the diaphragm and it is attached to the sternum by the sternopericardial ligament.
The pericardial cavity is the potential space between the visceral and parietal serous layers. It contains a small amount of serous fluid, known as pericardial fluid. There are two recesses within this cavity: the transverse sinus and the oblique sinus. The transverse sinus is bounded anteriorly by the aorta and pulmonary artery and posteriorly by the roof of the left atrium and the right pulmonary artery. Laterally, the transverse sinus communicates with the rest of pericardial cavity. The oblique sinus is a blind-ending cavity behind the left atrium. Its borders are formed by reflections of serous pericardium. The upper border is formed by the pericardium between the superior pulmonary veins, the right border by the pericardium around the right pulmonary veins and inferior vena cava, and the left border by the pericardium around the left pulmonary veins (Fig. 2.1).
Fig. 2.1
A 3D volume-rendered depiction of the normal heart. Panel (a) anterior view. Panel (b) left view. Panel (c) posterior view. Panel (d) right view. Panel (e) superior view. Panel (f) inferior view. Ao arch aortic arch, Ao asc ascending aorta, Ao desc descending aorta, IVC inferior vena cava, MPA main pulmonary artery, LA left atrium, LAD left anterior descending coronary artery, LLPV left lower pulmonary vein, LPA left pulmonary artery, LUPV left upper pulmonary vein, LV left ventricle, PDA posterior descending coronary artery, RA right atrium, RCA right coronary artery, RPA right pulmonary artery, RLPV right lower pulmonary vein, RUPV right upper pulmonary vein, RV right ventricle, RVOT right ventricular outflow tract, SVC superior vena cava, RAA right atrial appendage
Figure 2.2: CT image demonstrating the transverse and oblique sinuses.
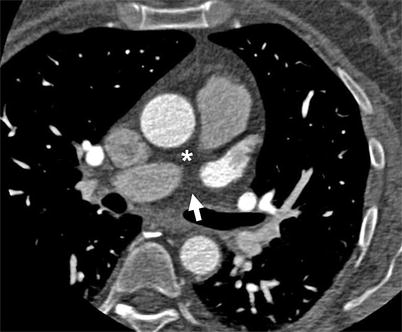
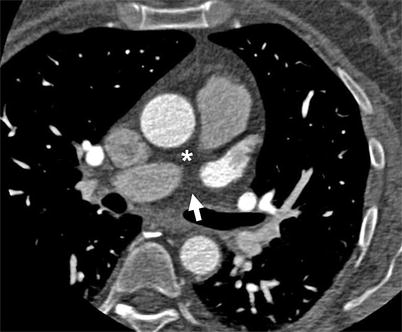
Fig. 2.2
A CT image illustrating the transverse (asterisk) and oblique sinuses (arrow)
2.1 Right Atrium
The right atrium (RA) lies to the right and anterior to the left atrium (LA). It contains three basic components: the venous component, the appendage, and the vestibule of the tricuspid valve (Fig. 2.3).
Fig. 2.3
The anatomy of the right atrium contains three sections: the venous (double arrow), appendage (RAA), and the vestibule (asterisk). Ao aorta, CS coronary sinus, IVC inferior vena cava, MPA main pulmonary artery, RAA right atrial appendage, RV right ventricle, SVC superior vena cava, TV tricuspid valve
The triangular-shaped right atrial appendage is separated externally from the superior and inferior vena cava by the terminal groove. Internally, the terminal groove corresponds to the location of the terminal crest which extends inferiorly from the left side of the superior vena cava (SVC) entrance to the right side of the inferior vena cava (IVC) opening where it ramifies into an isthmus between the IVC and tricuspid valve (cavotricuspid isthmus) [1, 2]. The most characteristic feature of the morphology of the right atrial appendage is the pectinate muscles that extend around the entire parietal margin of the atrioventricular junction. The sinus node is located within this chamber, usually lying to the right of the superior cavoatrial junction [3].
The venous portion of the right atrium is positioned in the right side of the right atrium. There is no well-defined border between the appendage and the venous component of the right atrium [4]. Superiorly and inferiorly the venous component connects with the SVC and IVC, respectively. The posterior atrial wall between the orifices of the cavae forms the intercaval area [2]. The opening of the SVC has no valve. The IVC orifice is guarded by the Eustachian valve, which extends anteriorly and to the left from the lateral margin of the IVC to the sinus septum (Eustachian ridge) [2, 5]. The coronary sinus enters the RA close to the right side of the IVC ostium. The Thebesian valve, a small crescent-shaped, sometimes fenestrated flap [2], accompanies the coronary sinus orifice.
The posterior aspect of the RA contains the atrial secundum, which is virtually confined to the fossa ovalis. The superior rim of the fossa ovalis is an extensive infolding between the venous component of the right atrium and the right pulmonary veins, while the posterior inferior rim is directly continuous with the sinus septum that separates the orifices of the IVC and the coronary sinus. The anteroinferior margin is adjacent to the triangle of Koch (see description below) [5–7]. The floor of the fossa ovalis is formed by a fibromuscular flap valve that fuses with the rim of the fossa ovalis, resulting in closure of the fossa. In 25–30 % of individuals, the anatomical fusion is incomplete (usually at the anterosuperior margin), leading to interatrial shunting in some individuals [2].
The vestibular component is positioned in the left side of the right atrium and forms the outlet of the RA. It contains the triangle of Koch, which is an anatomical landmark for the atrioventricular node (AV node). The triangle of Koch is demarcated by (a) the tendon of Torado, a fibrous structure formed by the junction of the Eustachian valve (valve of the IVC) and the Thebesian valve (valve of the coronary sinus); (b) the ostium of the coronary sinus posteriorly; and (c) the septal leaflet of the tricuspid valve [5, 8]. Of note, the septal isthmus is not truly septal but rather the inferior part of the anteromedial RA wall [2].
2.2 Left Atrium
The left atrium (LA) is located to the left and posterior to the RA. Like the RA, the LA has three basic components: (1) the left atrial appendage, (2) the venous component, and (3) the vestibule of the mitral valve. Unlike the RA, the venous component is considerably larger than the appendage.
The left atrial appendage is positioned at the left atrial margin. In contrast to the RA appendage, it is a smaller, fingerlike structure. It has a discrete junction with the LA venous component, which, unlike the RAA junction, is not marked by a terminal crest or terminal groove. Internally it contains a complex network of muscular ridges (pectinate muscles) and membranes with a comb-like appearance [5].
The venous component is located in the posterior LA and contains the orifices of the pulmonary veins. Typically, four distinct pulmonary venous ostia are present, although anatomical variability frequently occurs [9]. The right and middle lobe veins usually unite, so two trunks from each lung are formed (bilateral superior and inferior veins). The pulmonary veins perforate the fibrous layer of the pericardium and open separately into the upper and back part of the LA. Not infrequently, the two left pulmonary veins have a common opening and the three veins on the right side have separate openings into the left atrium. Occasionally, there is a left middle pulmonary vein. Therefore, the number of pulmonary veins opening into the left atrium can vary between three and five in the healthy population [10, 11].
Internally, ridge-like structures separate the ostia of the superior and inferior pulmonary veins [11]. The left pulmonary vein ostia are positioned more superiorly than the right pulmonary vein ostia. The left pulmonary veins are situated between the LA appendage and the descending aorta. The right pulmonary veins project behind the SVC or the RA. The atrial wall infolding between the entrances of the right pulmonary veins and the SVC forms the superior rim of the fossa ovalis.
The vestibule of the mitral valve forms the outlet of the LA and is positioned to the left and anteriorly in the LA. It forms part of the mitral isthmus which is situated between the left inferior pulmonary vein and mitral valve annulus [12]. The coronary sinus runs externally along the inferior aspect of the vestibular component at a variable distance from the mitral valve annulus and enters the RA.
2.3 Cardiac Valves
The cardiac valves are in close proximity to each other. The leaflets of three of the valves are in fibrous continuity, while the pulmonary valve leaflets are exclusively supported by a free-standing muscular infundibulum. The fibrous continuation between the mitral and aortic valve is established by the continuity between the anterior leaflet of the mitral valve (called the aortic leaflet) and the noncoronary and right coronary leaflets of aortic valve (Fig. 2.4). Laterally the fibrous tissue is thickened and forms the right and left fibrous trigones. The right fibrous trigone joins the membranous septum, creating the central fibrous body. Superiorly the aorto-mitral continuity extends into the interleaflet triangles positioned at the level of the noncoronary leaflet of the aortic valve. The central fibrous body brings the aortic and mitral valves into fibrous continuity with the tricuspid valve. The septal leaflet of the tricuspid valve is attached to the right ventricular aspect of the membranous septum which divides the septum atrioventricular and interventricular components. The morphology of the individual cardiac valves is elucidated further in the following sections.
Fig. 2.4
A rendition of the continuity between the mitral and aortic valves. The membranous septum is in continuation with the right fibrous trigone and the interleaflet triangle between the right and noncoronary aortic valve leaflets. The right fibrous trigone and the membranous septum form the central fibrous body of the heart. RCA right coronary artery, LMCA left main coronary artery
2.4 Right Ventricle and Tricuspid Valve
The right ventricle (RV) extends from the atrioventricular junction toward the left to the cardiac apex and cephalad to the ventriculoarterial junction. The tricuspid and pulmonary valves demarcate the RV from the right atrium and pulmonary trunk, respectively. The RV has three distinct components: (1) the inlet, (2) the apical, and (3) the outlet (Fig. 2.5) [13].
Fig. 2.5
The anatomy of the right ventricle. Note the presence of the inlet, apical, and outlet components. Ao aorta, IVC inferior vena cava, MPA main pulmonary artery, PM papillary muscle, PV pulmonary valve, RA right atrium, RAA right atrial appendage, SMT septomarginal trabeculations, SVC superior vena cava, TV tricuspid valve
The inlet portion of the right ventricle surrounds the tricuspid valve, extending from its annulus to the insertions of the papillary muscles to the ventricular walls. The tricuspid valve annulus is positioned closer to the cardiac apex than the mitral valve annulus. It divides the membranous septum into atrioventricular (partition between the RV and LA) and interventricular sections (partition between the RV and LV). Generally, the tricuspid valve has three leaflets, although other configurations can be encountered. A distinguishing feature of the tricuspid valve is the direct attachment of its septal leaflet (tendinous cords attach directly to the interventricular septum). The septal leaflet is supported by an inferior papillary muscle (not always present) and a more constant medial papillary muscle. The anterosuperior leaflet is large and is usually supported by a prominent anterior papillary muscle arising from the apical portion of septomarginal trabeculations. The commissure between the septal and anterosuperior leaflets is supported by a medial papillary muscle. The inferior leaflet (also known as the mural or posterior leaflet) attaches to the diaphragmatic aspect of the RV via cords that insert either into small papillary muscles or into the ventricular wall itself.
The apical trabecular part of the RV extends to the cardiac apex and contains coarse trabeculations.
The outlet portion of the RV consists of the infundibulum, a circumferential muscular structure that supports the leaflets of the pulmonary valve. The infundibulum is contiguous with the supraventricular crest, which comprises the ventriculo-infundibular fold and outlet septum (infundibular septum). The ventriculo-infundibular fold is part of the inner curve of the heart and it separates the tricuspid and pulmonary valves. The outlet septum (infundibular septum) separates the subpulmonary and subaortic outflow tract and also the aortic and pulmonary valve leaflets. The supraventricular crest inserts between the anterosuperior and posteroinferior limbs of septomarginal trabeculation (septal band), which is the muscular strap extending toward the RV apex reinforcing the septal aspect of the RV.
The anterosuperior limb of septomarginal trabeculation extends to the attachment of the pulmonary leaflet, overlying the outlet septum. The posteroinferior limb extends to the interventricular portion of the membranous septum, usually giving rise to the medial papillary muscle. The septomarginal trabeculation also gives rise to other muscular straps. Those trabeculations that extend from the anterior margin of the septomarginal trabeculation to the parietal RV wall form the septoparietal trabeculations. At the RV apex, the septomarginal trabeculation is divided into smaller straps. Some of these extend into the apical part of the RV and some of them support the tension apparatus of the tricuspid valve. One prominent trabeculation becomes the anterior papillary muscle, while another creates a moderator band, which attaches to the anterior papillary muscle and runs to the parietal wall of the RV.
Different segmental models of the RV have been proposed and are generally based on the division of the RV free wall into equal thirds (basal, mid-cavity, and apical) perpendicular to the long axis of the heart. Each level is also circumferentially divided into equal number of segments (i.e., three segments: anterior, lateral, and inferior) [14]. Several distinctive features help to distinguish the RV from the left ventricle. These features include (a) the closer proximity of the tricuspid valve to the apex, (b) the presence of uniformly coarse apical trabeculations, (c) trileaflet configuration of the atrioventricular valve with direct attachment of the septal leaflet to the interventricular septum, (d) presence of more than two papillary muscles, and (e) presence of the moderator band [14].
2.5 Left Ventricle and Mitral Valve
The left ventricle (LV) extends from the atrioventricular junction to the left and anterior to the heart apex and cephalad to the ventriculoarterial junction. The mitral and aortic valves separate the LV from the LA and aorta, respectively. Similar to the RV, the LV can be subdivided into three components: (1) inlet, (2) apical, and (3) outlet. The distinction between them, especially between the inlet and outlet portions, is less clear than in the RV.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree