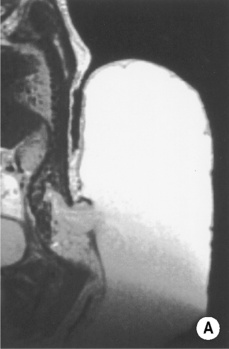
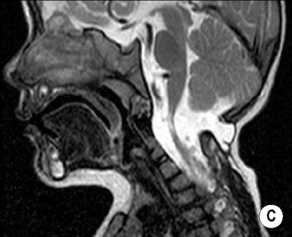
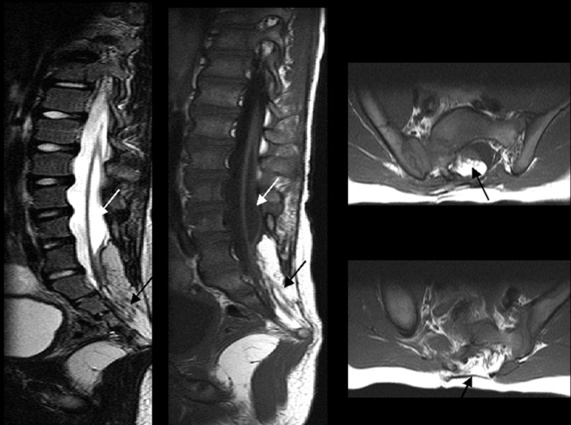
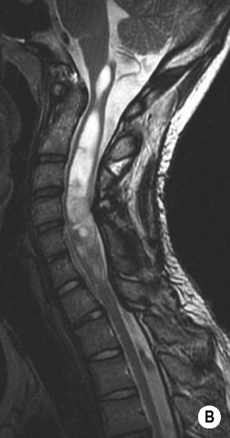
• This is also known as a neural tube defect (NTD), and comprises a group of congenital spine abnormalities that may cause progressive neurological damage (affecting 1:1000 live births) • The common feature is an anomaly of the midline structures of the back • It results from incomplete midline closure of the bony and neural spinal tissues following defective primary neural tube closure and persistence of the neural placode • This is due to a failure of fusion of the posterior spinal bony elements • Without a tethered cord: this is commonest at L5 or S1 • With a tethered cord: neurological defects are uncommon • Associations: meningocele • The nervous tissue is exposed and neurological defects are common • Most are myelomeningoceles and are virtually always associated with a Chiari II malformation • Usually the neural placode protrudes beyond the skin level with an expanded CSF-containing sac lined by meninges • Nerve roots (from the everted ventral placode) cross the widely dilated meningocele subarachnoid spaces to enter the neural exit foraminae • It is surgically repaired soon after birth, as untreated and exposed neural tissue is prone to ulceration and infection • Herniation of the spinal meninges through the intervertebral foramina or a vertebral body defect • Generalized or focal dural ectasia may also be seen in: neurofibromatosis • Anterior thoracic meningocele with ventral herniation of the spinal cord: this is most easily recognized with a midsagittal MRI of the thoracic spine where the spinal cord is displaced anteriorly and is in contact with a vertebral body near an intervertebral disc (commonly T6) • Lateral thoracic meningocele: this commonly presents as a paravertebral mass (CXR) • Posterior meningocele: herniation of the CSF sac (which is lined by dura and arachnoid) through a spinal defect results in a clinically apparent mass covered by skin • Anterior sacral meningocele: these are typically presacral and appear as a unilocular, complex lobular or multilocular cystic mass (the mass contains CSF which communicates with the intraspinal subarachnoid space) • Terminal myelocystocele: the central canal is dilated by a large hydromyelic cavity herniating into a posterior meningocele (through a posterior spinal bony defect) • Myelomeningocele: herniation of the spinal meninges and spinal neural tissue through a vertebral canal defect • Myelocele: the neural placode is flush with the skin surface but there is no skin covering • A low-lying conus medullaris tethered by a short thick filum terminale • The spinal cord reaches the adult position by term – the majority lie between T11/12 and L1/2 (it is abnormal if it is seen at or below the level of L3) • A mass of adipose tissue located mainly between the posterior spinal cord columns (a tongue-like extension along the central canal can often be seen) • Its usual location near the thoracocervical or craniovertebral junctions • This results from incomplete separation of the notochord from the endoderm, or from herniation of the endoderm into the dorsal ectoderm • A persistent connection between the endoderm and ectoderm resulting in splitting or deviation of the notochord (a cleft of the vertebral column associated with GI and CNS anomalies) • This forms part of the ‘split notochord’ syndrome: the spinal cord is split into two (usually unequal) hemicords • They are usually found within the thoracolumbar cord, extending over several vertebral segments • A longitudinal CSF-filled cavity that is lined mainly by glial tissue • An epithelial-lined skin opening with a variable fistulous extension to the dural surface A thin linear strip of tissue hypointense to the adjacent fat • Dermal openings at the sacrococcygeal level: these are directed inferiorly below the thecal sac (sacrococcygeal pits) • Dermal openings above the intergluteal cleft: these pass superiorly and may form a fistulous connection with the dural sac • This follows the abnormal development of the caudal cell mass as a result of apoptosis of notochordal cells which have not formed at the correct craniocaudal position • Absence of the vertebral column at the affected level (as well as a truncated spinal cord, an imperforate anus and genital anomalies) • A loculated CSF fluid collection:
The spine
SPINAL DYSRAPHISM
SPINAL DYSRAPHISM
DEFINITION
 it is also associated with anomalous development of the caudal cell mass
it is also associated with anomalous development of the caudal cell mass
Spina bifida occulta
 the defect is covered by skin
the defect is covered by skin
 it affects 20% of the general population with no neurological problems (± back pain)
it affects 20% of the general population with no neurological problems (± back pain)
 a cutaneous lesion such as a dimple, sinus, hairy naevus or haemangioma may be a marker of an underlying defect and is seen in 50% of cases
a cutaneous lesion such as a dimple, sinus, hairy naevus or haemangioma may be a marker of an underlying defect and is seen in 50% of cases
 lipomyelomeningodysplasia
lipomyelomeningodysplasia  diastematomyelia
diastematomyelia  neurenteric cyst
neurenteric cyst  dermoid and epidermoid cysts
dermoid and epidermoid cysts  dorsal dermal sinus
dorsal dermal sinus  caudal agenesis
caudal agenesis  myelocystocele
myelocystocele  spinal or filum terminale lipoma
spinal or filum terminale lipoma
Spina bifida aperta
 they are usually found within the lumbosacral region
they are usually found within the lumbosacral region
 occasionally it is a myelocele where the placode is flush with the surface and no meningocele component is present
occasionally it is a myelocele where the placode is flush with the surface and no meningocele component is present
 the posterior elements of the vertebral column and the other mesenchymal derivatives (e.g. paravertebral muscles) remain everted
the posterior elements of the vertebral column and the other mesenchymal derivatives (e.g. paravertebral muscles) remain everted
MENINGOCELES
DEFINITION
 varying degrees of dural ectasia usually accompany spinal dysraphisms
varying degrees of dural ectasia usually accompany spinal dysraphisms
 Ehlers–Danlos and Marfan’s syndromes
Ehlers–Danlos and Marfan’s syndromes  erosive arthropathies (e.g. ankylosing spondylitis)
erosive arthropathies (e.g. ankylosing spondylitis)
Types of meningocele
 it is usually solitary and located on the right
it is usually solitary and located on the right  there is an angular kyphoscoliosis towards the side of the meningocele with pressure erosion of the relevant intervertebral foraminal margins
there is an angular kyphoscoliosis towards the side of the meningocele with pressure erosion of the relevant intervertebral foraminal margins
 it occurs mainly within the lumbosacral region
it occurs mainly within the lumbosacral region
 there is usually a large eccentric anterior lower sacral defect (with a pathognomonic scimitar appearance on XR) and an expanded sacral canal
there is usually a large eccentric anterior lower sacral defect (with a pathognomonic scimitar appearance on XR) and an expanded sacral canal  there can be varying degrees of sacral or coccygeal agenesis
there can be varying degrees of sacral or coccygeal agenesis
 it is rare, and associated with syndromes such as VACTERL
it is rare, and associated with syndromes such as VACTERL
CONGENITAL SPINAL ANOMALIES
TETHERED CORD SYNDROME
DEFINITION
 it is commonly a component of other spinal malformations (e.g. a spinal lipoma)
it is commonly a component of other spinal malformations (e.g. a spinal lipoma)
SPINAL LIPOMA
DEFINITION
Intramedullary/intradural lipomas
 the overlying dura mater is usually intact and the lipoma entirely intradural – however there may be a dural defect to which the cord and lipoma become adherent
the overlying dura mater is usually intact and the lipoma entirely intradural – however there may be a dural defect to which the cord and lipoma become adherent
NEURENTERIC CYST
DEFINITION
 the cyst attachment to the notochord can prevent vertebral body fusion (leading to spinal anomalies)
the cyst attachment to the notochord can prevent vertebral body fusion (leading to spinal anomalies)  it forms part of the ‘split notochord’ syndrome
it forms part of the ‘split notochord’ syndrome
‘Split notochord’ syndrome
 Dorsal enteric fistula: the most severe form, representing a fistula connecting the intestinal cavity with the midline dorsal skin surface (therefore travelling through soft tissues and spine)
Dorsal enteric fistula: the most severe form, representing a fistula connecting the intestinal cavity with the midline dorsal skin surface (therefore travelling through soft tissues and spine)
 Dorsal enteric (dermal) sinus: this is a remnant of the posterior portion of the fistula with a blind-ending tube opening onto the skin surface
Dorsal enteric (dermal) sinus: this is a remnant of the posterior portion of the fistula with a blind-ending tube opening onto the skin surface
 Dorsal enteric cyst (neurenteric cyst): this is a trapped remnant of the middle portion of the fistula and is found within the intraspinal or paraspinal compartments
Dorsal enteric cyst (neurenteric cyst): this is a trapped remnant of the middle portion of the fistula and is found within the intraspinal or paraspinal compartments
 Dorsal enteric diverticulum: this is a remnant of the anterior portion of the fistula with a tubular diverticulum originating from the dorsal bowel mesentery
Dorsal enteric diverticulum: this is a remnant of the anterior portion of the fistula with a tubular diverticulum originating from the dorsal bowel mesentery
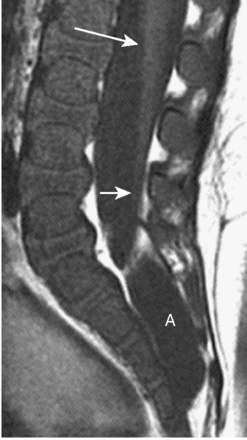
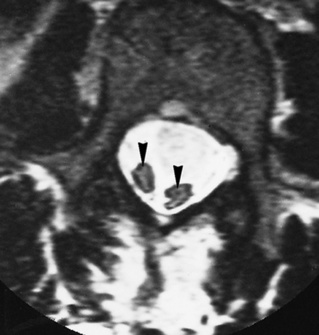
DIASTEMATOMYELIA
DEFINITION
 each hemicord has a central canal and an anterior spinal artery but only gives off the ipsilateral spinal roots from one anterior and one posterior grey matter horn
each hemicord has a central canal and an anterior spinal artery but only gives off the ipsilateral spinal roots from one anterior and one posterior grey matter horn  the hemicords nearly always reunite caudally
the hemicords nearly always reunite caudally
SYRINGOMYELIA
DEFINITION
 it usually involves many segments (or the whole cord)
it usually involves many segments (or the whole cord)  it follows either cord damage (and subsequent cavitation) or CSF that has been abnormally driven into the cord (via the perivascular spaces)
it follows either cord damage (and subsequent cavitation) or CSF that has been abnormally driven into the cord (via the perivascular spaces)  as a result of hydrodynamic forces the lesion is capable of propagating into normal cord tissue
as a result of hydrodynamic forces the lesion is capable of propagating into normal cord tissue
DORSAL DERMAL SINUS
DEFINITION
 it typically affects the lumbosacral region
it typically affects the lumbosacral region  it is often associated with cutaneous stigmata (e.g. a hairy naevus or capillary haemangioma)
it is often associated with cutaneous stigmata (e.g. a hairy naevus or capillary haemangioma)
RADIOLOGICAL FEATURES
MRI
 they do not require further imaging
they do not require further imaging
 these warrant further investigation
these warrant further investigation
CAUDAL AGENESIS
DEFINITION
Caudal agenesis
 Type I: there is a high (often T12) abrupt spinal cord termination
Type I: there is a high (often T12) abrupt spinal cord termination  there is a characteristic wedge-shaped configuration with variable coccygeal to lower thoracic vertebral aplasia
there is a characteristic wedge-shaped configuration with variable coccygeal to lower thoracic vertebral aplasia
 Type II: the true notochord is not affected and only the caudal cell mass is involved
Type II: the true notochord is not affected and only the caudal cell mass is involved  the vertebral aplasia is less extensive (with up to S4 present as the last vertebra)
the vertebral aplasia is less extensive (with up to S4 present as the last vertebra)
 OEIS: omphalocele / exstrophy / imperforate anus / spinal defects
OEIS: omphalocele / exstrophy / imperforate anus / spinal defects
 VACTERL: vertebral anomalies / anal atresia / cardiovascular anomalies / tracheo-oesophageal fistula / oesophageal atresia / renal or radial abnormalities / limb anomalies
VACTERL: vertebral anomalies / anal atresia / cardiovascular anomalies / tracheo-oesophageal fistula / oesophageal atresia / renal or radial abnormalities / limb anomalies
 Currarino triad: partial sacral agenesis + an anorectal malformation + a presacral mass (either a teratoma or anterior meningocele)
Currarino triad: partial sacral agenesis + an anorectal malformation + a presacral mass (either a teratoma or anterior meningocele)
INTRASPINAL ARACHNOID CYST
DEFINITION
 Extradural: these arise from defects within the dura mater (congenital or inflammatory)
Extradural: these arise from defects within the dura mater (congenital or inflammatory)
 Intradural: these arise from arachnoidal duplications or spinal arachnoiditis
Intradural: these arise from arachnoidal duplications or spinal arachnoiditis
 Tarlov cyst: a perineural arachnoid cyst occurring commonly within the sacrum (especially on the 2nd sacral root)
Tarlov cyst: a perineural arachnoid cyst occurring commonly within the sacrum (especially on the 2nd sacral root)  it is of doubtful clinical significance
it is of doubtful clinical significance
The spine










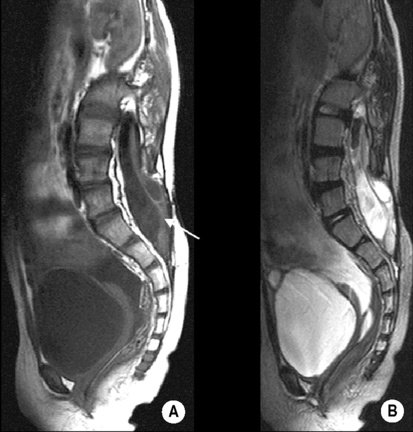
 an enlarged thecal sac
an enlarged thecal sac  a thickened (> 1.5mm) filum terminale
a thickened (> 1.5mm) filum terminale it is considered a normal variant in the absence of a clinical tethered cord syndrome (and is seen in up to 5% of the normal population)
it is considered a normal variant in the absence of a clinical tethered cord syndrome (and is seen in up to 5% of the normal population) the spinal cord terminates at or below the level of L3 (in 80% of cases), and is usually tethered to the dorsal dura where it fuses with the lipoma
the spinal cord terminates at or below the level of L3 (in 80% of cases), and is usually tethered to the dorsal dura where it fuses with the lipoma they occur within the cervical or lower thoracic regions and can compress the spinal cord (usually the anterior aspect)
they occur within the cervical or lower thoracic regions and can compress the spinal cord (usually the anterior aspect) there are varying degrees of laminar dysplasia and fusion
there are varying degrees of laminar dysplasia and fusion they are are usually located within the thoracolumbar region
they are are usually located within the thoracolumbar region  a bony or cartilaginous midline extradural spur may arise from the malformed lamina which often lies between each hemicord
a bony or cartilaginous midline extradural spur may arise from the malformed lamina which often lies between each hemicord a tethered cord (75% of cases)
a tethered cord (75% of cases)


 scoliosis
scoliosis a well-circumscribed CSF cavity often demonstrating prominent transverse ridges within its wall (giving a beaded or loculated appearance)
a well-circumscribed CSF cavity often demonstrating prominent transverse ridges within its wall (giving a beaded or loculated appearance)  pulsatile cysts can show flow-related signal changes
pulsatile cysts can show flow-related signal changes it can be congenital or acquired (e.g. following a lumbar puncture)
it can be congenital or acquired (e.g. following a lumbar puncture) in 20% a dorsal dermal sinus can be traced to a skin dimple on the lower back (this is a possible source of intradural sepsis)
in 20% a dorsal dermal sinus can be traced to a skin dimple on the lower back (this is a possible source of intradural sepsis) lower limb deformities
lower limb deformities the spine and spinal cord may appear severed (the most severe cases) or focally hypoplastic (less severe cases)
the spine and spinal cord may appear severed (the most severe cases) or focally hypoplastic (less severe cases) they can be multiple and are rarely associated with myelomalacia or syringomyelia
they can be multiple and are rarely associated with myelomalacia or syringomyelia  extradural lesions can be overdiagnosed within the thoracic region (the thoracic spine is commonly wide and partly loculated)
extradural lesions can be overdiagnosed within the thoracic region (the thoracic spine is commonly wide and partly loculated)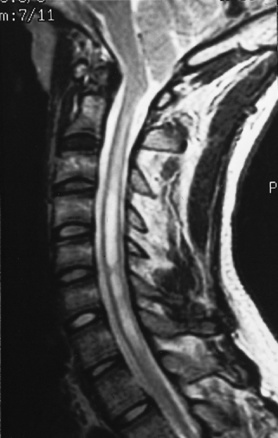








 bullet-shaped vertebral bodies
bullet-shaped vertebral bodies  short pedicles
short pedicles  posterior vertebral body scalloping
posterior vertebral body scalloping  lumbar hyperlordosis
lumbar hyperlordosis  a ‘champagne glass’ pelvis
a ‘champagne glass’ pelvis  squared pelvic iliac wings
squared pelvic iliac wings upper spinal cord compression (due to ligamentous thickening)
upper spinal cord compression (due to ligamentous thickening)  dens hypoplasia
dens hypoplasia  posterior vertebral body scalloping
posterior vertebral body scalloping dens hypoplasia
dens hypoplasia  posterior vertebral body scalloping
posterior vertebral body scalloping





