CHAPTER 94 Thoracic Aortic Trauma
THORACIC AORTIC TRAUMA
Etiology and Pathophysiology
Blunt aortic trauma is caused by a severe deceleration injury. The aortic arch is relatively fixed to the thoracic inlet by the brachiocephalic vessels, whereas the ascending and descending aorta are relatively mobile. During deceleration, horizontal shear forces act unequally on the relatively fixed arch and mobile ascending and descending aorta, causing extreme stress on the points of attachment of the aorta, namely, the aortic root and aortic isthmus, rendering these sites susceptible to transection (Fig. 94-1).1 In addition, rapid deceleration may cause the vertebral column, sternum, first rib, and clavicle to compress the aorta in the region of the isthmus, contributing to the mechanism of injury.2
In clinical practice, the aortic isthmus is by far the most common site of aortic injury; the aortic root and ascending aorta represent 5% or less of cases (Fig. 94-2). However, in autopsy series, the ascending aorta is involved in 25% of cases.3 This discrepancy is explained by the fact that many patients with ascending aortic injury do not survive to reach the hospital or are not stable enough for imaging because of grave complications of ascending aortic trauma, such as hemopericardium with tamponade, disruption of the aortic valve, and coronary artery dissection.
The degree of traumatic aortic injury depends on the nature of disruption of the aortic wall. Potential aortic injuries range from intimal hemorrhage, through intimal laceration and medial laceration, to complete laceration of the aorta.1 Disruption of the intima and media results in a pseudoaneurysm. Complete laceration, with disruption of the adventitia, usually results in immediate death.
Manifestations of Disease
Imaging Techniques and Findings
Radiography
Plain film findings associated with aortic trauma include a widened mediastinal contour, obscuration of the aortic arch or descending aortic margin, displacement of the trachea or of a nasogastric tube (if present) to the right, and left apical cap (Fig. 94-3). Fracture of the first or second ribs may be seen as a result of the causative trauma.4 However, each of these findings has been shown to have poor sensitivity or poor specificity. For example, in the trauma setting, a widened mediastinum is more commonly explained by anteroposterior positioning, lung contusion, hemothorax, and venous mediastinal bleeding, decreasing the specificity of these findings. Furthermore, in the majority of aortic injuries, the adventitia remains intact, resulting in only mild radiographic mediastinal findings, decreasing the sensitivity of plain radiography. In one study of aortic trauma, 44% of patients with subsequently proven aortic injury had a normal chest radiograph.5 Therefore, plain radiography is not sufficiently sensitive or specific for the evaluation of aortic injury, and in the correct clinical setting, the patient should proceed directly to other modes of imaging.
Computed Tomography
Multidetector computed tomography (MDCT) is the definitive modality for diagnosis of aortic trauma because of its speed, accuracy, postprocessing advantages, and ability to simultaneously evaluate the whole body for traumatic injury. CT angiography has been shown to have 100% sensitivity and 100% negative predictive value for traumatic aortic injury, at lower cost and with fewer complications than by catheter angiography.6
Aortic Pseudoaneurysm
Most patients with aortic trauma who survive to imaging will have a partial tear of the aortic wall. If the intima and media are torn but the adventitia remains intact, blood is forced between the layers, causing formation of a pseudoaneurysm. The imaging appearance is of a rounded bulge projecting from the aorta (Fig. 94-4). The margins are typically irregular, and there is often an intimal flap that forms a “collar” at the neck of the pseudoaneurysm. Note that the injury to the intima may extend several centimeters proximal or distal to the visualized pseudoaneurysm. The extent of the injury, especially the proximal extent, is crucial in the planning of repair because branch vessel involvement has a major influence on repair technique.

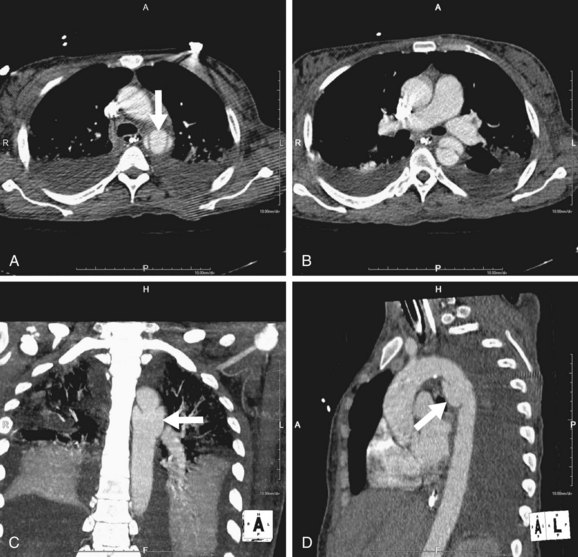
 FIGURE 94-1
FIGURE 94-1
 FIGURE 94-2
FIGURE 94-2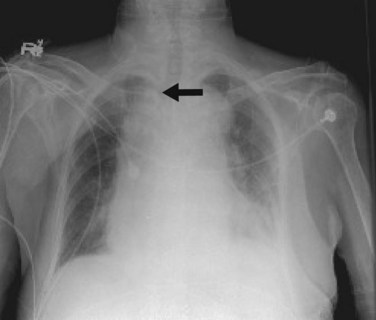
 FIGURE 94-3
FIGURE 94-3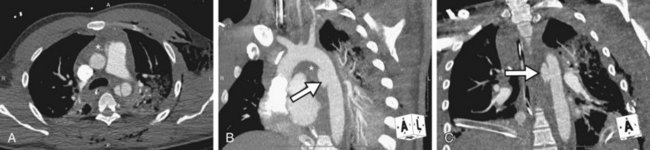
 FIGURE 94-4
FIGURE 94-4

