Specific Indications
Chest and cardiac trauma
The majority of patients who sustain a penetrating cardiac injury do not survive to receive medical care due to exsanguinating hemorrhage. Hemodynamically unstable patients who survive transport to the hospital should proceed immediately to the operating room for exploration without any further imaging. For patients who remain hemodynamically stable after penetrating thoracic injuries, there is a definite role for rapid bedside ultrasound as part of their evaluation.
Of those that survive penetrating injury to the heart, approximately 2% of patients will develop pericardial tamponade. Often the signs and symptoms of pericardial tamponade can be delayed by hours or even days. Patients may be completely asymptomatic until rapid decompensation ensues with the development of shock and potentially cardiac arrest. It is crucial to detect a pericardial effusion as quickly as possible to prevent this from occurring. Ultrasound can provide evidence of tamponade, such as right ventricular diastolic or atrial collapse, well before clinical symptoms appear. A 10-year retrospective review by Plummer et al. in 1992 found that bedside ultrasound significantly decreased the time to diagnosis of penetrating cardiac injury and had a direct impact on the survival rate and neurologic outcome of survivors.8
One prospective cohort study of consecutive penetrating torso injury patients at a Level I trauma center found that ultrasound examination had a sensitivity of 48% and therefore lacked sufficient sensitivity to be used alone in determining the need for operative intervention after penetrating torso injury.9 Nevertheless, the FAST examination can still be used to screen trauma victims with penetrating chest injury for a pericardial effusion or other cardiac defects and determine the need for pericardial window or more extensive operative intervention.
Blunt trauma to the heart is a relatively uncommon mechanism of injury but can be underestimated and often missed due to a wide range of clinical presentations and nonspecific symptoms. Injuries can include myocardial contusions with resulting wall motion abnormalities, aortic transection, valvular injuries, or ventricular wall rupture. Symptoms may range from palpitations to life-threatening arrhythmias to cardiogenic shock. To date there is no gold standard test for accurate diagnosis of blunt cardiac injury. Aortography is the preferred diagnostic test for suspected aortic transection but is costly, time-consuming, and not always readily available. Along with a high index of suspicion various studies have shown a beneficial role for ultrasound (in addition to cardiac enzymes and electrocar-diography) in the diagnosis of blunt cardiac injury.10 Two dimensional echocardiography can provide a direct view of wall motion abnormalities, intimal flaps, valve abnormalities, pericardial effusions, and severe global dysfunction, and should be performed on all patients that sustain blunt chest trauma.
While the FAST examination was initially meant to be a bedside tool for the detection of hemoperitoneum and hemopericardium, its use has recently expanded to include the identification of blood, fluid, or air in the pleural space as part of the E-FAST examination. In fact, ultrasound has a sensitivity equivalent to that of chest x-ray for detecting pneumothoraces4 and is even more sensitive than x-ray for visualizing fluid in the pleural space.
A chest radiograph requires more than 150 mL of fluid to be present in the pleural cavity in order to detect an effusion.11 With a sensitivity of 93% for pleural effusion, ultrasound can detect as little as 20 mL of fluid and can be carried out much more rapidly.11 While a chest radiograph should still be done as part of the initial assessment of the trauma patient, ultrasound is more frequently being used to determine the need for an immediate tube thoracostomy.11,12
Abdominal trauma
The FAST examination has been most widely utilized and studied in the diagnosis and management of blunt abdominal trauma. Many algorithms have been developed to assess patients that have sustained blunt abdominal trauma (Figure 9-1), the majority of which suggest that a hemodynamically unstable patient with a positive FAST warrants a laparotomy. Although not yet well validated, several hemoperitoneum scoring systems have found that the amount of free fluid detected on ultrasound can accurately predict the need for therapeutic laparotomy.13 According to such algorithms, patients with a negative ultrasound should undergo DPL followed by further evaluation for an extra-abdominal source of bleeding (ie, into the chest or extremity) if the DPL is negative. It is also important to note that patients suffering from spinal shock or head trauma can present with hemodynamic instability and a negative FAST examination. These patients may require further imaging after resuscitation and stabilization to further elucidate the extent of their injuries. While the role of ultrasound in the evaluation of unstable patients is well established, its reliability in the assessment of stable trauma patients is less clear. Several studies have questioned the routine use of ultrasound as a primary tool in assessing hemo-dynamically stable patients, especially multiply injured patients with a high Injury Severity Score (ISS), who are more likely to have ultrasound-occult injuries.14,15 These studies have found that it may lead to the underdiagnosis of abdominal injury, in part due to its lower sensitivity for detecting parenchymal injury.14 Therefore, a positive FAST in a hemodynamically stable patient should generally be followed by a CT scan to further evaluate the site of injury and minimize the rate of negative laparotomies, whereas a stable patient with a negative FAST can be observed with serial examinations and/or further imaging depending on clinical suspicion and mechanism of injury. While ultrasound is less sensitive than CT scan for detecting parenchymal injury and retroperitoneal bleeding, it has proven to be extremely useful in identifying intraperitoneal fluid that might otherwise be missed by other screening modalities.
Figure 9-1. Algorithm for the management of patients with blunt abdominal injury based on their hemodynamic status and results of FAST examination.
The FAST examination has been proven to be highly specific, but less sensitive for detecting hemoperitoneum in patients with penetrating abdominal injuries. One study found the sensitivity of FAST alone for the evaluation of penetrating torso injury to be 67%, with a positive predictive value of 92%, and a negative predictive value of 89%.16 The authors determined that the routine use of ultrasound in penetrating torso injury was useful for the detection of peritoneal fluid and it can be considered an important tool for guiding management in the setting of multiple penetrating injuries. However, it is important to note that a negative FAST examination does not rule out abdominal injury, such as a diaphragm or hollow viscus injury, and further evaluation is recommended.
Orthopedic injury
While it is not considered one of the primary goals of trauma resuscitation, the evaluation of skeletal injuries is an important adjunct to the secondary survey. Even non-life-threatening orthopedic injuries should be evaluated and managed without significant delay. Radiography has traditionally been the diagnostic test of choice for assessing bone fractures. However, there is growing interest in bedside ultrasound as a more rapid, noninvasive method for diagnosing orthopedic injuries. Ultrasound tends to be less reliable in the setting of compound fractures and injuries in close proximity to joints, but recent studies have demonstrated that it may be comparable to radiography for the diagnosis of long bone fractures with sensitivity and specificity of 89% and 100%, respectively.17
Ultrasound has also proven to be useful for guiding the manipulation and reduction (M&R) of distal radius fractures in adults and forearm fractures in children.18,19 Ang et al. prospectively studied the use of ultrasound-guided M&R in 62 patients with distal forearm fractures and compared it to the blind manual palpation technique. They found that post-reduction radiographic findings were similar after both techniques, but there was slightly improved volar tilt in the ultrasound group (P = .048). The rate of operative intervention was also lower among those who underwent ultrasound-guided reduction (4.9% versus 16.7%; P = .02).18 Ultrasound reduced the need for repeat M&R and therefore decreased the need for sedation and analgesia.
 Patient Populations Who Benefit from Trauma Ultrasound
Patient Populations Who Benefit from Trauma Ultrasound
The FAST examination is most useful in the rapid evaluation of hemodynamically unstable patients when the etiology of shock is unclear. Ultrasound is also useful in patients who have an unreliable examination (ie, in the setting of intoxication or head injury) and who require frequent re-assessments. In patients who require urgent transfer to a trauma center, it can also be a useful test during air or ground transport due to its portability and ease of use.
Fast examination and pregnancy
Pregnant women comprise another population of patients in whom ultrasound is particularly useful. DPL is relatively contraindicated in pregnancy and while CT scan should be performed if clinically indicated, there are potential teratogenic effects of radiation that can be avoided with the use of ultrasound.
Ultrasound and pediatric trauma
While the use of the FAST examination is clearly beneficial in the evaluation of adult trauma patients, the utility of trauma ultrasound has not been studied as extensively in children. The presence of physiologic free fluid in their pelvis makes interpreting the FAST examination slightly more challenging in pediatric patients. Limited studies have determined the sensitivity of FAST to range from 30% to 80%, and specificity 95% to 100% in children who have sustained blunt abdominal trauma.20 When fluid is visualized outside of the pelvis in children, the sensitivity for solid organ injury increases to 90% and there is an 87% and 97% positive and negative predictive value, respectively.,21
It is important to note that a positive FAST examination in a hemodynamically stable pediatric trauma patient should still be followed by a CT to further evaluate the source of hemoperitoneum. A negative FAST, however, does not always preclude the need for a CT scan but it may help to avoid unnecessary radiation exposure in patients who have a very low likelihood of intraperitoneal injury. In hemodynamically unstable pediatric trauma patients, the FAST examination can rapidly help guide decisions regarding the need for operative intervention. Further studies are clearly needed to evaluate the clinical utility of the FAST examination for pediatric trauma patients, especially given that most intra-abdominal injuries in children are managed nonoperatively.
More recent studies have demonstrated a role for bedside ultrasound in the evaluation and management of fractures in pediatric trauma patients. Not only is it highly sensitive for detecting certain types of orthopedic injuries, but it can be done rapidly and minimizes the risk of radiation exposure to pediatric patients. Clavicle fractures are one of the most common orthopedic injuries in children. A recent study by Cross et al. demonstrated that bedside ultrasound can accurately diagnose pediatric clavicle fractures with 95% sensitivity and 96% specificity, especially in patients with a high likelihood of fracture.22 Another study prospectively evaluated the use of ultrasound for the reduction of forearm fractures in children and found it to have an initial success rate of 92% (95% CI, 75–99%).19 It could be used to immediately assess for realignment of the bones and minimize the use of postreduction x-rays.
Disaster and mass casualty incidents
Mass Casualty Incidents (MCIs) are situations that require the rapid triage of large numbers of injured patients where the volume of injuries exceeds the resources and capabilities of medical responders and personnel in the field. A rapid, accurate screening and diagnostic tool is necessary to identify those who require immediate intervention, and thereby improve patient safety and outcomes.
Sarkisian et al was among the first to describe point-of-care ultrasound in a mass casualty setting, after an earthquake in northwestern Armenia in 1988 that injured more than 150,000 people.23 Four hundred patients were evaluated with ultrasound in a 72-hour period, 96 examinations showed positive findings and 16 operations were performed based on these results with 1% false negative rate.22 This and other more recent studies have shown that ultrasound is both sensitive and specific in resource-limited situations, and is becoming a more widely used tool by first responders in remote settings after natural disasters, terrorist attacks, and military mass casualties. It has been used both for initial assessment and surgical decision making, and prioritizing the need for further imaging. It can also be performed by adequately trained nonphysician and prehospital personnel in the setting of mass casualty incidents.
A recent paper by Stawicki et al. proposed the concept of a comprehensive ultrasound assessment of the chest, abdomen, vena cava, and extremities in acute triage (CAVEAT).24 In addition to the standard FAST views, they proposed that evaluation of the inferior vena cava could yield important information about filling pressures and intravascular volume status, and help identify those who are likely to respond to volume expansion. Despite taking several minutes longer than the traditional FAST examination, the CAVEAT protocol could also be used to identify occult fractures when radiography is unavailable and thus lead to more timely management and utilization of resources.24
Data on its use in military deployment are sparse, but recent reports indicate that handheld ultrasound is becoming a more routinely used tool by forward medical units in combat environments.24 Images can be transmitted by satellite from remote areas for expert interpretation and help influence treatment and evacuation strategies. Training courses currently exist to teach military surgeons the FAST technique.
 Contrast-Enhanced Ultrasound
Contrast-Enhanced Ultrasound
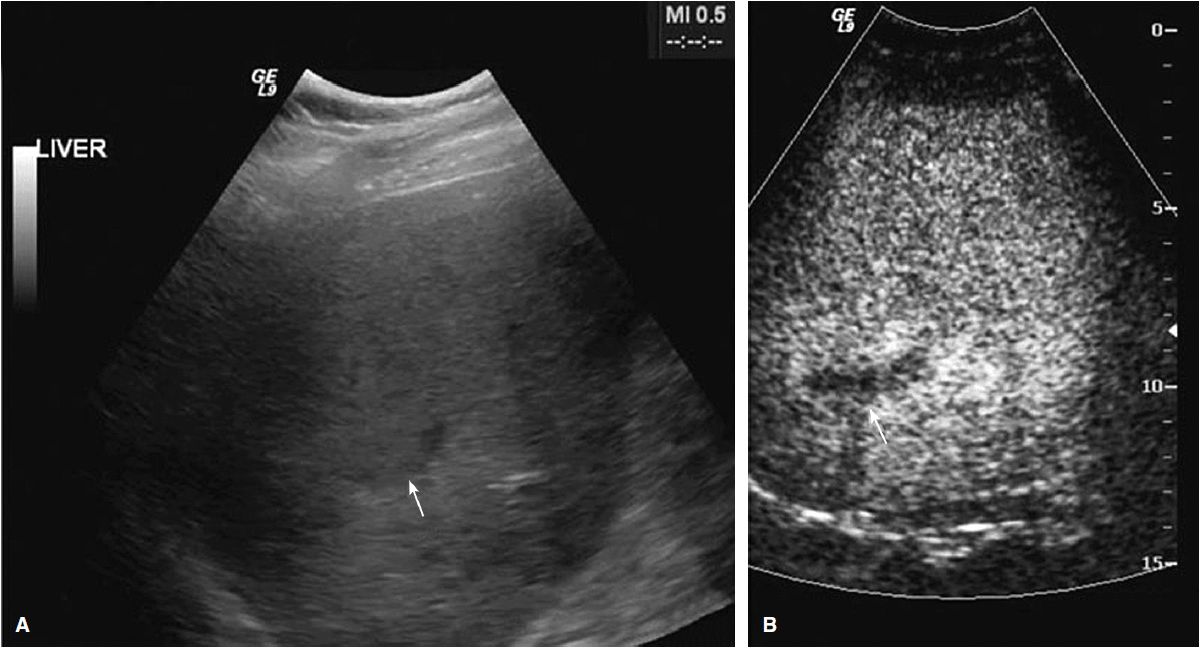
The role of contrast-enhanced ultrasound (CEUS) in the assessment of trauma patients is also a recent subject of interest. CEUS uses contrast agents containing highly stable microbubbles filled with an inert gas that resonate at low acoustic pressure. Continuous real-time images are produced based on the microbubble signal that can provide important information on solid organ injury.25 A growing body of evidence suggests that CEUS has increased sensitivity for detecting subtle parenchymal injuries, as well as vascular lesions, active hemorrhage, and delayed pseudoaneurysms.26,27 With sensitivities ranging from 63–99%, studies have shown CEUS to be more sensitive than ultrasound for detecting solid organ injury.25,26 Solid organ lacerations and hematomas are nonenhancing due to lack of blood supply and appear as dark anechoic areas on contrast-enhanced ultrasound (Table 9-1 and Figure 9-2). Advantages of CEUS include its lack of ionizing radiation and nephrotoxicity, which make it preferable for use in children and pregnant women, its ease of use, and ability to visualize arterial and venous phases.
Figure 9-2. (A) Grayscale ultrasound showing subtle area of abnormal hepatic echostructure (white arrow); (B) CEUS with hypoechoic region consistent with parenchymal laceration (white arrow). (From Cokkinos D, et al. Ultraschall Med. 2012;33(1):60–67.)
Limitations to CEUS include its inability to adequately visualize retroperitoneal structures and skeletal injuries. It also requires intravenous access and may take slightly longer to obtain that traditional grayscale imaging. Therefore, its use should be restricted to hemodynamically stable trauma patients with a high likelihood of parenchymal injury in whom CT is unavailable or contraindicated due to iodinated contrast allergy.
NORMAL ANATOMY
Free intraperitoneal fluid collects in dependent areas formed by peritoneal reflections and mesenteric attachments, including the retrovesicular space (in men), the rectouterine pouch or the pouch of Douglas (in women), and right and left paracolic gutters. The right paracolic gutter connects Morison pouch with the pelvis. The left paracolic gutter courses to the splenorenal recess. The retrovesical pouch is the most dependent area of the male in supine position, while the pouch of Douglas is the most dependent area in the supine female.
Free fluid that accumulates on the right side of the intraperitoneal cavity will flow into the hapatorenal recess (Morison pouch) before traveling down the right paracolic gutter into the pelvis. Morison pouch is the most common location for free fluid to collect in the setting of parenchymal injury due to blunt trauma. Free fluid in the left upper quadrant will collect in the left subphrenic space and less commonly in the splenorenal space. With smaller collections, the phrenocolic ligament will often block the flow of fluid from the left paracolic gutter to the splenorenal recess, so fluid will usually spread across the midline to the right upper quadrant.
NORMAL APPEARANCE OF ULTRASOUND
 Simple Fluid
Simple Fluid
Intraperitoneal free fluid is anechoic on ultrasound. It is jet black and has a “pointy” appearance, forming around bowel and viscera in contrast to the “rounded” appearance of fluid within the lumen of a vessel or organ.
 Complex Fluid
Complex Fluid
Complex fluid on ultrasound is usually indicative of hemoperitoneum. Immediately after traumatic injury, blood appears sonolucent (hypoechoic) but becomes echogenic as clot begins to form over several hours. As it forms a hematoma, it may even appear hyperechoic. Blood becomes sonolucent again as fibrinolysis occurs approximately 12–24 hours from the time of injury.28 It is important to recognize that echogenic blood is likely to be located at the site of injury and can therefore help guide intervention; however, it may be similar in echotexture to the surrounding parenchyma and can also be missed on ultrasound.
 Solid Organ Appearance
Solid Organ Appearance
The spleen lies in a posterolateral position and has an echo-genic capsule with a homogeneous cortex. Despite its gray echotexture similar in appearance to the liver, it is smaller in size and the intraparenchymal vessels are less visible. The kidneys lie inferior to the liver and spleen in a retroperito-neal location. The renal cortex has a similar echotexture but is slightly more hypoechoic than the liver or spleen and is outlined by the brightly echogenic Gerota’s fascia.
 Hollow Organ Appearance
Hollow Organ Appearance
The bowel varies in appearance depending on whether it is filled with air, fluid, or solid matter. When the bowel lumen contains air, it may distort the appearance of surrounding structures. If it contains fluid or solid material, the bowel may have a cystic appearance but peristaltic waves are visible, distinguishing it from a stationary cystic structure.
 Parenchymal Findings
Parenchymal Findings
While the utility of ultrasound for detecting free fluid is well documented, its utility for the identification of solid organ injury is less clear. Moreover, both splenic and liver lacerations can occur with or without hemoperitoneum; therefore, relying on the presence of free intraperito-neal fluid for the diagnosis of solid organ injury can be misleading.
If done accurately, the identification of parenchymal architectural abnormalities can help guide us to the site of injury and can be instrumental in planning surgical intervention if necessary. Lacerations often appear as an irregular contour or hyper- or hypoechoic areas within the visceral organ, whereas subcapsular hematomas may look like an echogenic rim.28 Splenic parenchymal injuries can be diffusely heterogeneous or disorganized patterns with cystic or hypoechoic areas. This is in contrast to liver parenchymal injuries that usually appear as focal hyperechoic lesions.28
Injuries to the kidney can appear as a focal lesion or heterogeneity of the parenchyma that replaces normal kidney in the renal fossa, and adrenal injuries typically present as discreet mass above the kidney. A pseudoaneurysm may appear as a cyst-like anechoic mass within an organ, but can be differentiated from a cyst using Doppler to demonstrate flow within the pseudoaneurysm.28 In situations where the presence of parenchymal injury is not clear, a higher frequency probe (7.5-MHz linear array probe) may more accurately detect tissue irregularities, especially in thin patients.29
SCANNING TECHNIQUES AND COMMON FINDINGS
Unlike a comprehensive ultrasound study that must visualize each organ in multiple planes, the FAST examination can be done with limited scanning planes with a patient lying supine in order to detect the presence or absence of free fluid. The FAST typically encompasses four views: the pericardial view, the perihepatic view, the perisplenic view, and the pelvic view. An anterior thoracic view is sometimes added to the standard views to assess for the presence of a pneumothorax. Each of these will be discussed in more detail below.
 Pericardial View
Pericardial View
Technique
The pericardial view looks at the space between the right ventricle and the liver in order to rule out the presence of a pericardial effusion. With the patient lying supine, the probe (with the marker dot pointing toward the right) should be placed in the subxiphoid area and angled toward the patient’s left shoulder (Figure 9-3). Ensure that the transducer is lying flush with the skin. Pressing firmly just below the xiphoid should reveal the right ventricle next to the left hepatic lobe. To improve the image, consider having the patient inhale deeply and hold their breath (if possible), with the transducer positioned further toward the patient’s right side.
Figure 9-3. Positioning of the ultrasound probe to obtain the subxiphoid view. This visualizes the space between the right ventricle and the liver to rule out a pericardial effusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree