his chapter will focus on imaging of shoulder trauma, arthroplasty, arthrodesis, and miscellaneous shoulder procedures requiring use of orthopaedic fixation devices and prostheses.
his chapter will focus on imaging of shoulder trauma, arthroplasty, arthrodesis, and miscellaneous shoulder procedures requiring use of orthopaedic fixation devices and prostheses.
 Trauma
Trauma
Shoulder fractures and dislocations of the glenohumeral and acromioclavicular joints are common. Conservative management may be effective in certain situations. However, operative intervention is commonly required. Clinical presentations, classifications when appropriate, treatment options, and imaging of postoperative complications will be reviewed in each section.
Proximal Humeral Fractures
Proximal humeral fractures account for 5% of all fractures. These injuries occur most commonly in elderly osteoporotic patients and are typically associated with minor trauma, such as a fall. Morbidity is similar to hip fractures in this population. In younger patients, the mechanism of injury is more often high-velocity trauma (motor vehicle accidents, etc.).
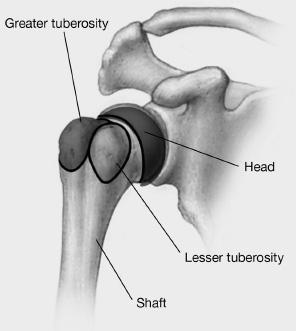
Multiple classifications have been used for proximal humeral fractures. Fracture lines tend to follow the physeal lines that divide the humerus into four parts: (a) the head, (b) the greater tuberosity, (c) the lesser tuberosity, and (d) the shaft (see Fig. 9-1). The Neer classification was proposed in 1970. This system includes the four segments of the humerus and addresses vascular isolation of the head and the degree of displacement. As defined by Neer, fragments are considered displaced if there is >1 cm of separation or >45 degrees of angulation of a fragment with respect to the others (see Fig. 9-2). Most fractures are undisplaced (80% to 85%) using the Neer classification.
Neer classification
One-part fracture: No fragments displaced (80%)
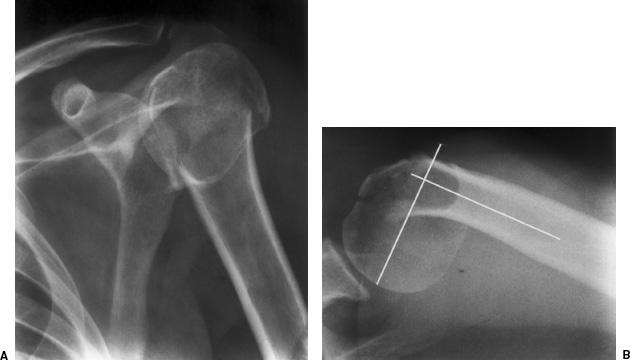
Two-part fracture: One fragment displaced (13%) (Fig. 9-2)
Three-part fracture: Displacement of the surgical neck and either the greater or lesser tuberosity (3%)
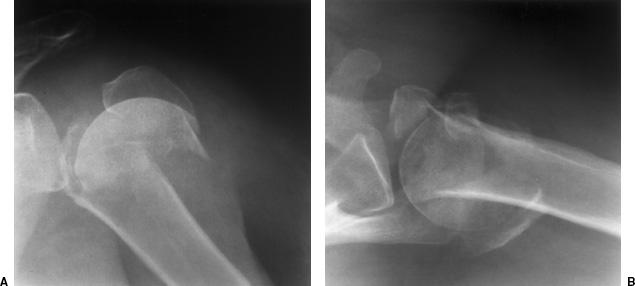
Four-part fracture: Displaced fractures of the greater tuberosities and surgical neck (4%) (see Fig. 9-3)
Other classifications include the AO (Arbeitgemeinshaft fur osteosynthesefragen) classification that includes three categories based on the vascular isolation of the articular (head) fragment and the likelihood of avascular necrosis. Type A has no vascular isolation and a low incidence of avascular necrosis (extracapsular with two to four fragments). Type B fractures have partial isolation of the articular fragment and type C fractures have an isolated articular fragment with a high incidence of avascular necrosis (Fig. 9-3). There are subcategories with all three types due to increasing complexity. The Orthopaedic Trauma Association classification is even more complex and includes the degree of displacement of each fragment, angulation, impaction, and associated dislocations (see Fig. 9-4). Imagers should become familiar with the system used by the surgeons with whom they interact. Agreement on which classification is best is difficult due to frequent interobserver disagreement. Some use three-dimensional reconstructions of computed tomographic (CT) images to classify proximal humeral fractures.
 Fig. 9-1 Illustration of the proximal humerus demonstrating the four segments involved in proximal fractures.
Fig. 9-1 Illustration of the proximal humerus demonstrating the four segments involved in proximal fractures.
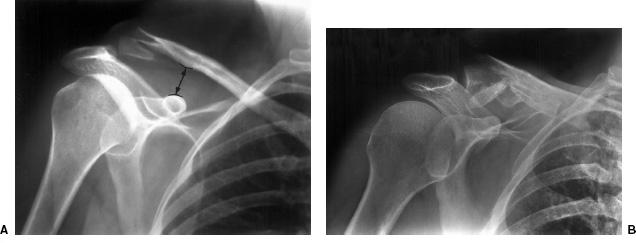
 Fig. 9-2 Two-part fracture. Anteroposterior (AP) (A) and axillary (B) radiographs demonstrate a fracture of the humeral neck and tuberosity. The head is angulated over 45 degrees making this a two-part fracture.
Fig. 9-2 Two-part fracture. Anteroposterior (AP) (A) and axillary (B) radiographs demonstrate a fracture of the humeral neck and tuberosity. The head is angulated over 45 degrees making this a two-part fracture.
 Fig. 9-3 Four-part fracture. Anteroposterior (AP) (A) and axillary (B) radiographs demonstrating displacement of >1 cm of all fragments (head, tuberosities, and shaft).
Fig. 9-3 Four-part fracture. Anteroposterior (AP) (A) and axillary (B) radiographs demonstrating displacement of >1 cm of all fragments (head, tuberosities, and shaft).
 Fig. 9-4 Orthopaedic Trauma Association B3.1. Axillary radiograph demonstrates a vertical cleft fracture with the greater tuberosity intact.
Fig. 9-4 Orthopaedic Trauma Association B3.1. Axillary radiograph demonstrates a vertical cleft fracture with the greater tuberosity intact.
SUGGESTED READING
Edelson G, Kelly I, Vigder F, et al. A three-dimensional classification for fractures of the proximal humerus. J Bone Joint Surg. 2004;86B:413–425.
Neer CS II. Displaced proximal humeral fractures: Classification and evaluation. J Bone Joint Surg. 1970;52A:1077–1089.
Orthopaedic Trauma Association Committee on Coding and Classification. J Orthop Trauma. 1996;10:1–155.
Preoperative Imaging
Imaging of patients with suspected proximal humeral fractures should include anteroposterior (AP), scapular Y, and axillary projections. The last may be difficult for some patients. Therefore, a transthoracic radiograph provides a lateral view and is excellent for evaluation of humeral head rotation (see Fig. 9-5). CT with coronal and sagittal reformatting or three-dimensional reconstruction is optimal for evaluating fragment displacement and angulation (see Fig. 9-6). Three-dimensional reconstructions may also improve the consistency for classification.
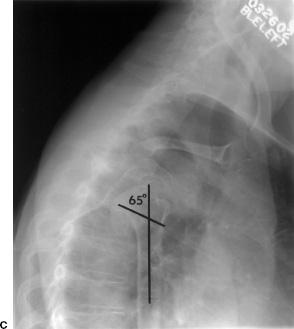
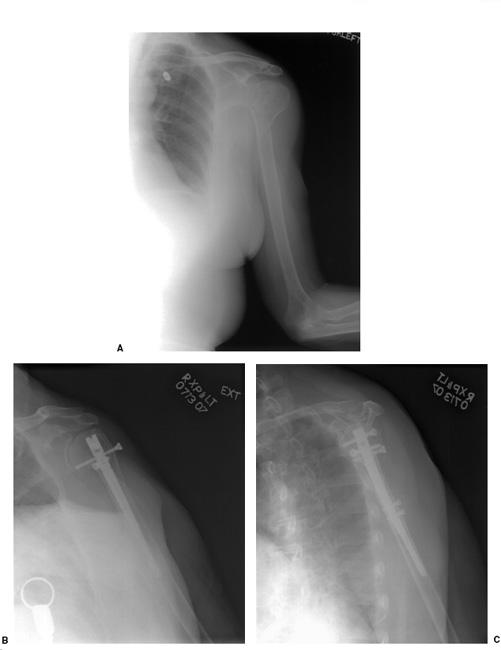
 Fig. 9-5 Radiographs of a proximal humeral fracture (three part). Anteroposterior (AP) (A), scapular Y or Neer view (B), and transthoracic (C) projection of a comminuted proximal humeral fracture with displacement of the head and tuberosity. The transthoracic view provides an image at 90 degrees to the AP view and demonstrates the position of the humeral head in relation to the shaft. There is 65 degrees of posterior rotation of the humeral head in addition to the displacement.
Fig. 9-5 Radiographs of a proximal humeral fracture (three part). Anteroposterior (AP) (A), scapular Y or Neer view (B), and transthoracic (C) projection of a comminuted proximal humeral fracture with displacement of the head and tuberosity. The transthoracic view provides an image at 90 degrees to the AP view and demonstrates the position of the humeral head in relation to the shaft. There is 65 degrees of posterior rotation of the humeral head in addition to the displacement.
SUGGESTED READING
Burstein AH, Adler LM, Blank JE, et al. Evaluation of the Neer system of classification of proximal humeral fractures with computerized tomography scans and plain radiographs. J Bone Joint Surg. 1996;78A:1371–1375.
Treatment Options
Treatment of proximal humeral fractures is based on the fracture classification, patient age, comorbidities, activity, and bone quality. Treatment options include closed reduction, open reduction and internal fixation, and arthroplasty. Hemiarthroplasty is usually performed unless there is significant glenoid articular disease.
One- and two-part fractures (Fig. 9-6) may be treated conservatively with closed reduction. Greater tuberosity fractures displaced 5 mm or more should be internally fixed to avoid loss of function and axillary nerve injury. Lesser tuberosity fractures tend to displace medially, but can usually be treated with closed reduction.
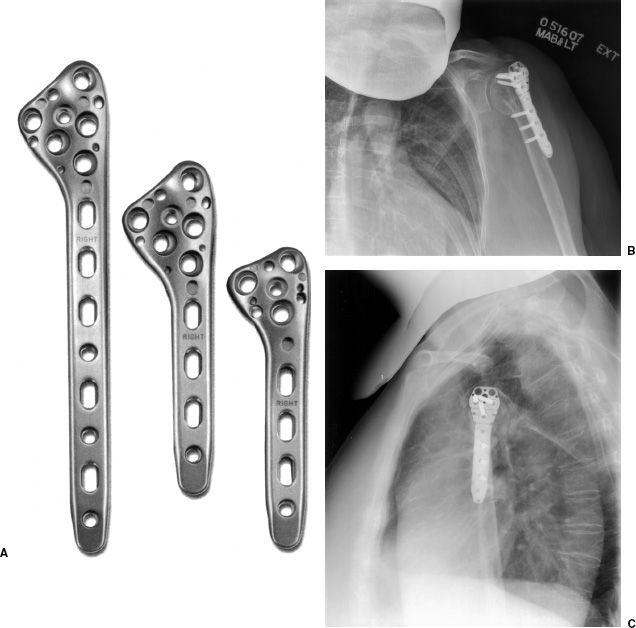
Three- and four-part fractures (Fig. 9-5) are more complex. In elderly patients with significant comorbidities, fractures may be treated with closed reduction. Significant loss of motion is common. Valgus-impacted head fragments are at less risk for avascular necrosis so results may be satisfactory with closed reduction. Open reduction may be accomplished with plate and screw fixation (see Fig. 9-7), intramedullary nails (see Fig. 9-8), or tension band constructs (see Fig. 9-9). Hemiarthroplasty is also an option. This approach is commonly performed on elderly patients with osteoporotic bone because internal fixation is more complex in this setting (see Fig. 9-10).
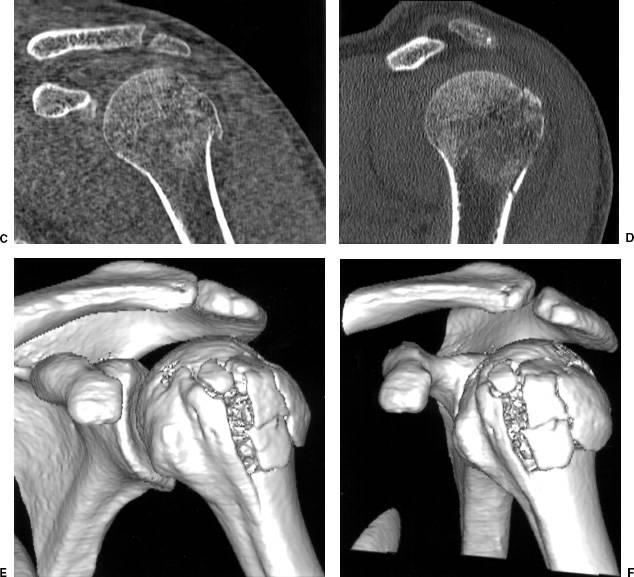
 Fig. 9-6 Radiographic and computed tomographic (CT) images of a one-part fracture. Radiograph (A) and axial (B), coronal (C), sagittal (D), and three-dimensional (E and F) reformatted images demonstrating a minimally displaced comminuted fracture involving the greater tuberosity with sparing of the biceps groove.
Fig. 9-6 Radiographic and computed tomographic (CT) images of a one-part fracture. Radiograph (A) and axial (B), coronal (C), sagittal (D), and three-dimensional (E and F) reformatted images demonstrating a minimally displaced comminuted fracture involving the greater tuberosity with sparing of the biceps groove.
SUGGESTED READING
Jacob RP, Miniaci A, Anson PS, et al. Four-part valgus impacted fractures of the proximal humerus. J Bone Joint Surg. 1991;73B:295–298.
Naranja RJ, Iannoti JP. Displaced three and four-part proximal humeral fractures: Evaluation and management. J Am Acad Orthop Surg. 2000;8:373–382.
Neer CS II. Displaced proximal humeral fractures: Part II. Treatment of three and four-part displacement. J Bone Joint Surg. 1970;52A:1090–1103.
Imaging of Postoperative Complications
Complications following repair of proximal humeral fractures may be related to the initial injury or surgical approaches. Proximal humeral fractures are associated with neurovascular injuries in 21% to 36% of cases. The axillary nerve is most frequently injured and this may result in permanent motor dysfunction. Nerve injury is most common following anterior fracture dislocations. Most vascular injuries (84%) occur in elderly patients and more than half are associated with brachial plexus injuries. Diagnosis may be accomplished clinically (loss of sensation over the lateral deltoid with axillary nerve injury) or magnetic resonance imaging (MRI). Vascular injuries can be clarified with angiography because magnetic resonance (MR) angiography can be difficult following acute trauma. The rotator cuff and biceps are typically involved. Interposition of the biceps tendon between tuberosity fragments will prevent healing. Rotator cuff disruptions and tendon interposition can be evaluated with CT, MRI, or conventional arthrograms (see Fig. 9-11).
 Fig. 9-7 Internal fixation with locking plate and screws. A: Proximal humeral locking plates. (Courtesy of Acumed, Hillsboro, Oregon.) Anteroposterior (AP) (B) and transthoracic (C) views following plate and screw fixation of a three-part fracture.
Fig. 9-7 Internal fixation with locking plate and screws. A: Proximal humeral locking plates. (Courtesy of Acumed, Hillsboro, Oregon.) Anteroposterior (AP) (B) and transthoracic (C) views following plate and screw fixation of a three-part fracture.
 Fig. 9-8 Intramedullary nail fixation. A: Radiograph demonstrating a two-part proximal humeral fracture with undisplaced tuberosity fragments. Anteroposterior (AP) (B) and scapular Y (C) views following intramedullary nail and screw fixation of the proximal fragments with distal locking screws.
Fig. 9-8 Intramedullary nail fixation. A: Radiograph demonstrating a two-part proximal humeral fracture with undisplaced tuberosity fragments. Anteroposterior (AP) (B) and scapular Y (C) views following intramedullary nail and screw fixation of the proximal fragments with distal locking screws.
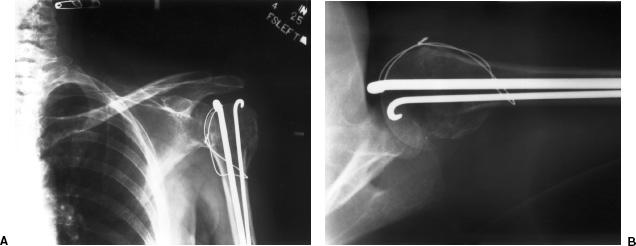
 Fig. 9-9 Comminuted minimally displaced proximal humeral fracture. Anteroposterior (AP) (A) and axillary (B) radiographs demonstrate internal fixation with Rush rods and tension band wire. The Rush rods extend into the subacromial space, which may result in impingement.
Fig. 9-9 Comminuted minimally displaced proximal humeral fracture. Anteroposterior (AP) (A) and axillary (B) radiographs demonstrate internal fixation with Rush rods and tension band wire. The Rush rods extend into the subacromial space, which may result in impingement.
Arthrosis and loss of range of motion occur with both closed and open treatment approaches (see Fig. 9-12). Adhesive capsulitis is also fairly common following proximal humeral fractures. This may be difficult to detect unless conventional arthrography is performed and the actual capsular volume measured. Mild to moderate (5 to 10 mL) capsulitis may respond to distention arthrography.
Avascular necrosis occurs in up to 14% of three-part fractures treated with closed reduction and the incidence is higher with four-part fractures. Imaging may be hindered with internal fixation devices. However, aggressive approaches in treatment approaches for three- and four-part fractures (internal fixation or hemiarthroplasty) reduce the need to image patients following treatment. Patients treated with closed reduction or minimal internal fixation hardware can be evaluated with MRI.
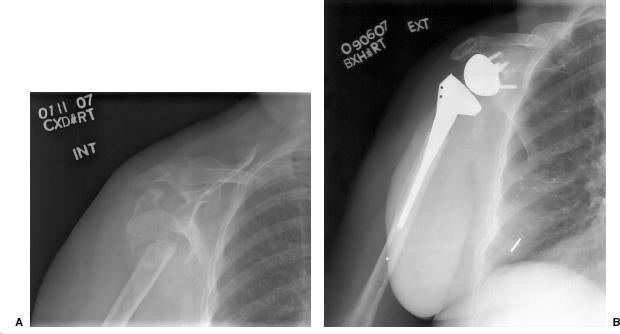
Implant failure, malunion, and nonunion may be evident on serial radiographs (see Fig. 9-13). Evaluation of nonunion is most easily accomplished with CT with reformatting in the coronal and sagittal planes in the presence of orthopaedic hardware. In patients treated with closed reduction, MRI may also be helpful. The fracture margins will have low signal intensity with high signal intensity between the fragments on T2-weighted sequences.
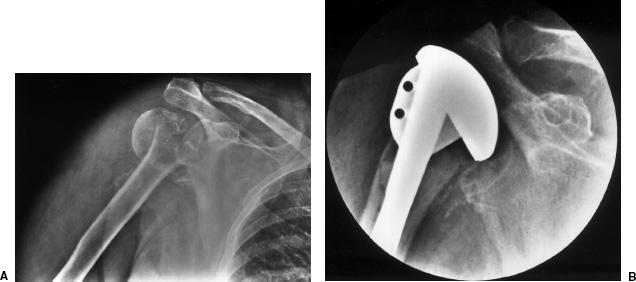
 Fig. 9-10 Anteroposterior (AP) radiograph (A) demonstrating a four-part fracture in an elderly woman. B: Operative image following hemiarthroplasty.
Fig. 9-10 Anteroposterior (AP) radiograph (A) demonstrating a four-part fracture in an elderly woman. B: Operative image following hemiarthroplasty.
 Fig. 9-11 Conventional arthrogram demonstrating entrapment of the biceps tendon (arrows) between the tuberosity fragments.
Fig. 9-11 Conventional arthrogram demonstrating entrapment of the biceps tendon (arrows) between the tuberosity fragments.
Clavicle Fractures
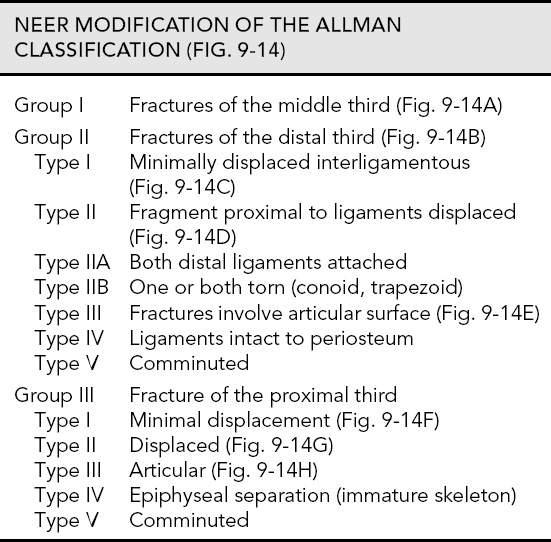
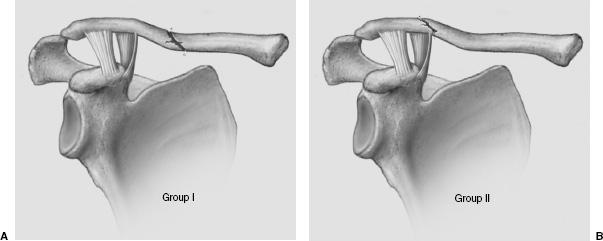
Clavicle fractures are common in neonates, children, and adults. Clavicle fractures account for 5% to 10% of adult fractures and 35% to 45% of shoulder-related fractures. The mechanism of injury may be direct trauma (fall on the shoulder) or a fall on the outstretched hand. Allman divided clavicular fractures by location into group I—middle third, group II—distal, and group III–—proximal. Most fractures (72% to 80%) involve the mid clavicle, whereas 20% to 30% of fractures involve the distal clavicle. Proximal or medial clavicular fractures are uncommon (2% to 5%). The Neer modification further subdivides groups II and III based on ligament and articular involvement and the degree of comminution. The Orthopaedic Trauma Association classification is more complex and is based on location, fracture line orientation, comminution, and articular involvement. The Allman classification with the Neer modification is commonly used (see Fig. 9-14).
 Fig. 9-12 Old three-part fracture treated with closed reduction in an 85-year old woman. There is complete loss of joint space with reduced humeroacromial space and no motion in the glenohumeral joint.
Fig. 9-12 Old three-part fracture treated with closed reduction in an 85-year old woman. There is complete loss of joint space with reduced humeroacromial space and no motion in the glenohumeral joint.
 Fig. 9-13 Nonunion. A: Radiograph demonstrating nonunion of a four-part fracture. B: The patient was treated with a reverse shoulder arthroplasty.
Fig. 9-13 Nonunion. A: Radiograph demonstrating nonunion of a four-part fracture. B: The patient was treated with a reverse shoulder arthroplasty.
SUGGESTED READING
Allman FL Jr. Fractures and ligamentous injuries of the clavicle and its articulations. J Bone Joint Surg. 1967;49A:774–784.
Neer CS II. Fractures of the distal third of the clavicle. Clin Orthop. 1968;58:43–50.
Webber MC, Haines JF. The treatment of lateral clavicle fractures. Injury 2000;31:175–179.
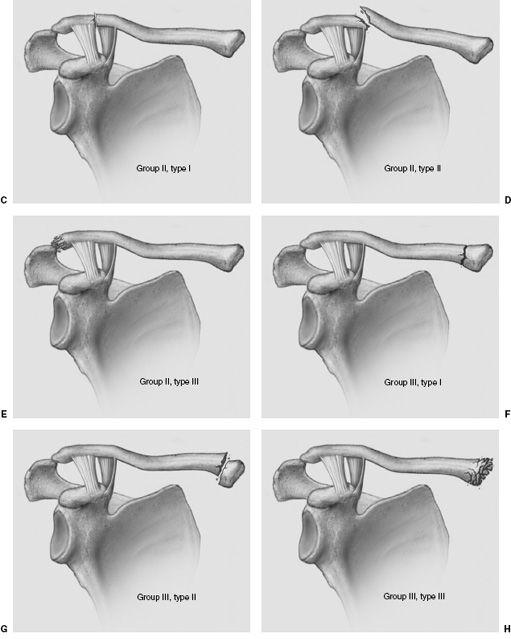
Pretreatment Imaging
Imaging of patients with suspected clavicular injuries should include AP and angled AP (15 degrees normally or 40 degrees cephalad for subtle injuries) projections to include the entire clavicle and acromioclavicular and sternoclavicular articulations (see Fig. 9-15). The mid and distal aspects of the clavicle are easily evaluated on these views. The medial clavicle and its articulation are more difficult to visualize due to bony overlap. Although there are several techniques that can be used to better visualize the medial clavicle, CT is most often performed to better define this region (see Fig. 9-16).
Stress views can be performed on patients with suspected ligament injury and acromioclavicular separation. However, this approach is usually reserved for stable injuries to avoid further displacement of the clavicle fracture.
SUGGESTED READING
Cofield RH, Berquist TH. The shoulder. In: Berquist TH. Imaging of orthopaedic trauma, 2nd ed. New York: Raven Press; 1992:579–657.
 Fig. 9-14 Neer modification of the Allman clavicle fracture classification. A: Group I—fractures of the middle third of the clavicle. B: Group II—fractures of the distal third of the clavicle. C: Group II, type I—fracture of the distal clavicle between the ligaments. D: Group II, type II—fracture of the distal clavicle proximal to the ligaments with elevated medial fragment. E: Group II, type III—comminuted fracture of the distal articular surface. F: Group III, type I—minimally displaced fracture of the medial clavicle. G: Group III, type II—displaced fracture of the medial clavicle with elevation of the distal fragment. H: Group III, type III—comminuted medial articular fracture.
Fig. 9-14 Neer modification of the Allman clavicle fracture classification. A: Group I—fractures of the middle third of the clavicle. B: Group II—fractures of the distal third of the clavicle. C: Group II, type I—fracture of the distal clavicle between the ligaments. D: Group II, type II—fracture of the distal clavicle proximal to the ligaments with elevated medial fragment. E: Group II, type III—comminuted fracture of the distal articular surface. F: Group III, type I—minimally displaced fracture of the medial clavicle. G: Group III, type II—displaced fracture of the medial clavicle with elevation of the distal fragment. H: Group III, type III—comminuted medial articular fracture.
 Fig. 9-15 Minimally displaced fracture of the mid clavicle (group I). The anteroposterior (AP) (A) radiograph does not clearly demonstrate the fracture. The fracture is clearly identified (arrow) on the angled (15 degrees cephalad) view (B).
Fig. 9-15 Minimally displaced fracture of the mid clavicle (group I). The anteroposterior (AP) (A) radiograph does not clearly demonstrate the fracture. The fracture is clearly identified (arrow) on the angled (15 degrees cephalad) view (B).
Treatment Options
Conservative treatment is most often employed for treatment of clavicle fractures, specifically medial and mid-clavicle fractures. A sling or figure-of-eight brace is typically used for approximately 6 weeks with early shoulder, elbow, and hand range of motion exercises when tolerated by the patient.
Operative intervention is considered for cosmetic deformity, shortening of mid clavicle fractures >2 cm, and distal fractures. The incidence of nonunion is highest with shortening and displaced distal clavicular fractures (see Fig. 9-17). Treatment of distal third fractures has been controversial. Group II type II fractures are at the level of the coracoclavicular ligaments. Type IIA fractures are proximal to the ligaments and the ligaments remain intact. Type IIB injuries have significant displacement of the fracture fragments due to the loss of downward restraint of the coracoclavicular ligaments (see Fig. 9-18). Excellent surgical results have been reported with intramedullary pin or wire fixation and ligament repair. Plate and screw fixation is also an option (see Figs. 9-19 and 9-20).
 Fig. 9-16 Axial computed tomographic (CT) image demonstrating a medial fracture dislocation (arrow) (group III, type III).
Fig. 9-16 Axial computed tomographic (CT) image demonstrating a medial fracture dislocation (arrow) (group III, type III).
SUGGESTED READING
Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicle fractures. A multicenter, randomized clinical trial. J Bone Joint Surg. 2007;89A:1–10.
Chen CH, Chen WJ, Shih CH. Surgical treatment of distal clavicle fracture with coracoclavicular ligament disruption. J Trauma. 2002;52:72–78.
Neer CS II. Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma. 1963; 3:99–110.
Imaging of Complications
Complications may be related to the type of injury or treatment. In the past, the incidence of malunion and nonunion was considered to be insignificant. However, in recent years nonunion in displaced midshaft fractures has been reported to be 15% with unsatisfactory patient outcomes in up to 32% of cases. Distal third fractures are less frequent compared to midshaft fractures, but they account for half of nonunions. Imaging of nonunion can be accomplished with serial radiographs (Fig. 9-19). However, if callus and healing potential need to be better defined it is best to evaluate the fracture with CT with reformatted images in the appropriate image planes. The incidence of nonunion in displaced midshaft and distal clavicle fractures can be reduced significantly (2.2%) with operative intervention. Surgical treatment is not without complications. Migration of wires and pins has been described. Hardware removal for pain and irritation may also be necessary in up to 8% of patients. Other complications related to operative intervention include wound infection (4.8%) and transient brachial plexus neuropathy (13%). Other reported complications regardless of treatment include complex regional pain syndrome and thoracic outlet syndrome. The latter may require conventional or MR angiography for diagnosis. Instability or residual symptoms in the acromioclavicular joint can be evaluated with stress views once the fracture is considered healed clinically.
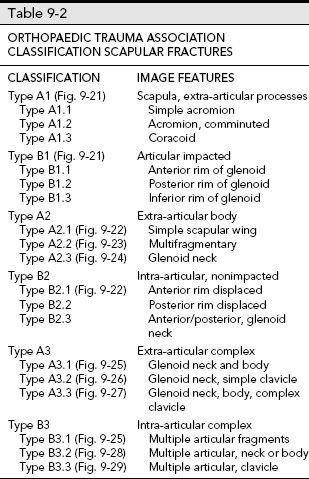
 Fig. 9-17 A: Group I mid clavicle fracture with >2 cm of shortening and nonunion. B: Radio-graph following reduction with an intramedullary pin.
Fig. 9-17 A: Group I mid clavicle fracture with >2 cm of shortening and nonunion. B: Radio-graph following reduction with an intramedullary pin.
 Fig. 9-18 A: Group II, type IIB fracture of the distal clavicle with upward displacement and increase in the coracoclavicular space (curved lines, double arrow) due to associated rupture of both the conoid and trapezoid ligaments. B: Comminuted fracture at the level of the ligaments with avulsed fragments inferiorly and elevation of the major medial fragment (group II, type V).
Fig. 9-18 A: Group II, type IIB fracture of the distal clavicle with upward displacement and increase in the coracoclavicular space (curved lines, double arrow) due to associated rupture of both the conoid and trapezoid ligaments. B: Comminuted fracture at the level of the ligaments with avulsed fragments inferiorly and elevation of the major medial fragment (group II, type V).
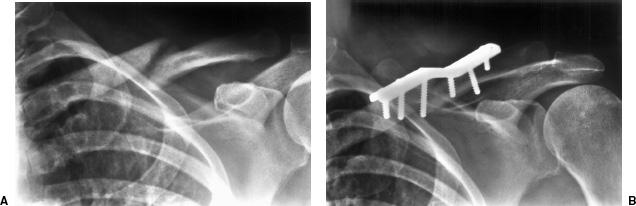
 Fig. 9-19 A: Nonunion of a mid clavicle fracture treated with plate and screw fixation (B).
Fig. 9-19 A: Nonunion of a mid clavicle fracture treated with plate and screw fixation (B).
 Fig. 9-20 Anteroposterior (AP) (A) andangled AP (B) radiographs following locking plate and screw fixation of a mid clavicle fracture. There are also several interfragmentary screws.
Fig. 9-20 Anteroposterior (AP) (A) andangled AP (B) radiographs following locking plate and screw fixation of a mid clavicle fracture. There are also several interfragmentary screws.
SUGGESTED READING
Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicle fractures. A multicenter, randomized clinical trial. J Bone Joint Surg. 2007;89A:1–10.
Connolly JF, Dehne R. Nonunion of the clavicle and thoracic outlet syndrome. J Trauma. 1989;29:1127–1132.
Scapular Fractures
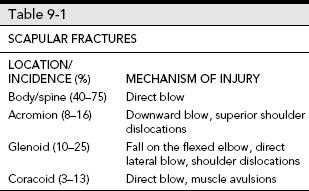
Scapular fractures are uncommon, accounting for only 1% of all fractures and 3% to 5% of all shoulder injuries. There is a high incidence of associated injuries due to the high velocity mechanism of injury required for complex scapular fractures. Scapular neck and body fractures are most common (see Table 9-1).
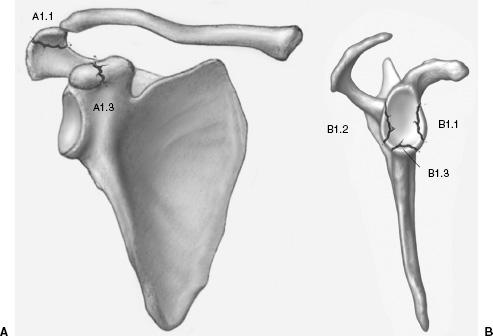
Multiple classification systems have been applied to scapular fractures. Anatomic description is important and most systems are designed to specify complexity and articular involvement. The Orthopaedic Trauma Association classification separates fractures into extra-articular, articular, and complex (see Table 9-2 and Figs. 9-21 to 9-29).
 Fig. 9-21 Orthopaedic Trauma Association extra-articular processes. A: Illustration of simple fractures of the acromion (type A1.1) and coracoid (type A1.3) and (B) impacted articular fractures of the glenoid anterior rim (B1.1), posterior rim (B1.2), and inferior glenoid (B1.3).
Fig. 9-21 Orthopaedic Trauma Association extra-articular processes. A: Illustration of simple fractures of the acromion (type A1.1) and coracoid (type A1.3) and (B) impacted articular fractures of the glenoid anterior rim (B1.1), posterior rim (B1.2), and inferior glenoid (B1.3).
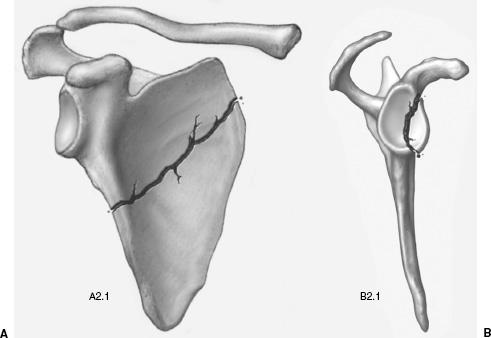
 Fig. 9-22 Orthopaedic Trauma Association scapular fractures. A: Illustrations of simple scapular wing (type A2.1) and (B) displaced anterior glenoid fracture (type B2.1).
Fig. 9-22 Orthopaedic Trauma Association scapular fractures. A: Illustrations of simple scapular wing (type A2.1) and (B) displaced anterior glenoid fracture (type B2.1).
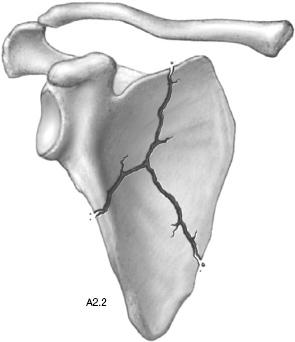
 Fig. 9-23 Orthopaedic Trauma Association complex extra-articular. Illustration of a type A2.2 fracture of the scapular body.
Fig. 9-23 Orthopaedic Trauma Association complex extra-articular. Illustration of a type A2.2 fracture of the scapular body.
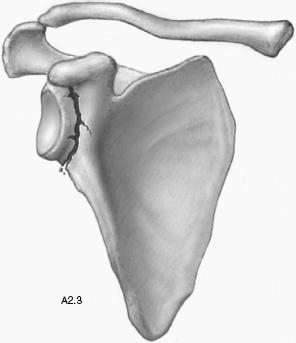
 Fig. 9-24 Orthopaedic Trauma Association extra-articular glenoid neck. Illustration of a glenoid neck fracture type A2.3.
Fig. 9-24 Orthopaedic Trauma Association extra-articular glenoid neck. Illustration of a glenoid neck fracture type A2.3.
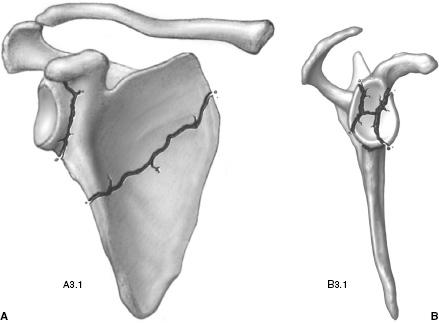
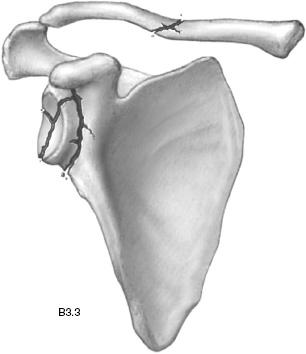
 Fig. 9-25 Orthopaedic Trauma Association extra-articular complex and intra-articular complex. A: Illustration of glenoid neck and body fractures (type A3.1) and (B) complex articular fracture (type B3.1).
Fig. 9-25 Orthopaedic Trauma Association extra-articular complex and intra-articular complex. A: Illustration of glenoid neck and body fractures (type A3.1) and (B) complex articular fracture (type B3.1).
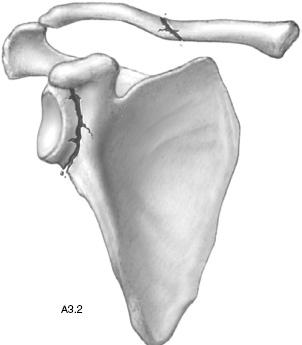
 Fig. 9-26 Orthopaedic Trauma Association glenoid neck and simple clavicle. Illustration of a glenoid neck and associated simple clavicle fracture (type A3.2).
Fig. 9-26 Orthopaedic Trauma Association glenoid neck and simple clavicle. Illustration of a glenoid neck and associated simple clavicle fracture (type A3.2).
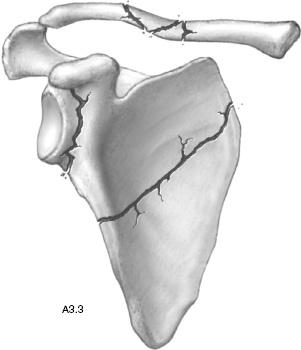
 Fig. 9-27 Orthopaedic Trauma Association glenoid neck, body, and complex clavicle. Illustration of a glenoid neck, body, and complex clavicle fracture (type A3.3).
Fig. 9-27 Orthopaedic Trauma Association glenoid neck, body, and complex clavicle. Illustration of a glenoid neck, body, and complex clavicle fracture (type A3.3).
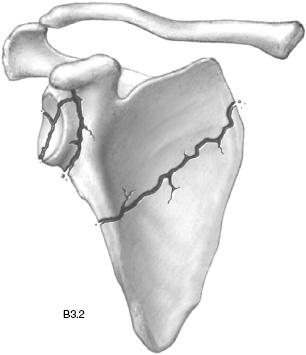
 Fig. 9-28 Orthopaedic Trauma Association complex articular, glenoid neck, and body. Illustration of complex articular, glenoid neck, and body fractures (type B3.2).
Fig. 9-28 Orthopaedic Trauma Association complex articular, glenoid neck, and body. Illustration of complex articular, glenoid neck, and body fractures (type B3.2).
 Fig. 9-29 Orthopaedic Trauma Association complex articular and clavicle. Illustration of a complex articular fracture with associated clavicle fracture (type B3.3).
Fig. 9-29 Orthopaedic Trauma Association complex articular and clavicle. Illustration of a complex articular fracture with associated clavicle fracture (type B3.3).
 Fig. 9-30 Axillary view demonstrating an undisplaced coracoid fracture (arrows).
Fig. 9-30 Axillary view demonstrating an undisplaced coracoid fracture (arrows).
SUGGESTED READING
Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg. 1984;66B: 725–731.
Orthopaedic Trauma Association Committee on coding and classification. J Orthop Trauma. 1996;10:1–155.
Pretreatment Imaging
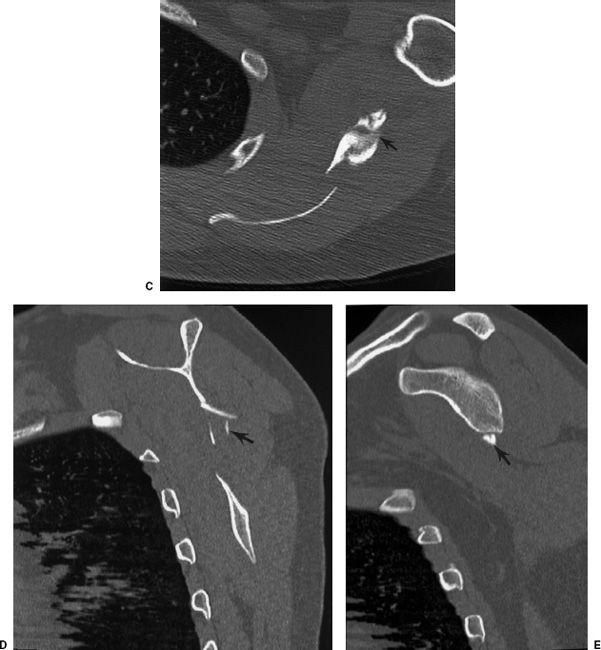
AP, lateral or scapular Y and axillary views should be obtained. The latter two projections may provide the only clear images of the coracoid and acromion (see Fig. 9-30). The most difficult problem is defining the complexity of the injury to the body and neck of the scapula and, more importantly, the articular involvement. This is difficult to assess on radiographs. When there is a question about the extent of injury, CT with reformatting or three-dimensional reconstruction should be obtained (see Fig. 9-31).
SUGGESTED READING
Cofield RH, Berquist TH. The shoulder. In: Berquist TH. Imaging of orthopaedic trauma, 2nd ed. New York: Raven Press; 1992:579–657.
 Fig. 9-31 Scapular fractures. A: Anteroposterior (AP) radiograph demonstrating a fracture that appears to involve the glenoid articular surface (arrows). B: Impacted glenoid neck fracture with a superiorly displaced body fragment (arrow). No obvious articular involvement. Computed tomography (CT) images in the axial (C) and sagittal (D and E) planes demonstrating a complex body fracture (arrows) with a small inferior glenoid fragment (arrow in E).
Fig. 9-31 Scapular fractures. A: Anteroposterior (AP) radiograph demonstrating a fracture that appears to involve the glenoid articular surface (arrows). B: Impacted glenoid neck fracture with a superiorly displaced body fragment (arrow). No obvious articular involvement. Computed tomography (CT) images in the axial (C) and sagittal (D and E) planes demonstrating a complex body fracture (arrows) with a small inferior glenoid fragment (arrow in E).
Treatment Options
Most scapular fractures can be treated with closed reduction. This is due to the extensive muscle support about the scapula that reduces displacement. Most fractures treated with closed reduction (90%) heal within 6 to 8 weeks. Shoulder motion should be initiated as soon as possible.
Glenoid articular fractures can be internally fixed with screws, K-wires, or reconstruction plates and screws. Similar fixation devices can be used for glenoid neck, scapular spine, and coracoid fractures.
SUGGESTED READING
Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg. 1984;66B: 725–731.
Kavanagh BF, Bradway JK, Cofield RH. Open reduction and internal fixation of displaced intraarticular fractures of the glenoid fossa. J Bone Joint Surg. 1993;75A:479–484.
Imaging of Complications
Complications directly related to the injury or treatment include neurovascular injury, infection, malunion, and nonunion. If not properly reduced, glenoid articular fractures can result in recurrent dislocations and instability. Instability can be diagnosed clinically. Imaging evaluation is best accomplished with MR arthrography. Capsulitis and arthrosis may also occur. Distention arthrography may be useful for releasing adhesions in patients with capsulitis.
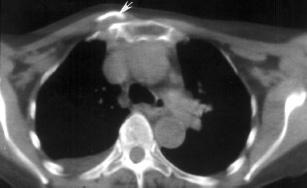
The most significant complications are not related to the scapula. Patients frequently have complications of the upper extremity, shoulder, lung, and chest wall. Pulmonary contusions and hemothorax occur in 15% to 55% of patients. Cerebral contusions occur in up to 40% and neural deficits in 5%. Splenic laceration is not uncommon resulting in splenectomy in 8% of patients. Most of these complications can be effectively classified with CT or MRI.
SUGGESTED READING
Goss TP. Fractures of the glenoid cavity. J Bone Joint Surg. 1992;74A:299–305.
Goss TP. Scapular fractures and dislocations: Diagnosis and treatment. J Am Acad Orthop Surg. 1996;52:106–115.
Dislocations
Glenohumeral dislocations are the most common and account for 50% of all dislocations. Dislocations may also occur in the acromioclavicular joint and account for 12% of all dislocations. Sternoclavicular joint dislocations are uncommon, accounting for only 3% of all shoulder dislocations.
 Fig. 9-32 Anterior dislocation. Anteroposterior (AP) (A) and scapular Y (B) radiographs demonstrating the typical subcoracoid position of the humeral head. On the scapular Y image (B), the humeral head should be over the glenoid at the junction of the Y formed by the scapular wing, coracoid, and spine and acromion (lines). In this case, it is obviously anteriorly dislocated. C, coracoid.
Fig. 9-32 Anterior dislocation. Anteroposterior (AP) (A) and scapular Y (B) radiographs demonstrating the typical subcoracoid position of the humeral head. On the scapular Y image (B), the humeral head should be over the glenoid at the junction of the Y formed by the scapular wing, coracoid, and spine and acromion (lines). In this case, it is obviously anteriorly dislocated. C, coracoid.
Glenohumeral Dislocations
Glenohumeral dislocations are almost always anterior (96% to 98%), with posterior dislocations accounting for 2% to 4% dislocations; inferior and superior dislocations are rare. Most anterior dislocations are due to a fall with the arm abducted and externally rotated. As the humeral head is displaced anteriorly, injury to the subscapularis, anterior capsule, and glenohumeral ligaments occurs to varying degrees. There are three glenohumeral ligaments (superior, middle, and inferior) which, along with the capsule and labrum, provide anterior stability. With anterior dislocations, the inferior glenohumeral ligament, which is the primary stabilizer, is injured along with the labral complex. This results in the Bankart lesion which may also include an osseous fragment. This lesion is evident in 50% of patients. A posterolateral impaction in the humeral head (Hill-Sach lesion) occurs in 67% to 76% of patients. Greater tuberosity fractures occur in 15% of patients. When this occurs, the biceps tendon may become trapped between the humeral head and tuberosity fragment.
Posterior dislocations occur from falls with the arm internally rotated and adducted, with electroconvulsive therapy, and following direct anterior trauma. The posterior capsule, glenoid rim, and anteromedial humeral head (reverse Hill-Sachs) may also be involved. Seventy-five percent of injuries will have a reverse Hill-Sachs lesion and up to 25% of patients have associated lesser tuberosity fractures.
SUGGESTED READING
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree