Cryptogenic Organizing Pneumonia
Jud W. Gurney, MD, FACR
Key Facts
Terminology
Clinicopathological entity characterized by polypoid plugs of loose granulation tissue within air spaces
Imaging Findings
Multiple alveolar opacities (90%)
Either subpleural or peribronchial, oval or trapezoid in shape
May be migratory and wax and wane
Air-bronchograms (often dilated) common
Perilobular pattern
Consolidation outlines periphery of secondary pulmonary lobule
Reverse halo sign
Central ground-glass opacity surrounded by denser crescentic (semicircular to circular) consolidation at least 2 mm in thickness
Solitary alveolar opacity (10%) mimics bronchogenic carcinoma
Top Differential Diagnoses
Chronic Eosinophilic Pneumonia
Bronchioloalveolar Cell Carcinoma
Sarcoidosis, Alveolar
Pathology
Polypoid granulations tissue in bronchiolar lumen (Masson bodies) and alveolar ducts associated with variable interstitial and airspace infiltration by mononuclear cells and foamy macrophages
Clinical Issues
Subacute symptoms over weeks
Treatment corticosteroids, relapses (despite treatment) in over 50%
TERMINOLOGY
Abbreviations and Synonyms
Cryptogenic organizing pneumonia (COP), secondary organizing pneumonia (SOP), proliferative bronchiolitis, idiopathic bronchiolitis obliterans organizing pneumonia (BOOP)
Definitions
Clinicopathological entity characterized by polypoid plugs of loose granulation tissue within air spaces
IMAGING FINDINGS
General Features
Best diagnostic clue: Bilateral, peripheral, basal, nodular consolidation
Patient position/location: Typically in mid and lower zones
Size: Tiny nodules to whole lobes
CT Findings
Multiple patterns
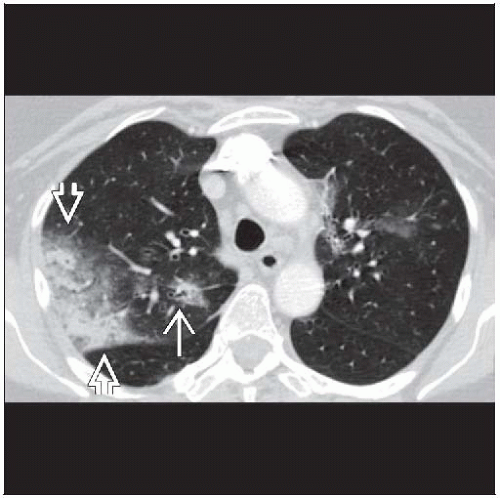
Multiple alveolar opacities (90%)
Size of consolidation from few cm in size to whole lobe
Often admixed with ground-glass opacities
Air-bronchograms common, often dilated
Bilateral, lower zones
Lung volumes preserved
Axial plane: Subpleural or bronchovascular (75%)
May be migratory and wax and wane over weeks to months
More common in immunocompetent compared to immunocompromised patients
Presence of consolidation associated with greater likelihood of partial or complete response to treatment
Multiple pulmonary nodules (10%)
< 5 mm diameter (40%), > 5 mm diameter (60%)
May have air-bronchograms
No zonal predominance
Solitary alveolar opacity (10%)
Mimics bronchogenic carcinoma
< 3 cm (60%) or > 3 cm diameter (40%)
Median diameter 1.9 cm
More common upper lung zones (60%) vs. lower lung zones (40%)
Subpleural (40%), peripheral bronchovascular (33%), or peripheral (30%)
Round (30%); flat, oval, or trapezoidal (70%)
Pleural tag (50%)
Irregular margin (spiculated) (95%)
Satellite nodules (55%)
Vessels converge at edge of lesion (80%)
May be cavitary
Reticular interstitial pattern (< 10%)
Overlaps with idiopathic pulmonary fibrosis or nonspecific interstitial pneumonia
Signifies fibrosis
Associated findings in patients with multiple alveolar opacities
Band-like opacities, 2 patterns
Linear opacities paralleling bronchial course toward pleura
Subpleural lines, unrelated to bronchi
Pleural effusions less common (10%), when present small
Mediastinal adenopathy (20%)
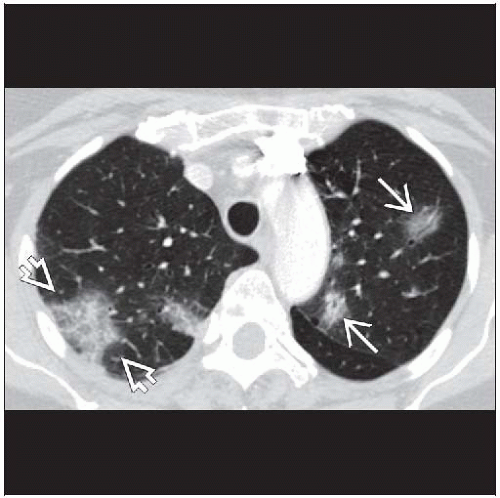
Perilobular pattern
Consolidation outlines periphery of secondary pulmonary lobule
May form arcades and polygonal opacities that extend to pleural surface like fish scales or tiles on a roof (imbricate)
Perilobular consolidation not as sharply defined as thickened interlobular septa in pulmonary edema
More predominant in mid and lower lung zones
Seen in 50% but not specific for COP
Reverse halo sign
Central ground-glass opacity surrounded by denser crescentic (semicircular to circular) consolidation at least 2 mm in thickness
Also known as atoll sign
Seen in 20% but not specific for COP
Also described in lymphomatoid granulomatosis and paracoccidioidomycosis
Radiographic Findings
Radiography
Findings less well identified compared to CT
Focal or multifocal consolidation, remains chronic after course of antibiotic therapy; clue to conditions that give chronic consolidation pattern
Chronic consolidation arbitrarily defined as persistent more than 30 days
Differential for chronic consolidation
Bronchioloalveolar cell carcinoma
Cryptogenic organizing pneumonia
Alveolar sarcoidosis
Alveolar proteinosis
Lymphoma or pseudolymphoma
Chronic eosinophilic pneumonia
Lipoid pneumonia
Chronic aspiration
DIFFERENTIAL DIAGNOSIS
Chronic Eosinophilic Pneumonia
Usually in upper lung zone (eosinophilia absent in COP)
Nodules, nonseptal linear pattern, reticulation and peri-bronchiolar distribution more common in COP
Septal lines more common in chronic eosinophilic pneumonia
Bronchioloalveolar Cell Carcinoma (BAC)
BAC not predominately subpleural
Foci usually predominantly ground-glass opacities
Sarcoidosis, Alveolar
Few large airspace masses with air-bronchograms
Preferentially involves upper lung zones
Usually associated with symmetric hilar and mediastinal adenopathy
Lung Cancer (Solitary Mass)
Aspiration
Opacities not as chronic or peripheral as COP
Predominately in dependent lung segments
Typical predisposing conditions: Esophageal motility disorder, obtundation, alcoholism
Lipoid Pneumonia
Lipoid pneumonia may have fat density in areas of consolidated lung at CT
May present with “crazy-paving” appearance on CT
History of lipoid ingestion: Oily nose drops, mineral oil
Pulmonary Embolism
Multiple infarcts peripherally located in bases (identical to COP)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree