Clinical Presentation
The patient is a 38-year-old man who was thrown from a motorcycle during a motor vehicle collision and presented in the emergency department with severe neck pain, right upper extremity pain, and bilateral lower and upper extremity weakness, right more than left. Bowel and bladder function are intact.
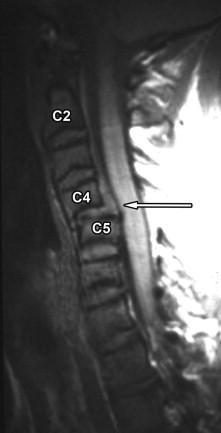
Imaging Presentation
Radiographs and computed tomography (CT) scan (not shown) demonstrated anterior subluxation of C4 vertebral body on C5, widening of C4-5 intervertebral disc space posteriorly, and bilaterally subluxed C4 facets relative to C5. Magnetic resonance (MR) imaging confirms C4 on C5 subluxation and further reveals traumatic disc herniation compressing the spinal cord at the C4-5 level, right more than left ( Figs. 27-1 to 27-3 ) .


Discussion
The vast majority of disc herniations in adults cannot be related to a specific traumatic episode. A traumatic disc herniation is one that occurs with a traumatic event. Most traumatic herniations are diagnosed in the acute post-traumatic setting with MR imaging. Commonly associated injuries include vertebral fracture, vertebral subluxation, epidural hematoma, traumatic cord compression, cord contusion, and paraspinal ligamentous disruption. Concomitant brain contusions or intracranial hemorrhage may also be present.
Herniated discs commonly occur with acute cervical spine trauma. In one series, traumatic disc herniations were demonstrated by MR imaging in 42% of patients with acute cervical spine trauma. In the same series, traumatic disc herniations occurred in 80% of patients presenting with bilateral locked facets and 100% of patients with anterior cord syndrome. In adults, traumatic disc herniations most commonly occur in the cervical spine but also occur in the thoracic or lumbar spine.
Most believe traumatic disc herniations occur because of excessive mechanical force on the disc. During normal axial loading, the normal nucleus and inner annulus is compressed slightly in the craniocaudal dimension, which in turn causes an increase in radially directed (shear) force, which causes slight circumferential annular expansion. Sharpey’s outer annular fibers, composed of dense type II collagen, resist these outward shear forces. When traumatic compressive, rotational, or radial forces are exerted upon the spine and intervertebral discs, the shear force upon the annulus is likely far greater than normal and the annulus ruptures allowing nuclear and inner annular tissue to escape into the anterior epidural space or neural foramen. Pre-existing internal disc derangement, such as degenerative annular fissures, likely renders the disk more susceptible to herniation when the intervertebral disc is subjected to traumatic axial loading (compressive) forces or radial (shear) forces.
Small traumatic disc herniation may or may not be symptomatic. However, the vast majority of traumatic disc herniations are symptomatic. Commonly, the patient has neck or low back pain and often radicular pain depending on the location of the disc herniation. In one series of patients with symptomatic traumatic disc herniations, 63% had radiculopathy, 30% had both radiculopathy and myelopathy, and 7% had only myelopathy.
Cervical hyperflexion or hyperextension injuries may cause traumatic disc herniations ( Figs. 27-4 and 27-5 ) . Traumatic disc herniations may occur with or without vertebral fractures ( Figs. 27-6 to 27-8 ) . If the traumatic disc fragment is large and compresses the cord, or if there is an associated epidural hematoma, there is a high incidence of anterior cord syndrome resulting from compression of the anterior spinal artery. The anterior spinal artery supplies the anterior two thirds of the spinal cord so a large portion of the anterior spinal cord is at risk for traumatic or ischemic injury. In anterior cord syndrome, the patient experiences considerable weakness if the anterior horns are involved. Pain and temperature sensation may be disturbed. Dorsal column function including fine touch and proprioception are often intact.














