Do you see the branch that has been cut out on the left side of the tree in the picture? If the branch had been removed due to disease, where would you look to see if the disease had resurfaced? You would look really carefully at the remainder of that branch. You would also probably check the rest of the tree to be sure there was no new sign of disease in any other branches.
When imaging the patient with known or suspected breast cancer ( Chapter 17 ), we focused our attention on the affected ductal system to evaluate extent of disease. Likewise, when looking for recurrent cancer in women who have undergone breast-conserving therapy (BCT), we will focus on the ductal system where the cancer developed. We will start by looking at the lumpectomy scar and then within that ductal system.
In this chapter, we will review benign surgical changes and then turn our attention to detection of residual and recurrent breast cancer. We will give you our best tips for differentiating benign postoperative changes from those that may represent cancer.
Reduction Mammoplasty and Mastopexy
Reduction mammoplasty, mastopexy, and breast augmentation are typically performed by plastic surgeons rather than breast surgeons. Breast augmentation is discussed in Chapter 19 .
Reduction mammoplasty is performed to reduce the overall size of the breasts. It is often performed for women with back or shoulder problems due to the weight of large breasts. After mastectomy with reconstruction, the contralateral breast may be reduced to improve symmetry of breast size. Mastopexy, or a “breast lift,” is similar in surgical approach, but breast tissue is not removed. This is performed for women with ptotic breasts wishing to reverse the effects of living on a gravitational planet.
For both reduction mammoplasty and mastopexy, a keyhole incision is made ( Fig. 18-1 ). The scars of reduction mammoplasty are therefore seen primarily on the inferior breasts.
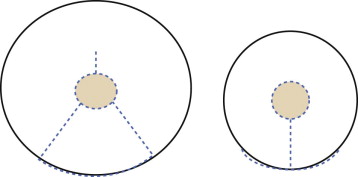
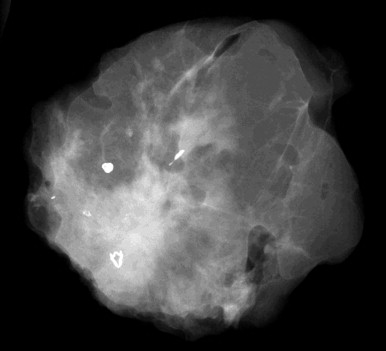
The breast tissue has a “swirled” appearance in the inferior aspect of the mediolateral oblique (MLO) views—the ducts are heading toward the prior location of the nipple, which has been moved up to a perkier location ( Fig. 18-2 ). Isolated islands of breast tissue may be seen and are the result of separation of the tissue during surgery ( Fig. 18-3 ). Dermal calcifications are very common in the scar tissue ( Fig. 18-4 ). Oil cysts are also very common after both reduction and mastopexy ( Fig. 18-5 ).
Benign Surgical Biopsy
Surgical Biopsy Terminology
“Lumpectomy” literally means removal of a palpable lump. However, by convention, “lumpectomy” is used to describe the surgical removal of a cancer, regardless of whether or not it is palpable. “Excisional biopsy” refers to the surgical removal of an entire breast lesion. For example, a palpable fibroadenoma may undergo surgical excision. “Incisional biopsy” indicates a surgical biopsy in which only a portion of a lesion is removed. This type of biopsy may be performed when a core biopsy shows a high-risk lesion or was benign discordant. The goal of incisional biopsy is to obtain tissue for diagnosis rather than to completely remove a palpable finding or known carcinoma.
Changes of Surgical Biopsy
In the immediate postoperative period, small hematomas and seromas are common. Large fluid collections necessitating drainage are very uncommon. Fluid collections in the biopsy cavity decrease in size and have typically resolved by the time imaging is next performed. Imaging after a benign surgical biopsy may be helpful to confirm that the targeted lesion has been sampled or removed, but it is not required.
The first postoperative mammogram is often obtained 6 to 12 months after biopsy. Distortion from scarring will be worst on this earliest mammogram. The size and density of the scar will improve with time. Scars are planar ( Fig. 18-6 ). After about 5 years, distortion after benign biopsy becomes difficult to identify in most women. Significant architectural distortion more than 10 years after a benign biopsy is uncommon and should be viewed with suspicion. Don’t assume that the architectural distortion you see is due to a fibroadenoma that was removed in 1995! Comparison with older mammograms or diagnostic evaluation may be indicated.
Fat necrosis and benign dystrophic calcifications may evolve over the first year or two. The detritus of surgery may also be seen. Sutural calcifications may develop ( Fig. 18-7 ). A piece of retained hookwire may be seen occasionally ( Fig. 18-8 ).
Surgery for Breast Cancer
Lumpectomy for Carcinoma
Imaging of women undergoing BCT is important for detecting residual disease in the early postoperative period (prior to radiation therapy [RT]), for identifying recurrent breast cancer after therapy, and for diagnosing metachronous breast cancer ( Box 18-1 ).
- •
Ipsilateral pre-RT mammogram (all calcification cases, others on a case-by-case basis)
- •
Ipsilateral mammogram every 6 months for 2 to 3 years
- •
Contralateral mammogram every year
- •
Magnification views of the lumpectomy bed with each mammogram for 5 years
Residual Disease
There are several opportunities to identify residual disease in women undergoing BCT. These include positive or close margins of the excised specimen at pathologic examination, a specimen radiograph showing the lesion near the radiographic margin, and the pre-RT mammogram.
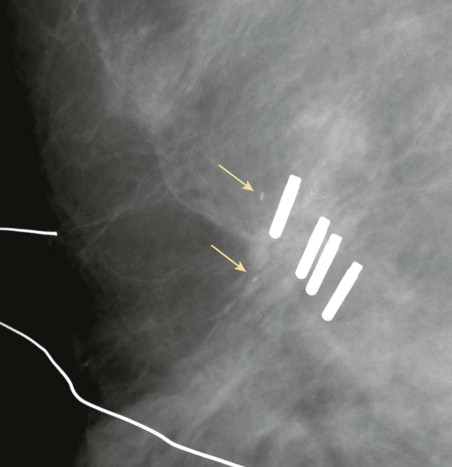
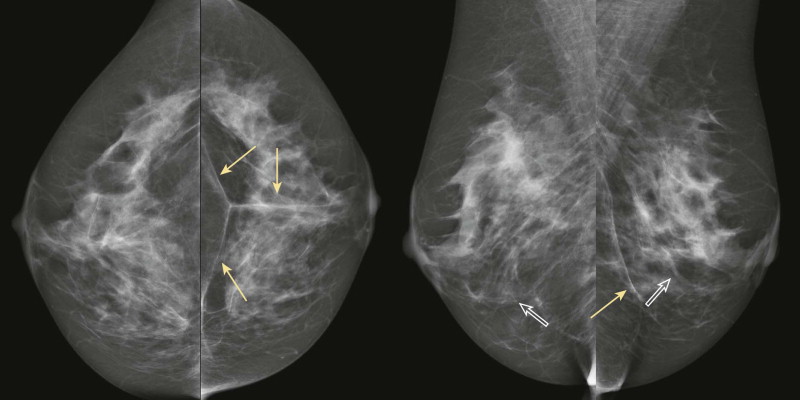
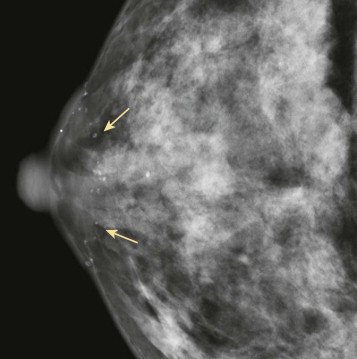
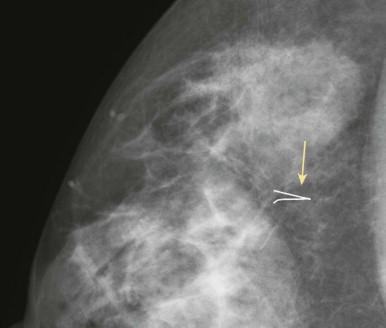
A pathology report of positive or close margins is associated with a high likelihood of cancer remaining in the breast. If the patient had calcifications associated with the cancer, magnification views of the operative region prior to re-excision may demonstrate concerning residual calcifications that can be localized as part of the re-excision surgery ( Fig. 18-9 ). These calcifications may be difficult to visualize because of the postoperative changes, so look back at the preoperative magnification views for comparison.
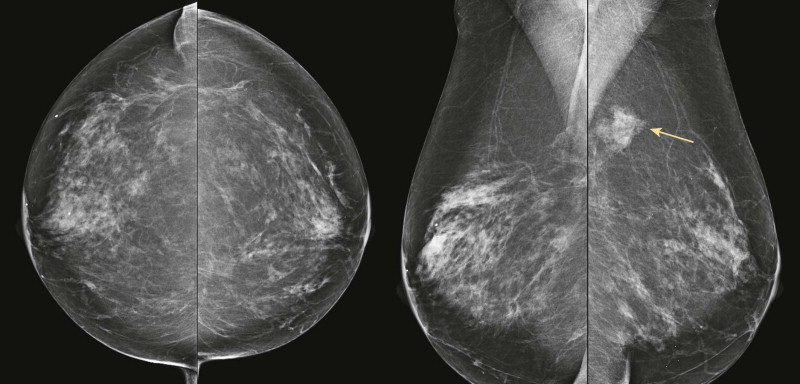
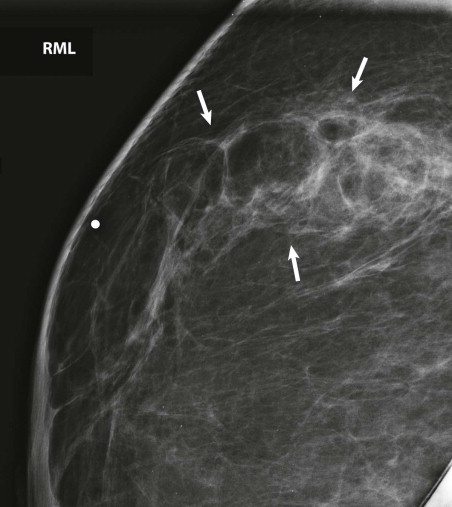
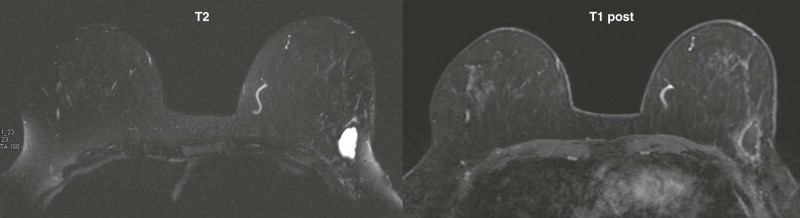
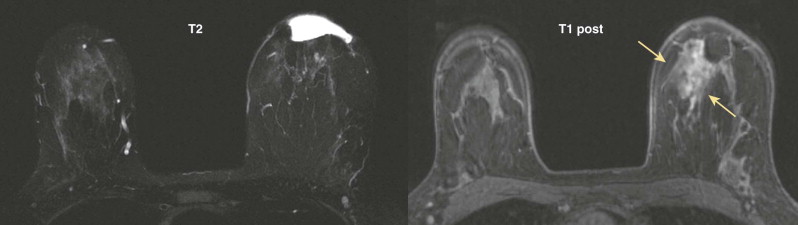
Magnetic resonance imaging (MRI) is also very useful in assessing the amount of residual disease to assist decision making about whether another excision is likely to be successful ( Fig. 18-10 ). It can also detect additional previously occult lesions distant from the site of known tumor. When the MRI is abnormal ( Fig. 18-11 ), additional disease should be confirmed by biopsy before mastectomy is recommended. False-positive and false-negative MRI findings are fairly common; the sensitivity and specificity of MRI in identifying residual cancer in women with positive or close margins are 61.2% and 69.7%, respectively. A negative MRI does not indicate that the patient can forgo re-excision. Microscopic or nonenhancing carcinoma may still be present.
A pathology report of negative margins does not ensure that there is no residual disease present. Pathologic assessment of margins is an imperfect science; four to five small samples of tissue are taken from the areas that appear most suspicious for cancer on the surface of the lumpectomy tissue by gross inspection. Pathologists estimate that around 16% of the surface of a lumpectomy specimen is sampled for microscopic examination.
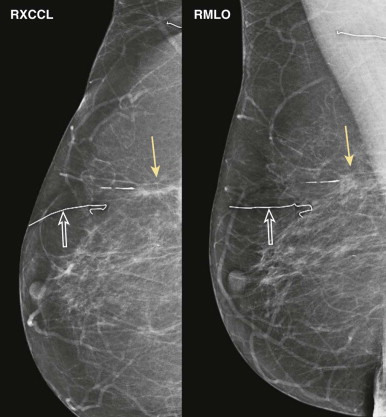
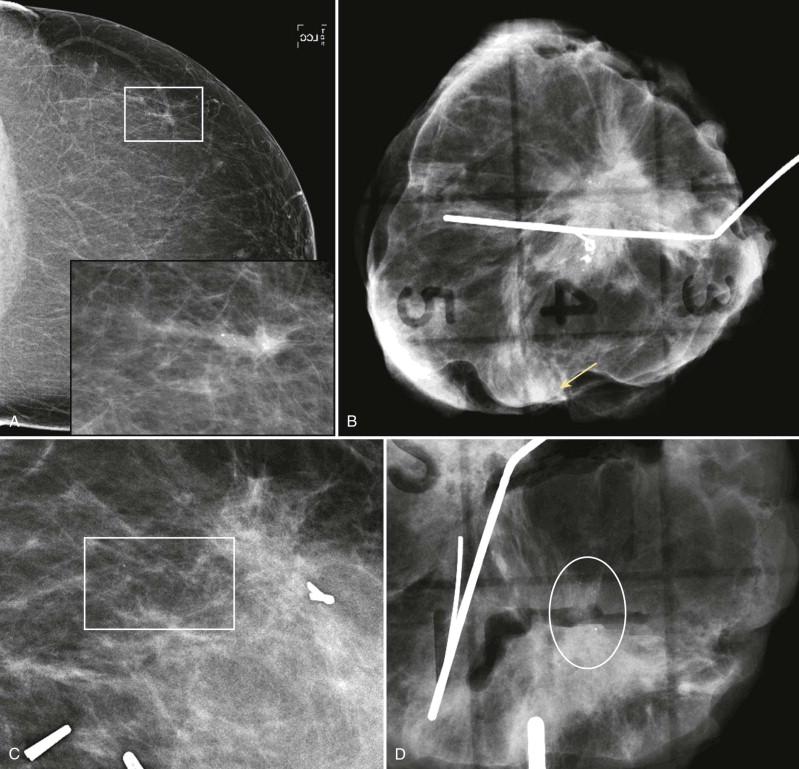
Radiologists have an opportunity to help; the specimen radiograph not only confirms whether the lesion was removed or not, but also where the lesion was located within the specimen ( Fig. 18-12 ). If the lesion is at or near an edge, the chance of incomplete excision is 79% to 98%. In these cases, communication with the surgeon in the operating room may guide immediate resection of the suspect margin. This can result in a negative margin, eliminating the need for additional surgery.
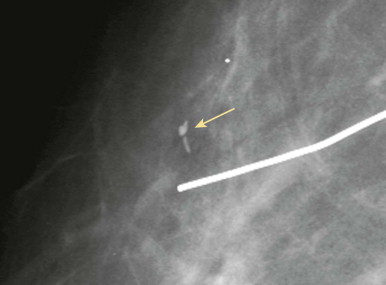
Radiologists have one more opportunity to identify residual disease: the pre-RT mammogram . In the early BCT trials, women with residual calcifications in or near the lumpectomy bed had a local recurrence rate of 60% compared with a 6% recurrence rate of women overall. That’s a huge difference, so we have a job to do! For women with breast cancer presenting as calcifications with or without an associated mass, an ipsilateral mammogram with magnification views prior to RT may identify residual calcifications in or near the lumpectomy bed ( Fig. 18-13 ). If a pre-RT mammogram is not obtained and residual carcinoma is identified after RT is administered, the patient must undergo mastectomy.