Tracheobronchomalacia
Melissa L. Rosado-de-Christenson, MD, FACR
Key Facts
Terminology
Excessive collapsibility of airway lumen
Tracheomalacia = affects trachea
Tracheobronchomalacia = affects trachea and bronchi
Imaging Findings
Chest radiographs may be normal because they are obtained at end-inspiration
CT findings
Inspiratory imaging may be normal
Coronal tracheal diameter exceeds sagittal diameter
Expiratory airway collapse to < 50% of expected luminal area
Crescent or lunate tracheal morphology
Expiratory collapse of central bronchi in cases of tracheobronchomalacia
Exclusion of external compression/mass effect
Top Differential Diagnoses
Saber-Sheath Trachea
Acquired Tracheal Stenosis
Wegener Granulomatosis
Relapsing Polychondritis
Pathology
Lack of integrity of tracheobronchial cartilages
Decreased longitudinal fibers of pars membranacea
Clinical Issues
Patients may be asymptomatic; incidental diagnosis
Cough, dyspnea, hemoptysis
Diagnostic Checklist
CT is imaging study of choice
Dynamic airway CT during expiration, forced expiration, or coughing
TERMINOLOGY
Definitions
Malacia = softness
Generally used to characterize cartilage or bone
Pars membranacea = membranous portion of posterior trachea devoid of cartilage
Tracheomalacia = tracheal weakness and propensity for luminal collapse
Decrease or atrophy of longitudinal elastic fibers of pars membranacea &/or impairment of cartilage integrity
Accentuation of physiologic changes in airway lumen with exaggerated changes in tracheal diameter
Normal trachea: Dilates with inspiration and narrows with expiration based on pressure differences
Tracheal narrowing most prominent with
Forced expiration
Cough
Valsalva maneuver
Tracheobronchomalacia = involvement of trachea and main stem bronchi
Bronchomalacia = isolated collapsibility of central bronchi without tracheal involvement
Classification
Primary or congenital
Secondary or acquired
IMAGING FINDINGS
General Features
Best diagnostic clue
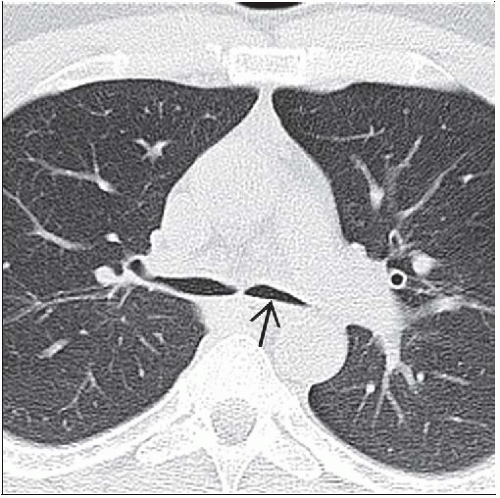
Airway narrowing to < 50% of expected luminal area
Typically accentuated by expiration
Patient position/location
Typically affects intrathoracic trachea
Extrathoracic or cervical tracheomalacia is less common
May be localized or may affect entire trachea
Size: > 50% decrease in airway luminal diameter
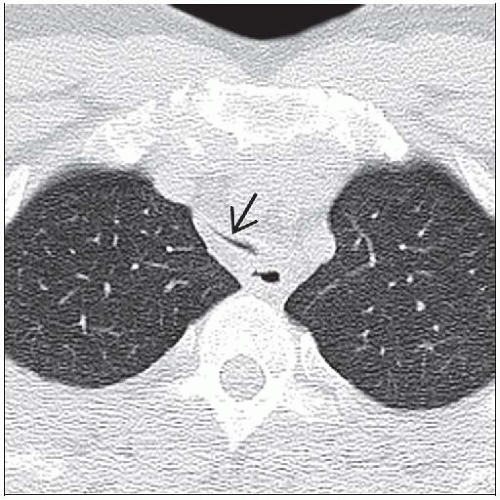
Morphology: Crescent-shaped with anterior ballooning of pars membranacea into airway lumen
CT Findings
Trachea may appear normal on inspiratory CT
Airway wall thickness normal
May be incidental diagnosis on CT
Coronal tracheal diameter may exceed sagittal diameter ⇒ “lunate” tracheal morphology
Expiratory reduction of tracheal cross-sectional area
Lower threshold criterion for diagnosis than with dynamic expiratory imaging
Change between inspiration and expiration > 18% in upper trachea > 28% in mid trachea
Leads to probability of tracheomalacia (90-100%)
Change in cross-sectional area less than above values → probability that patient does not have tracheomalacia is 95-100%
Dynamic CT imaging
High sensitivity and good agreement with bronchoscopically visible collapsibility
Imaging during coughing; most sensitive method for eliciting tracheal collapse
Criterion of > 50% collapse during coughing
Affected patients may show greater degrees of collapse ranging from 70-100%
Virtual bronchoscopy
Paired end inspiratory and dynamic expiratory virtual bronchoscopy
May obviate conventional bronchoscopy in patients with contraindications to procedure
Evaluation of adjacent structures for exclusion of external compression
Mediastinal masses
Goiter
Bronchogenic and other foregut cysts
Children with vascular anomalies
Double aortic arch, vascular ring
Anomalous left pulmonary artery; pulmonary artery sling
Airway obstruction may persist after surgical repair of vascular anomaly in up to 30% of cases
Associated abnormalities
Air-trapping
Children
Cardiovascular abnormalities: Patent ductus arteriosus, atrial or ventricular septal defects
Bronchopulmonary dysplasia
Gastroesophageal reflux
Chest wall anomalies, scoliosis, pectus excavatum
MR Findings
Evaluation of extrinsic airway abnormalities
Advantages
No ionizing radiation
Multiple assessments with various respiratory maneuvers
Radiographic Findings
Radiographs may be completely normal, as they are typically obtained in full inspiration
Radiography; low sensitivity of 60%
Imaging Recommendations
Best imaging tool: CT is study of choice for imaging airways
Protocol advice
Inspiratory and expiratory imaging
Imaging at end inspiration and end expiration
Dynamic CT
Imaging at full inspiration
Imaging during forced expiration or coughing
Dynamic CT
Preoperative airway evaluation in infants with vascular rings
Imaging after application and withholding of positive ventilatory pressure in infants to simulate inspiratory and expiratory imaging
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree