[9].
Within the last few years is has become more difficult to obtain iridium-192 wire in the UK. The future trend is to carry out implants using remote afterloading machines. Although HDR machines are mainly used for gynaecological insertions they can also be used to deliver interstitial or even surface of skin treatments. They can be used as the sole method of treatment or to deliver a boost doses after external beam radiotherapy.
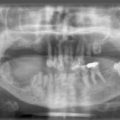
A typical example of this is the treatment of prostate cancer. Plastic catheters can be inserted under general anaesthetic using needles inserted through a template under ultrasound control. A high intensity iridium source can then move into each of the catheters to occupy pre-determined dwell positions for specific times. HDR treatments given in 2 to 4 single fractions for early prostate cancer are an alternative to permanent iodine-125 seed implants.
Patients with locally advanced prostate cancer were treated in a randomised control trial either by external beam radiotherapy only or by external beam plus an HDR brachytherapy boost. The patients receiving a brachytherapy boost had a 15% improvement in local control (assessed by PSA measurements) compared to those treated by external beam only.
Pulsed dose rate machines typically delivering a dose rate of 1 Gy per hour try to reproduce the therapeutic results seen following iridium-192 wire implants. A series of catheters are inserted into the treatment volume. The iridium-192 source enters the catheters once an hour to deliver a dose of 1 Gy to the treatment volume over a few minutes. As radioactive material is only present for a few minutes during each hour the patient may have visitors or receive nursing support between each pulse of radiation.
Except for prostate and gynaelogical cancers, brachytherapy will probably be a ‘niche’ area suitable for patients being referred to only a few centres where resources and experience can be concentrated.
References and further reading
[1] Dale R.G., Jones B. The clinical radiobiology of brachytherapy. Brit J Radiol. 1998;71:465–483.
[2] Sundar S., Symonds P., Deehan C. Tolerance of pelvic organs to treatment for carcinoma of cervix. Clin Oncol. 2003;15:240–247.
[3] Denton A.S., Bond J., Mathews S., et al. National audit of the management and outcome of carcinoma of the cervix treated by radiotherapy in 1993. Clin Oncol. 2000;12:347–353.
[4] International Commission on Radiation Units and Measurement. Dose and volume specification for reporting intracavitary brachytherapy in gyneacology. Maryland: Bethesda, 1985. ICRU report 38
[5] Aird E.G.A., Jones C.H., Joslin C.A.F., et al. Recommendations for brachytherapy dosimetry. British Institute of Radiology, 1993.
[6] Orton C.G., Seyedsadr M., Somnay A. Comparison of high and low dose-rate remote afterloading for cervix and the inportance of fractionation. Int J Radiat Oncol Biol Phys. 1991;21:1425–1434.
[7] Moule R.N., Hoskins P.J. Non-surgical treatment of localised prostate cancer. Surgical Oncology. 2009;18:255–267.
[8] Acher P., et al. Prostate brachytherapy: dosimetric results and analysis of a learning curve with a dynamic dose-feedback technique. Int J Radiat Oncol Biol Phys. 2006;65:694–698.
[9] Vale C.L., Tierney J.F., Davidson S.E., Drinkwater K.J., Symonds P. Substantial improvement in UK cervical cancer survival with chemoradiotherapy: results of a Royal College of Radiologists’ Audit. Clin Oncol. 2010;22:590–601.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree