Trauma
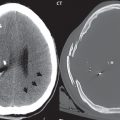
A few definitions are in order to introduce the topic of brain trauma. A cortical contusion is simply a bruise of the brain′s surface. The inferofrontal and anteroinferior temporal portions of these two lobes of the brain are particularly vulnerable ( Fig. 1.47 ). The term “coup” is used to reference an injury that lies directly beneath the area of impact. The term “contrecoup” is used for an injury that occurs remote from the site of impact, along a direct line but opposite to this site, caused by acceleration effects. Imaging of acute head injury is the province of CT. Acute intracranial hemorrhage and bone fractures are well seen and evaluated ( Fig. 1.48 ).


Parenchymal Injury
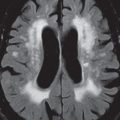
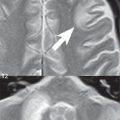
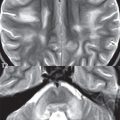
Diffuse axonal injury (DAI) and cortical contusion are the two most common findings in the setting of trauma with a closed head injury. Subcortical gray matter injury also occurs, but much less frequently. DAI occurs due to shear-strain forces with rapid deceleration. There are three common locations (given in order from the most to the least common, which also parallels the degree of severity of the injury from least to most): the gray–white matter junction, the corpus callosum (splenium), and the brainstem ( Fig. 1.49 ). CT is often normal in this setting.

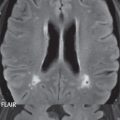
Injuries at the gray–white matter junction will be seen as multiple small foci of abnormal high signal intensity on FLAIR scans. Most commonly these involve the frontal lobe. If the lesions are hemorrhagic, they will be well seen in the acute time frame on T2*-weighted gradient echo scans, due to the presence of deoxyhemoglobin. Susceptibility weighted imaging offers a further improvement in sensitivity to T2* effects, and in cases with hemorrhage will demonstrate more extensive injury. The second most common injury seen in DAI is a shear injury of the corpus callosum, with the majority involving the splenium. This injury and the subsequently described injury of the brainstem are usually not seen in isolation but with extensive shear injury at the gray–white matter junction. In the brainstem, lesions are seen most often in the pons and the dorsolateral midbrain. Lesions in the brainstem carry a very poor prognosis, often with a fatal outcome.
In patients evaluated months to years following severe head trauma, the residual from DAI involving injury at the gray–white matter junction can be visualized, with high signal intensity on FLAIR due to gliosis and low signal intensity on T2*-weighted images due to the presence of hemosiderin. Encephalomalacia, with both gliosis and cystic changes, will be seen in areas of prior contusion. In severe injury, there may be resultant generalized cerebral atrophy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree