Functions
• General sensory afferent (GSA). Somatic sensory from skin and mucous membranes of the face, forehead, anterior scalp, nasal and oral cavities, conjunctiva, paranasal sinuses, teeth, anterior two thirds of tongue, and part of the external surface of the tympanic membrane as well as the dura of anterior and middle cranial fossae.
• Special visceral efferent (SVE). Branchial motor to muscles of mastication.
Anatomy
• The trigeminal nerve (Fig. 5.1) leaves the midlateral surface of the pons as a large sensory root (portio major) and a smaller anteromedial motor root (portio minor). It enters the subarachnoid space in the cerebellopontine angle cistern. It travels anterolaterally then pierces the dura mater at the petrous apex to enter Meckel’s cave. Meckel’s cave is a cerebrospinal fluid (CSF)-filled space between two layers of dura over the petrous portion of the temporal bone that encloses the trigeminal ganglion and all three roots of the trigeminal nerve. It lies just posterior and inferolateral to the cavernous sinus (Fig. 5.2).
• The trigeminal nerve has three major divisions—ophthalmic (cranial nerve [CN] V1), maxillary (CN V2), and mandibular (CN V3).
Sensory Portion (Portio Major)
• Sensory neuron cell bodies lie in the sensory ganglion (semilunar, gasserian, or trigeminal ganglion) in the Meckel cave on the floor of the middle cranial fossa.
• The trigeminal ganglion receives fibers from all three divisions of the trigeminal nerve: CN V1, V2, and V3.
• From this ganglion, the fibers of the sensory root (portio major) enter the pons, course dorsomedially, and terminate in three major nuclear complexes within the brainstem (Fig. 5.1):
1. Principal sensory nucleus of CN V. Located in the pons. Fibers carrying fine touch and pressure synapse here and then ascend in the trigeminal lemniscus, which crosses to the opposite side of the brainstem, and the smaller dorsal trigeminothalamic tract (uncrossed), both of which terminate in the ventroposteromedial (VPM) nucleus of the thalamus.
2. Spinal trigeminal nucleus. Extends from the principal sensory nucleus (in pons) caudally all the way to C-2 (cervical spinal cord), where it merges with the substantia gelatinosa (pain-related lamina in the spinal cord). The spinal trigeminal nucleus also gets input from CN VII, IX, and X. Fibers carrying pain and temperature (and crude touch as well) descend via the spinal trigeminal tract, synapse in the spinal trigeminal nucleus, then cross via the ventral trigeminothalamic tract to ascend to the VPM nucleus of the thalamus. There are also other pathways from the spinal trigeminal nucleus to intralaminar thalamic nuclei and the reticular formation that mediate affective and arousal components of facial pain.
3. Mesencephalic nucleus of CN V. Extends from principal sensory nucleus (in pons) cranially to superior colliculus (in midbrain). This nucleus contains the primary sensory neurons (i.e., there is no synapse in the trigeminal ganglion) involved in proprioception of head muscles (especially masticatory and extraocular muscles). This is the only case in which primary sensory neurons lie within the central nervous system (CNS) instead of in the peripheral ganglia.
• Information from the VPM nucleus of the thalamus travels to the ipsilateral somatosensory cortex (postcentral gyrus).
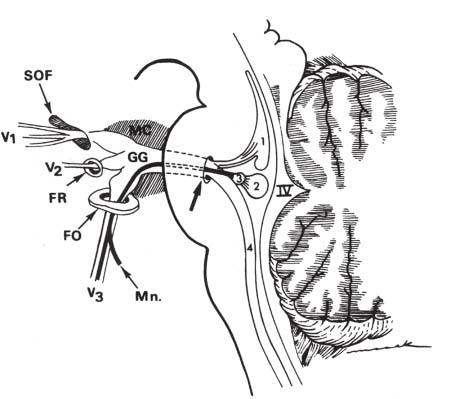
Fig. 5.1 Intracranial course of the trigeminal nerve. Four brainstem nuclei contribute to the trigeminal nerve: mesencephalic nucleus (1), principal sensory nucleus (2), motor nucleus (3), and spinal nucleus (4). Fibers from these nuclei coalesce to exit the lateral pons at the root entry zone (arrow). IV, fourth ventricle; FO, foramen ovale; FR, foramen rotundum; GG, gasserian ganglion; MC, Meckel’s cave; Mn, motor branches of the mandibular nerve; SOF, superior orbital fissure. (From Harnsberger HR. Handbook of Head and Neck Imaging (2nd ed.) St. Louis, MO: Mosby, 1995. Reprinted with permission.)
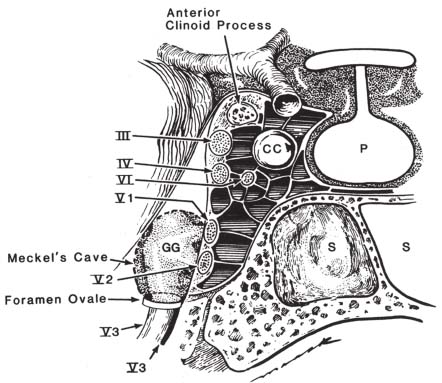
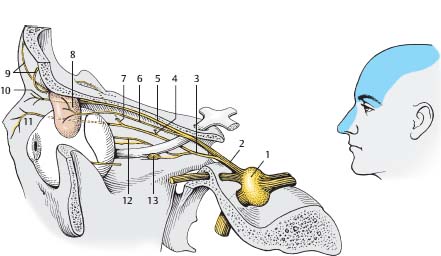
Fig. 5.3 Ophthalmic nerve (CN V1). (1, gasserian [trigeminal, semilunar] ganglion; 2, ophthalmic nerve; 3, nasociliary nerve; 4, posterior ethmoidal nerve; 5, frontal nerve; 6, lacrimal nerve; 7, anterior ethmoidal nerve; 8, lacrimal gland; 9, supraorbital nerve; 10, supratrochlear nerve; 11, infratrochlear nerve; 12, long ciliary nerves; 13, ciliary ganglion.)
Ophthalmic Division (CN V1 (Fig. 5.3)
• Purely sensory.
• From trigeminal ganglion courses in lateral wall of cavernous sinus inferior to CN IV (Fig. 5.2), enters orbit through superior orbital fissure (SOF)
• Structures in SOF: CNs III, IV, V1 (nasociliary, frontal, and lacrimal branches), VI, sympathetic fibers from internal carotid artery (ICA) plexus, superior ophthalmic vein, orbital branch of middle meningeal artery, and recurrent meningeal branch of lacrimal artery
• Before leaving cavernous sinus, divides into
1. Tentorial (meningeal) branch. Innervates dura of cavernous sinus, sphenoid wing, anterior fossa, petrous ridge, Meckel’s cave, tentorium cerebelli, posterior falx cerebri, and dural venous sinuses. Note that this branch does not exit via the SOF.
2. Frontal nerve. Enters orbit above annulus of Zinn, divides into supraorbital nerve (innervates frontal sinuses, forehead, scalp back to lambdoidal suture in midline) and supratrochlear nerve (medial conjunctiva, medial upper lid, forehead, side of nose).
3. Lacrimal nerve. Enters orbit above annulus of Zinn. Innervates lateral conjunctiva and skin near lacrimal gland. Receives postganglionic parasympathetic fibers (from CN VII greater superficial petrosal nerve [GSPN]) for lacrimation from zygomatic nerve of CN V2 (see below).
4. Nasociliary nerve. Enters orbit through annulus of Zinn. Has several branches:
• Infratrochlear nerve innervates lacrimal sac, caruncle, conjunctiva, and skin of medial canthus.
• Anterior and posterior ethmoidal nerves innervate ethmoidal air cells.
• Internal nasal nerve innervates the anterior portion of the nasal septum.
• External nasal nerve innervates the skin of the dorsum and tip of the nose.
• Long ciliary nerves carry sensation from ciliary body, iris, and cornea. They also convey sympathetic fibers from the ICA to the dilator pupillae muscle.
• Short ciliary nerves carry sensation from the globe. They also convey postganglionic parasympathetic fibers (from CN III) from the ciliary ganglion to the sphincter pupillae and ciliary muscles.
Maxillary Division (CN V2) (Fig. 5.4)
• Purely sensory.
• Middle meningeal nerve is given off from the maxillary nerve directly after its origin from the trigeminal ganglion. It accompanies the middle meningeal artery and innervates the dura of middle cranial fossa.
• From the trigeminal ganglion it courses in inferolateral wall of cavernous sinus inferior to CN V1 (Fig. 5.2).
• Exits cranial vault via foramen rotundum to enter pterygopalatine (sphenopalatine) fossa.
• Contents of foramen rotundum: CN V2, emissary veins, artery of foramen rotundum.
• In pterygopalatine fossa, branches into
1. Infraorbital nerve. Enters orbit via inferior orbital fissure (IOF). Structures in IOF: infraorbital nerve, zygomatic nerve, infraorbital artery and vein, and inferior ophthalmic vein. Then infraorbital nerve travels under orbital periosteum; then enters and traverses the infraorbital canal and exits via the infraorbital foramen to innervate the midportion of the face. Along its course it gives off
• Posterior superior alveolar nerves. To maxillary sinus, molar teeth of maxilla, and adjacent gums and cheek.
• Middle superior alveolar nerve. To maxillary premolar teeth.
• Anterior superior alveolar nerves. To the maxillary incisor and canine teeth.
• Inferior palpebral branches to lower lid skin and conjunctiva, external nasal branches to side of nose, and superior labial branches to upper lip.
2. Zygomatic nerve. It enters the orbit via the IOF, and gives off two branches:
• Zygomaticotemporal nerve. Runs along lateral wall of the orbit and passes through the zygomaticotemporal foramen in the zygomatic bone to enter the temporal fossa and innervates the skin of the side of the forehead and the lateral angle of the orbit.
• Zygomaticofacial nerve. Runs along inferolateral wall of the orbit and passes through the zygomaticofacial foramen in the zygomatic bone to reach the face and innervates the skin on the prominence of the cheek.
• Postganglionic parasympathetic fibers originating from the GSPN of CN VII that have just synapsed in the pterygopalatine ganglion join the zygomatic nerve and follow it into the IOF, travel with the zygomaticotemporal nerve, and then intraorbitally connect with fibers of the lacrimal nerve (of CN V1), ultimately providing the lacrimal gland with secretomotor innervation.
3. Other sensory fibers pass through the pterygopalatine ganglion without synapsing and include the following:
• Orbital. Several delicate filaments enter the IOF and innervate the orbital periosteum.
• Palatine. The greater palatine nerve travels in the greater palatine foramen to the upper gingiva and hard palate. Lesser palatine nerve travels in the lesser palatine foramen to the soft palate, uvula, and tonsils. Posterior inferior nasal nerves arise from the greater palatine nerve, reach the nasal cavity via holes in the palatine bone, and innervate the inferior nasal concha.
• Posterior superior nasal. These branches are distributed to the septum and lateral wall of the nasal fossa. They traverse the sphenopalatine foramen to reach the nasal cavity and the innervate superior and middle nasal conchae and posterior septum. One branch, larger than the others, is the nasopalatine nerve, which passes across the roof of the nasal cavity and descends to the roof of the mouth via the incisive foramen.
• Pharyngeal. This branch travels with the pharyngeal branch of the internal maxillary artery and innervates the mucous membrane of the nasopharynx.
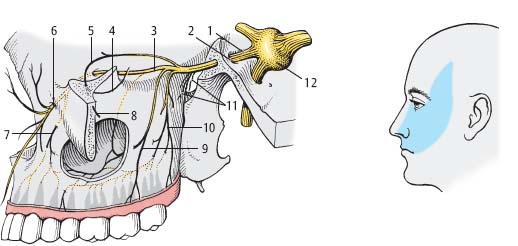
Fig. 5.4 Maxillary nerve (CN V2). (1, maxillary nerve; 2, foramen rotundum; 3, infraorbital nerve; 4, zygomaticotemporal nerve; 5, zygomaticofacial nerve; 6, infraorbital foramen; 7, anterior superior alveolar nerves; 8, zygomatic nerve; 9, middle superior alveolar nerve; 10, posterior superior alveolar nerves; 11, ganglionic branches [fine filaments running to the pterygopalatine ganglion]; 12, gasserian [trigeminal, semilunar] ganglion.)
Mandibular Division (CN V3) (Fig. 5.5)
• Sensory and motor.
• Largest of the three divisions.
• In Meckel’s cave, the sensory root of CN V3 lies inferior to V1 and V2 . and exits the skull via the foramen ovale. CN V3 does not enter the cavernous sinus (Fig. 5.2). Contents of foramen ovale: CN V3, lesser superficial petrosal nerve, emissary veins, and accessory meningeal artery. After CN V3 exits foramen ovale, it joins the motor root to form the mandibular nerve. The mandibular nerve lies in the infratemporal (zygomatic) fossa. where it divides into
1. Meningeal (recurrent) branch. Reenters foramen spinosum along with the middle meningeal artery to innervate the dura of the middle cranial fossa and the mucous lining of the mastoid air cells.
2. Medial pterygoid nerve. Small branch to the deep surface of the medial pterygoid muscle.
3. Masseteric nerve. Passes laterally to cross mandibular notch to the deep surface of the masseter muscle.
4. Deep temporal nerves. Enter the deep surface of the temporalis muscle.
5. Buccal nerve. Innervates the skin over the buccinator muscle (note: motor innervation to the buccinator is provided by buccal branches of CN VII).
6. Lateral pterygoid nerve. Enters the deep surface of the lateral pterygoid muscle.
7. Auriculotemporal nerve. Runs posterior to the neck of the mandible, then turns upward with the superficial temporal artery under the parotid gland, then ascends over the zygomatic arch. Branches include
• Anterior auricular. Innervate skin of the helix and tragus.
• Branches to the external acoustic meatus. Innervate skin of the external acoustic meatus and tympanic membrane.
• Articular branches. Innervate the temporomandibular joint.
• Superficial temporal branches. Accompany the superficial temporal artery to the vertex of the skull and innervate the skin of temporal region.
• Note that the auriculotemporal nerve conveys postganglionic parasympathetic fibers (from CN IX and the otic ganglion) to the parotid gland.
• The auriculotemporal nerve also interacts with CN VII via communicating branches.
8. Lingual nerve. Innervates the mucous membrane of the mouth and gums and anterior two thirds of the tongue (not taste, which is supplied by CN VII). It is joined by the chorda tympani nerve (branch of CN VII), which transmits taste from anterior two thirds of the tongue and provides parasympathetic secretomotor innervation to the submandibular ganglion. Passes between the medial pterygoid and ramus of mandible and crosses obliquely to reach the tongue.
9. Inferior alveolar nerve. Largest branch of the mandibular nerve. It descends adjacent to the ramus of the mandible to the mandibular foramen to enter the mandibular canal and gives off
• Dental branches innervating the mandibular molar and premolar teeth.
• Incisive branch innervating the mandibular canine and incisor teeth.
• Mental nerve, which emerges at the mentalforamen and innervates skin of chin and lower lip.
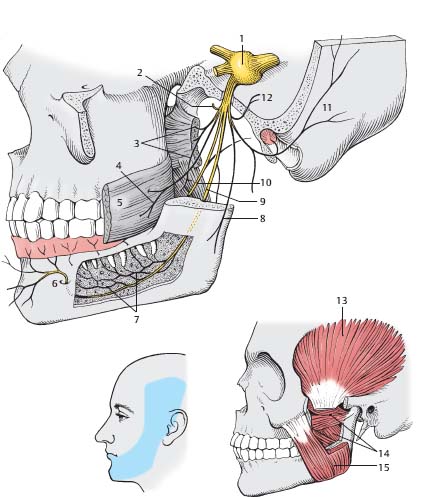
Fig. 5.5 Mandibular nerve (CN V3). (1, gasserian [trigeminal, semilunar] ganglion; 2, deep temporal nerves; 3, pterygoid nerves; 4, buccal nerve; 5, buccinator muscle; 6, mental foramen; 7, inferior dental branches of inferior alveolar nerve; 8, masseteric nerve; 9, inferior alveolar nerve; 10, lingual nerve; 11, auriculotemporal nerve; 12, recurrent meningeal branch; 13, temporalis muscle; 14, pterygoid muscles; 15, masseter muscle.)
• Motor fibers receive supranuclear input from corticobulbar fibers that originate in the lower one third of the precentral gyrus and traverse the corona radiata, internal capsule, and cerebral peduncle, and then decussate in the pons and terminate in the motor nucleus in the midpons, medial to the principal sensory nucleus of CN V.
• Motor nucleus of CN V (Fig. 5.1) sends a motor root that leaves the pons, passes forward in the cerebellopontine angle cistern, and pierces dura beneath the attachment of the tentorium to the petrous temporal bone, enters Meckel’s cave, travels immediately beneath the trigeminal sensory ganglion and exits the skull via foramen ovale. The motor root and sensory root of CN V3 then join to form the mandibular nerve.
• Motor component of the mandibular nerve gives branchial motor innervation to muscles of mastication:
 Masseter (zygomatic arch to angle of mandible, closes mouth)
Masseter (zygomatic arch to angle of mandible, closes mouth)
 Temporalis (coronoid process of mandible to temporal bone up to superior temporal line, closes mouth)
Temporalis (coronoid process of mandible to temporal bone up to superior temporal line, closes mouth)
 Medial pterygoid (medial aspect of lateral pterygoid plate to angle of mandible, closes mouth)
Medial pterygoid (medial aspect of lateral pterygoid plate to angle of mandible, closes mouth)
 Lateral pterygoid (lateral aspect of lateral pterygoid plate to top of mandible, opens mouth)
Lateral pterygoid (lateral aspect of lateral pterygoid plate to top of mandible, opens mouth)
 Tensor tympani (attached to malleus, involved in acoustic reflexes)
Tensor tympani (attached to malleus, involved in acoustic reflexes)
 Tensor veli palatini (eustachian tube cartilage to pterygoid hamulus to soft palate, involved in equalizing pressure in the middle ear)
Tensor veli palatini (eustachian tube cartilage to pterygoid hamulus to soft palate, involved in equalizing pressure in the middle ear)
 Mylohyoid
Mylohyoid
 Anterior belly of the digastric muscle
Anterior belly of the digastric muscle
Trigeminal Nerve: Normal Images (Figs. 5.6, 5.7, 5.8, 5.9, 5.10, 5.11)
Trigeminal Nerve Lesions
Evaluation
• Sensory evaluation. Somatic sensation (light touch, pain/temperature) tested on face and mucous membranes. Each of the three trigeminal divisions is tested and compared with the contralateral side. Lesions distal to the trigeminal ganglion result in sensory loss or paresthesias/dysesthesias confined to a single division. Lesions at or proximal to the ganglion result in sensory dysfunction over the whole ipsilateral face/forehead. The cutaneous area over the angle of the mandible is supplied by upper cervical roots (C-2/C-3) so a hemifacial sensory loss that spares the angle of the jaw makes anatomical sense. Dissociation of pain/temperature and light touch sensation on the face differentiates lesions affecting the spinal tract and nucleus of CN V from lesions affecting the principal sensory nucleus. It is important also to note that not all lesions result in complete sensory loss but rather may result in reduced sensation (hypesthesia), altered sensation (dysesthesia), abnormal sensation (paresthesia), or pain in the affected division.
• Motor evaluation. Test by having patient clench jaw (masseter, temporalis), open jaw, and move side to side against resistance (lateral pterygoids). Lesions of the motor nucleus or more distally result in lack of contraction of the ipsilateral masticatory muscles. When the mouth is opened, the jaw deviates to the paralyzed side (due to intact contralateral lateral pterygoid muscle). Other muscles innervated by CN V (e.g., mylohyoid, anterior belly of the digastric, tensor tympani, tensor veli palatini) are difficult to test individually.
• Reflex evaluation.
 Corneal reflex. Light touch to cornea leads to bilateral eyeblinks. Afferent arc is CN V1 from upper cornea or CN V2 from lower cornea to ipsilateral and contralateral CN VII motor nucleus. Efferent arc is CN VII to orbicularis oculi bilaterally for eyeblink.
Corneal reflex. Light touch to cornea leads to bilateral eyeblinks. Afferent arc is CN V1 from upper cornea or CN V2 from lower cornea to ipsilateral and contralateral CN VII motor nucleus. Efferent arc is CN VII to orbicularis oculi bilaterally for eyeblink.
 Jaw jerk reflex. Tapping the lower jaw leads to contraction of the masseter and temporalis muscles. Afferent arc is proprioceptive sensory fibers to mesencephalic nucleus of CN V. Efferent arc is motor nucleus of CN V to mandibular nerve to cause contraction of masseter and temporalis.
Jaw jerk reflex. Tapping the lower jaw leads to contraction of the masseter and temporalis muscles. Afferent arc is proprioceptive sensory fibers to mesencephalic nucleus of CN V. Efferent arc is motor nucleus of CN V to mandibular nerve to cause contraction of masseter and temporalis.

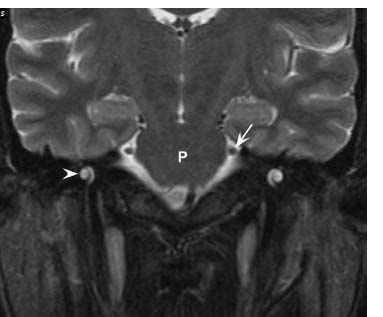
Fig. 5.7 Coronal T2-weighted image shows the cisternal segments of CN V (arrow) at the lateral aspect of the midpons (P). The more inferolateral cochlea (arrowhead) is well seen on this image.
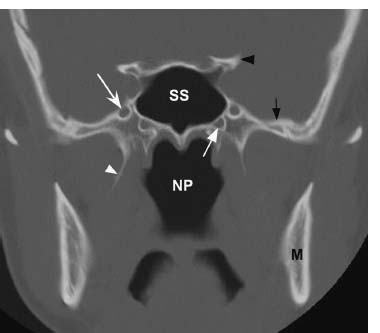
Fig. 5.8 Coronal CT image in bone window at the level of the midsphenoid sinus (SS) and nasopharynx (NP) shows the normal foramen rotundum (white concave arrow), the opening through which CN V2 exits the skull base. Note that the vidian (pterygoid) canal (white straight arrow) is located inferior and medial to the foramen rotundum. The right lateral pterygoid plate (white arrowhead), left clinoid process (black arrowhead, left mandible (M) and greater wing of the left sphenoid bone (black arrow) are also indicated.

Fig. 5.9 A more posterior coronal CT image in bone window shows the normal foramen ovale (arrow), the opening through which CN V3 exits the skull base.
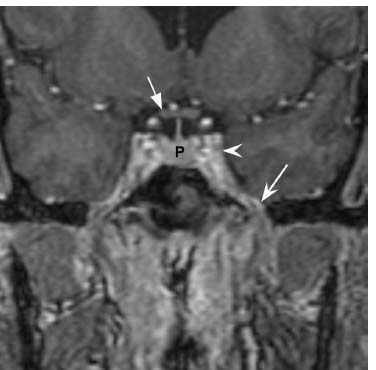
Fig. 5.10 Coronal postcontrast T1-weighted gradient-echo image in a different patient but at a similar plane as Fig. 5.8 shows the normal appearance of foramen ovale (concave arrow) and the cavernous sinus (arrowhead). The foramen ovale can typically be identified on the same coronal image as the optic chiasm (straight arrow) and pituitary gland (P).
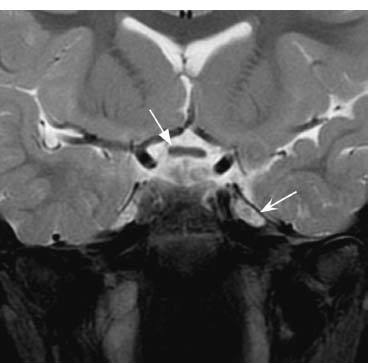
Fig. 5.11 Coronal T2-weighted image with fat saturation slightly more posteriorly shows the normal CSF-intensity signal within Meckel’s cave (concave arrow). The optic chiasm (straight arrow) is also indicated.
Types
Supranuclear Lesions
• Bilateral but predominantly contralateral control of muscles of mastication via corticobulbar fibers.
• Unilateral upper motor neuron lesions can interrupt the corticobulbar pathway from the motor cortex to pons. Because the jaw then deviates toward the paralyzed side (see above), it deviates away from the lesion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree