Chapter 12 The role of scalp pH
The availability of fetal scalp blood sampling for the assessment of fetal scalp capillary blood pH and its application in practice vary enormously. The NICE guidelines have suggested the use of scalp pH in situations with suspicious and/or pathological cardiotocography (CTG) after due consideration to the clinical situation.13 At times the clinical situation may demand early delivery rather than a scalp pH. In reality, junior doctors use scalp pH more when they have less experience of labour ward responsibilities. This is understandable as they have a greater anxiety with a less-developed degree of understanding. As they gain experience and use pH as a guide, they then understand better the associations of an abnormal and a normal pH and will need this reassurance less often. The process of scalp blood sampling is undignified and uncomfortable for the woman. This is not to say it should not be done if properly indicated.
When the fetal heart rate (FHR) is reactive and normal, the chance of fetal acidosis is extremely low.112–114 On the other hand, suspicious and abnormal FHR changes are not always associated with acidosis.113–116 Such observations form the basis of the perceived need to measure fetal scalp pH for further investigation.
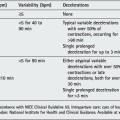
Changes in the CTG cause anxiety to the person not familiar with CTG interpretation. An inexperienced person in a centre with fetal blood sampling (FBS) facilities might perform FBS more frequently. When properly interpreted, assessment of FHR changes in most cases proves of equal value to pH in predicting fetal outcome.14 FBS is a useful adjunct because, even with the worst pattern of tachycardia, reduced baseline variability and decelerations, only 50–60% of the fetuses are acidotic.113 A wall chart correlating different FHR patterns to the percentage who are likely to be acidotic is available in most labour wards. It is clear from that chart and other studies that when the FHR pattern exhibited accelerations the chance of fetal acidosis was zero, emphasizing accelerations as the hallmark of fetal health.113 One problem of these charts is that all fetuses do not conveniently provide a fetal heart tracing that easily falls into one category. There is the added perspective of the need for a time continuum, which is so important in trace analysis.
Baseline variability is another good indicator of fetal health. When normal baseline variability is observed in the last 20 min prior to delivery, the babies are in good condition at birth regardless of other features of the trace.117 Fetal acidosis is more common when there is a loss of baseline variability with tachycardia or late decelerations.113, 118 The preservation of normal baseline variability indicates that the autonomic nervous system is responsive and the fetus is trying to compensate despite other abnormal features in the trace. The reason that, with a given FHR pattern, there are different percentages of fetuses showing acidosis depends on the duration for which the suspicious or abnormal FHR pattern was present before the time of FBS.15 The approximate duration after which acidosis develops in an appropriately grown term fetus with a given FHR pattern has been discussed previously. It is also known that, in fetuses with less ‘placental reserve’ such as those with intrauterine growth restriction (IUGR), thick scanty meconium-stained fluid,119 in the presence of bleeding and in post-term infants, the rate of decline of pH is steep compared with term infants appropriately grown with abundant, clear amniotic fluid.
RESPIRATORY AND METABOLIC ACIDOSIS
Assessing pH alone does not suffice to identify the fetus at risk, and more comprehensive blood gas analysis may be necessary for clinical management. The placenta is the respiratory organ of the fetus. Reduction of perfusion of the placenta from the fetal circulation is manifest as variable decelerations due to cord compression, and reduction of perfusion from the maternal circulation is manifest as late decelerations. During the early stage of such threats the transfer of carbon dioxide from the fetal to maternal side is reduced leading to its accumulation. This results in respiratory acidosis manifested by a low pH and a high PCO2. Respiratory acidosis is transitory particularly when corrective measures are taken and can be managed conservatively provided the FHR pattern improves. With a further reduction of perfusion from the maternal or fetal side the oxygen transfer becomes affected leading to anaerobic metabolism and metabolic acidosis in the fetus. This is manifested by a low pH, low PO2 and high base excess. Such metabolic acidosis is damaging to the tissues. Transitory low pH values of respiratory type are not uncommon in low-risk labours. Acidotic pH values in cord arterial blood in babies born with good Apgar scores are due to this phenomenon: 73% of babies with cord pH below 7.00 had a 1 min Apgar score of more than 7 and 86% had a 5 min Apgar score greater than 7.120 These findings are probably due to respiratory acidosis which does not correlate well with fetal or neonatal condition. In this situation a comprehensive blood gas analysis, including PCO2, base excess and preferably lactic acid, is desirable and more predictive. Caution should be exercised in using equipment that measures only pH. It is possible to determine the degree of metabolic acidosis by measuring the lactic acid level by the bedside with 5 μl of blood using the lactate card.121 Intrauterine infection with a high metabolic rate presents a greater oxygen demand to the fetus and metabolic acidosis might develop with minimal interruption of placental perfusion.
WHEN TO DO FETAL BLOOD SAMPLING
Gradually developing hypoxia
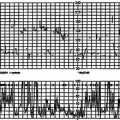
When the FHR shows hypoxic features suggestive of distress it is important to perform an FBS for pH and blood gases as the fetus may be, or become, acidotic. Initially this will be a respiratory, followed by metabolic, acidosis. Once the FHR shows a distress pattern (markedly reduced baseline variability with late or atypical variable decelerations), the time taken for metabolic acidosis to develop is unpredictable. This pattern is referred to as preterminal pattern by some authors. After a certain duration of the distress pattern (the distress period) the FHR starts to decline in a rapid stepwise pattern, culminating in terminal bradycardia and death (the distress-to-death period). The stress-to-distress interval (20.00 h–00.00 h, i.e. 4 h), the distress period (00.00 h–03.00 h, i.e. 3 h) and the distress-to-death period (03.00 h–03.40 h, i.e. 40 min) are illustrated by Figure 11.13A–J
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree