Chapter 1 Theoretical Considerations
Introduction
Ophthalmic ultrasonography is the main diagnostic imaging modality of the eye. It is a safe, non-invasive diagnostic tool providing instant feedback for the evaluation of a variety of ophthalmic disorders. Diagnostic ophthalmic ultrasonography is most useful in the presence of opaque ocular media due to corneal opacities, anterior chamber opacities, cataracts, vitreous hemorrhage or inflammatory opacities. Ophthalmic ultrasonography is also valuable in the presence of clear media, for evaluation of the iris, lens, ciliary body and orbital structures. Intraocular tumors are routinely documented, measured, and differentiated by ultrasonographic techniques (Chapter 11). This chapter provides a brief overview of the basic physics of ultrasound, instrumentation, and special examination techniques used in ophthalmic ultrasonography.
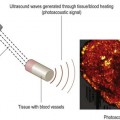
Basic physics
Laws of acoustic energy
The use of ultrasound in medicine is dependent on the physical laws of acoustic energy: reflection, refraction, and absorption.1 The angle of incidence is an important factor in the strength of the returning echoes. To accurately access structures based on the intensity of the returning echoes, the sound beam needs to be directed perpendicular to the desired structure. Sound beams directed at an oblique angle towards an interface result in the reflection of some of the sound beams away from the probe causing a weaker signal. Variations in the shape and size of the acoustic interface can also result in scattering of some of the sound beams. Ultrasound directed at a coarse, irregular surface results in significant loss of echo strength due to diversion of reflected echoes.
Frequency and resolution
Frequencies currently used in ophthalmic ultrasound machines range from 8–80 MHz, compared with 2–6 MHz typically used in other fields of diagnostic ultrasound. The use of higher frequencies allows for increased resolution, which is essential in the evaluation of small ophthalmic structures. The superficial location of the eye and the low absorptive properties of its primarily aqueous based structures, make the use of high frequencies practical.2 The high frequencies are achieved with mechanical scanning by single-element focused transducers. Electronically scanned arrays are not usually found in ophthalmic imaging devices because it is difficult to assemble array elements with the necessary half-wavelength spacing.3 The unique anatomy of the ocular structures allows the sound beam in ophthalmic devices to reach all areas of the eye in a close to optimal perpendicular orientation by movement of the eye and positioning of the transducer.
Instrumentation
In 1956 Mundt and Hughes published the first report of in vivo A-scan ultrasonography of intraocular tumors.4 Other clinical applications were published soon after.5 Techniques for B-scan ophthalmic examination and ultrasonographic features of specific ocular diseases and tumors were described within 2 years of the initial publication.6 Since then, many investigators have aided in the design and improvement of ophthalmic ultrasound instrumentation as well as expanded upon the diagnostic techniques. The most frequently utilized ophthalmic ultrasound instrumentation includes A-scan, B-scan (Chapters 2 and 3), and ultrasound biomicroscopy (Chapters 4 and 6). Color Doppler ultrasonography (Chapter 5) and 3-D ultrasonography (Chapter 19) has limited ophthalmic applications.
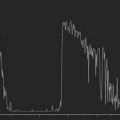
A-scan
A-scan is a one-dimensional display of echo strength over time. Vertical spikes correspond to echo intensity and are shown on the horizontal axis as a function of time. There are two primary types of A-scan used in ophthalmic ultrasonography; biometric A-scan and standardized diagnostic A-scan.7 Each has slightly different operating frequencies and amplification algorithms.
Biometric A-scan
Biometric A-scan is optimized for axial eye length measurements (Chapter 7). It utilizes a probe with an operating frequency of 10–12 MHz and a linear amplification curve.8 The sound velocity in ocular structures along the visual axis at physiological temperatures are well established resulting in highly accurate measurements.9–11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree