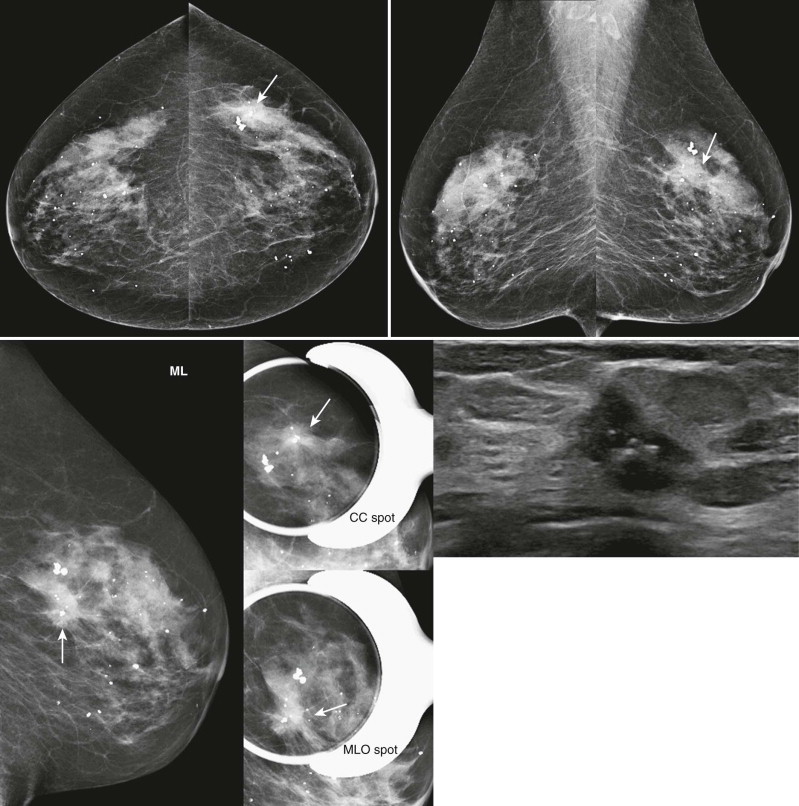
Let’s see. A screening recall. Is it a real finding? It looks kind of ugly on the screening views. The mediolateral oblique (MLO) spot looks fine, but the craniocaudal (CC) spot may still have something there. What next? Rolled CC views? Ultrasonography (US)? Magnetic resonance imaging (MRI)? Should I just let her go? It’s not always easy to decide if a screening finding is significant.
Is it real, or is it cubic zirconium? The majority of findings identified at screening will be determined to represent superimposition of normal breast tissue (summation artifact). The role of diagnostic evaluation is to separate benign findings from those that are potentially malignant. The important questions include whether the finding is new or developing, persists on spot compression, and is suspicious based on its imaging features. If the finding is suspicious, then location becomes important. A one-view finding must be localized if possible prior to biopsy.
In this chapter, we will focus on the diagnostic evaluation of the patient recalled from screening for a mass or asymmetry. We will give you tools to localize lesions in two orthogonal projections. Then we’ll need to decide on our level of suspicion for the lesion and whether biopsy is warranted. Evaluation of breast calcifications is discussed further in Chapter 6: Calcifications Made Easy .
The Screening Recall
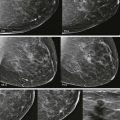
Our routine imaging for an abnormal screening mammogram includes a true lateral view (mediolateral [ML] or lateromedial [LM]) and spot compression views of the finding ( Fig. 4-1 ). Additional imaging often follows and may include additional mammographic views and US.
The goals of the workup are to decide whether the finding represents a true lesion and, if so, to localize it in two orthogonal projections, and determine its level of suspicion. These goals are often achieved simultaneously. For example, an ML view obtained to evaluate a finding seen in the MLO view may show that the finding represents superimposed breast tissue. Alternatively, if the finding represents a true mass, the ML view may help localize it to the medial or lateral breast.
True Lateral View
The true lateral view is helpful in determining the location of the finding because this can be misjudged on the MLO view. Obtaining a true lateral view is also very helpful for planning if stereotactic or wire-localized biopsy is performed.
The true lateral view may be ML or LM. So, which to choose? Remember that the view is named for the direction of the x-ray beam. We want the lesion to be as close to the image receptor as possible to maximize sharpness. If the lesion is in the lateral breast, then an ML view will put the lesion closest to the receptor. If the lesion is medial, then the LM view is preferred. If we are not sure whether the finding is medial or lateral, then an ML is performed because statistically, most cancers are located in the lateral breast.
Spot Compression Views
Spot compression views are often helpful in deciding whether a finding represents summation artifact or a true lesion. They are also used to confirm the location of a finding and to help determine the level of suspicion. Although it may seem more efficient to go straight to US when a mammographic finding is seen in two projections, spot compression views result in an increase in cancer detection of about 18%.
When a cancer undergoes focal (spot) compression, the abnormal tissue will typically appear more dense than the surrounding tissues, and mass borders are more clearly seen. These views may show a one-view asymmetry to represent a focal asymmetry or a mass. A mass with obscured margins may be shown to have spiculated margins on spot compression views. Associated findings such as architectural distortion are often better seen than on the screening views. When normal tissue undergoes spot compression, it will spread out and become less dense; the normal, respectful breast architecture becomes more apparent.
Spot compression views (“spots”) should be obtained in both CC and MLO projections if the finding is seen on both views. Spot compression views may be performed with or without magnification (“spot mags”). The advantage of using magnification with spot compression is the ability to see fine architecture and calcifications well, although the disadvantage is lower contrast. Whether or not to use magnification with spot compression is really one of personal preference. As you can see from our many case studies, we typically perform spot compression without magnification.
Go ahead and skip the spot compression views when the mass for which the patient is being recalled is very likely to represent a cyst ( Fig. 4-2 ). Spot compression views are often uncomfortable, but when there is a large cyst present they can be downright painful. So spare your patient the discomfort and start with US if the mass is likely to be a cyst.

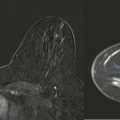
Tomosynthesis and Other Imaging
Digital breast tomosynthesis (DBT) gives us a not-quite three-dimensional evaluation of the breast. The use of DBT in diagnostic breast imaging is evolving. Many other mammographic views (rolled CCs, off-angle, tangential views, etc.) can be very helpful in both localizing the lesion and assessing the level of suspicion. Be creative!
Ultrasonography can be invaluable in identifying breast cancer, but we must first know when and where to look. As in spot compression views, an additional 20% of cancers will be detected when US is used appropriately as a part of the diagnostic evaluation. More on this later.
Breast MRI is rarely needed in the diagnostic evaluation of a mammographic finding. Here’s the problem: a negative MRI does not mean that the mammographic finding is not cancer. Additional mammographic views and US should be used to evaluate the finding and establish the level of suspicion. Occasionally, MRI is useful to localize a suspicious mammographic finding seen in one view that is not amenable to US or stereotactic biopsy.
Determining the Location of a Two-View Finding
When we see a finding that we think is concerning, we will want to localize it in two orthogonal views. Sometimes this is easy, but it may be especially challenging on a complex or dense mammogram. Even when the location on the CC and MLO views is obvious, we’ll need to remember that the MLO cannot be treated like a true lateral view when determining the location of a lesion. Localization is important because we will need to know where to focus our attention before we do an US.
There are a few things to keep in mind when localizing a finding. The lesion should have similar size, shape, and imaging characteristics in both CC and MLO views. The depth of the lesion should be similar on all mammographic views so long as the nipple is in profile.
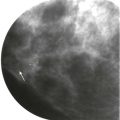
Lesion Depth
A finding should have similar depth (distance from the nipple) on all mammographic views as long as the nipple is in profile ( Fig. 4-3 ). A mass that is in the anterior breast on the CC view will not correspond to a finding in the posterior breast on the MLO view as long as the nipple is relatively in profile. If the nipple rolls under the breast on the CC view or to the side on the MLO view, the depth of the lesion could appear much different on the CC and MLO views ( Fig. 4-4 ).


Account for Obliquity on the MLO View
For a finding seen in both CC and MLO views, we need to remember that an MLO view is typically obtained at a 30- to 60-degree angle, although a true lateral view is obtained at 90 degrees. We have to mentally account for the differences in obliquity between the MLO and a true lateral view ( Fig. 4-5 ). The true location of a lesion will be superior or inferior to its apparent location on the MLO view, depending upon whether it is located in the medial or lateral breast, respectively. The location of a far lateral or far medial finding will be more affected by the obliquity on the MLO view than a more centrally located finding.

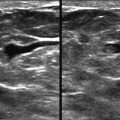
Correlating between Mammography and Ultrasonography
Understanding the location of a lesion on mammography prior to US or biopsy is important. Using the information available from the mammogram, it is often possible to have a good idea of the location and US appearance of a finding before you scan. If US is performed in the incorrect location, a mammographic finding may incorrectly be assumed benign ( Fig. 4-6 ).

The size, shape, and other characteristics of the lesion on the mammogram should be similar to the appearance on US ( Fig. 4-7 ). Other landmarks can also sometimes be used to increase your confidence that you are examining the correct finding. For example, a calcified oil cyst, fibroadenoma, or intramammary lymph node adjacent to the suspicious finding may be identified by US.

In addition to the “o’clock position” and depth of a lesion, it can be helpful to consider the location of a lesion relative to the central core of fibroglandular tissue. Ask yourself whether the lesion is at the border of the fibroglandular tissue, more centrally within this tissue, or in the retroglandular fat. Finding a lesion by US with the same position with respect to the fibroglandular tissue increases confidence that it corresponds to the mammographic finding.
Keep in mind that with mammography, the technologist pulls the breast tissue away from the chest wall. For US, the patient is recumbent and the breast tissue flattens toward the chest wall. As a result, lesions may appear closer to the pectoral muscle than one might expect based on the mammographic location. For example, a mass in the middle third of the breast on mammography may appear to abut the pectoralis muscle on US.
If you are uncertain whether the US and mammographic findings are the same lesion, but the US and mammographic findings individually are both suspicious enough to warrant biopsy, there is no real need to prove that they correspond before performing a biopsy. Place a clip after ultrasound-guided core biopsy and perform postprocedure mammography, which will show whether they correspond. Be ready, however, to also perform a stereotactic biopsy if the clip is not located in the suspicious mammographic finding. Hey, it happens.
Determining the Location of a One-View Finding
Let’s say that your colleague identified a suspicious one-view asymmetry on screening and now you are seeing her for diagnostic evaluation. We need to find it in an orthogonal projection before we do US so we can look in the correct location.
Our first step is to determine lesion depth (see Fig. 4-3 ). If the depth is such that the finding should be included on the other projection (see Fig. 4-3 , red, green, and most orange dots), then it is either due to superimposition of breast tissue or obscured on the other projection. If obscured, there are several techniques that we can use to determine the location in the orthogonal projection. If the lesion depth is far posterior (see Fig. 4-3 , yellow and some orange dots), then a different approach will be needed.
Obscured in the Other Projection
We have several views to help us. The “best guess” spot compression, true lateral, or stepped oblique views can help whether the finding is best seen in the CC or MLO view. If a lesion is seen well only in the CC projection, rolled CC views can be very helpful. For an MLO finding, a true lateral view is typically the most helpful.
“Best Guess” Spot Compression View
This is a good place to start for a one-view finding that may be obscured in the other projection. Go ahead and get your spot compression view in the projection that you are most worried about. Then make your best guess about where the finding may be located in the other projection. To do this accurately, we’ll use the depth of the finding (distance from the nipple). Then look at that depth on the other projection, which should be similar between views as long as the nipple is in profile ( Fig. 4-8 ). Sometimes there is more than one suspect and both may need to undergo spot compression.

Shallow or Stepped Oblique Views
In these techniques, full mammogram views are obtained at slightly different angles from the original CC or MLO view in which the finding is seen. Shallow oblique (or off-angle) views are obtained at plus and minus 10 to 15 degrees from the original angle. Stepped oblique views are similar in concept; full images are obtained at 10- to 15-degree intervals between the CC and MLO views. The finding can be tracked over the views to determine the location. We do not use these often because other techniques can usually determine the location with fewer exposures. In some cases, though, either shallow or stepped oblique views can localize a finding when our other tricks haven’t helped.
Rolled CC Views for a CC Finding
If a lesion is seen only on the CC view, the location in the superior or inferior breast must be determined. For rolled CC views, the breast is placed on the image receptor and the superior breast is rolled lateral (CCRL) or medial (CCRM). The inferior breast may also be rolled in the opposite direction during positioning. If a lesion moves laterally on the CCRL, then it is located in the superior breast ( Fig. 4-9 ). If it moves medially or does not shift in position, then it is in the inferior or central breast. These are similar in concept to shallow oblique views. Rolled CC views may also “unsuperimpose” normal structures and may be quite helpful in proving that a finding represents summation artifact rather than a true lesion.

ML View for an MLO Finding
We reviewed earlier how a lateral lesion shifts lower from the MLO to the ML view and a medial lesion shifts up (see Fig. 4-5 ). We can use this to our advantage for lesions seen only in the MLO view ( Fig. 4-10 ). An ML or LM view may also reveal a finding that was initially seen only on the CC view.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree