Study
Sample size
Transducer/US system
TrP ultrasound appearance
Sikdar et al. [27]
9
Linear array12–5 MHz (Philip iU22 clinical US system with L12–5 transducer)
“Focal hypoechoic (darker) areas with heterogeneous echotexture”
Ballyns et al. [25]
44
Linear array12–5 MHz (Philip iU22 clinical US system with L12–5 transducer)
“Typically, trigger points appear as focal hypoechoic (darker) areas with a heterogeneous echo texture”
Niraj et al. [30]
10
High-resolution linear array 12–7 MHz (Sonosite S-Nerve US system)
“Mixed echoic area”
Trapezius Muscle
The trapezius muscle is composed of three main parts: upper, middle, and lower [31]. Each part has a different function and fiber direction. The trapezius is innervated by cranial nerve XI (accessory nerve) and by C2–C4 cervical nerves. The function of the upper trapezius is to rotate the clavicle at the sternoclavicular joint, move the scapula obliquely upward, and rotate the glenoid cavity inferiorly. The middle trapezius retracts the scapula medially. The lower trapezius stabilizes the scapula and moves it medially and downward. According to Travell and Simons, trigger points in the upper trapezius are activated by everyday activities that involve sustained elevation of the shoulders such as painting, playing a musical instrument, holding a telephone without elbow support, and typing on a computer without armrests [2]. Other events that can also lead to generation of trapezius trigger points include whiplash, tight bra straps, heavy over the shoulder bags, or trauma. Travell and Simmons identified six trigger points in the trapezius muscle [2]. Two are located in the upper part, two in the middle part, and two in the lower part. The trigger points in the superior part refer pain over the posterior aspect of the neck and along the temporal and periarticular areas. The trigger points in the middle trapezius refer pain along the paraspinal area. In the inferior trapezius, pain is referred over the mastoid, behind the neck, and between the scapula.
Scanning Techniques and Anatomy to Identify: Upper Trapezius
The superior fibers of the trapezius originate at the occipital bone and cervical spinous processes via the nuchal ligament and insert on the lateral third of the clavicle forming the anterior margin of the trapezius. The fibers of anterior margin of the trapezius run obliquely inferior and lateral towards the posterior border of the lateral third of the clavicle [31]. Deep to the anterior margin is the supraclavicular fossa. This region is dangerous to inject due to the presence of many important life-sustaining nerves, vessels, and viscera. In the supraclavicular fossa are the subclavian artery and vein, brachial plexus, phrenic nerve, and apex of the lung.
With the patient either seated or prone, identify the trigger point by palpation. Place the probe along the posterior portion of the upper trapezius. Scan over the trigger point and identify it by US. The most superficial layer of muscle is the trapezius. When injecting the superior trap, the trajectory of the needle is dependent on the location. If along the far lateral region, a posterior to anterior trajectory will avoid the supraclavicular fossa entirely. If injecting more medially, a flat medial to lateral trajectory will avoid all other structures unless a long needle is used. Use the Doppler to identify any veins or arteries. Ribs, clavicle, and scapula are easily identifiable as hyperechoic.
Scanning Techniques and Anatomy to Identify: Middle Trapezius
The middle fibers of the trapezius originate from the aponeurosis at the level of the T1–T4 spinous processes and insert onto the acromion and the scapular spine. The middle trapezius can be divided into the lateral (scapular) region and the medial (rhomboid) region.
The lateral region is defined by scapula being deep to the trapezius. With the ultrasound probe parallel and superior to the scapular spine, the layers of tissue from superficial to deep are skin/subcutaneous fat, trapezius muscle, supraspinatus muscle, and the blade of scapula. The only vessels and nerve to be concerned with are the suprascapular artery, vein, and nerve as they pass through the suprascapular notch. This region is safer for injection since the lung is protected by the scapula (Fig. 8.1).
The medial region lies between the medial border of the scapula and the T1–T4 spinous processes. With the ultrasound probe oriented either transverse or longitudinal to the fibers of the trapezius, the layers of tissue of superficial to deep are the subcutaneous fat, trapezius muscle, rhomboid minor or levator scapulae, serratus posterior superior, erector spinae muscles, and ribs. The spinal accessory nerve (SAN) runs deep to the trapezius but superficial to the rhomboids and levator scapulae. The SAN runs inferior parallel to the spinous processes and medial to the medial border of the scapula. The SAN can be identified by turning on the Doppler and locating the superior branch of the transverse cervical artery and veins which run adjacent to the SAN. The SAN is about 1 mm in diameter and is monofascicular by ultrasound [32]. Deep to the rhomboids and levator scapulae but superficial to the serratus posterior superior and erector spinae muscle run the dorsal scapular nerve and the deep branch of the transverse cervical artery (Dorsal scapular artery) along the medial border of the scapula. Risk of pneumothorax is small due to thickness of the musculature in this region. Nonetheless, the ribs are easily identified by US as hyperechoic.
Scanning Techniques and Anatomy to Identify: Lower Trapezius
The lower fibers of the trapezius originate from the T5 to T12 spinous processes and insert onto the inferior portion of scapular spine. Similar to the middle trapezius, the lower trapezius can be divided into a lateral and medial region.
The lateral region is defined by the presence of the scapula deep to all tissues. This region occupies a small area inferior to the scapular spine. Place the US probe parallel and inferior to the scapular spine. The layers of tissue from superficial to the deep are the subcutaneous fat, the trapezius, the infraspinatus, and the blade of the scapula. Again, much like the lateral region of the middle trapezius, this region is safe to inject, as there are no major nerves or vessels and the scapula protects the lung.
The medial region spans quite a distance from T5 to T12. In the majority of this region, the rhomboid major muscle lies deep to the trapezius except in the more inferior portion where the erector spinae or the latissimus dorsi may lie deep. The SAN and associated vessels are less easily identified, as this is where they terminate.
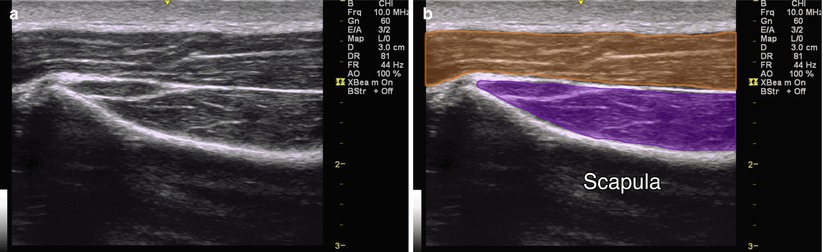
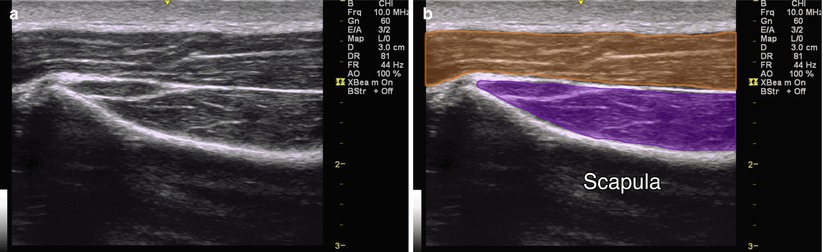
Fig. 8.1
(a) Coronal view of upper trapezius muscle. (b) Orange indicates trapezius muscle, purple indicates supraspinatus muscle, scapula labeled
Injection Technique: In-Plane Longitudinal Approach
Patient positioning: The patient should lie in the prone position for the lower and middle trapezius and either prone or seated for the upper trapezius.
Probe positioning: Place the probe over the trigger point either transverse or longitudinal to the muscle fibers (Fig. 8.2a).
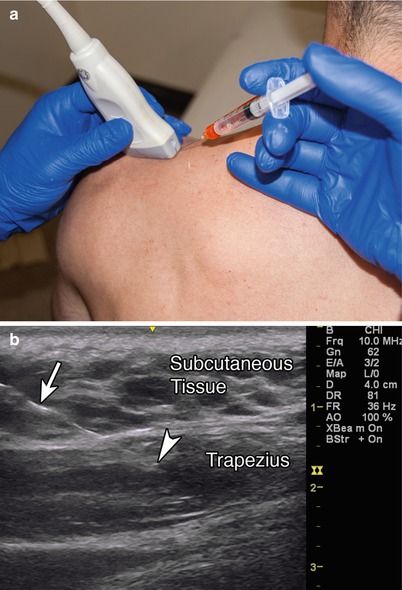
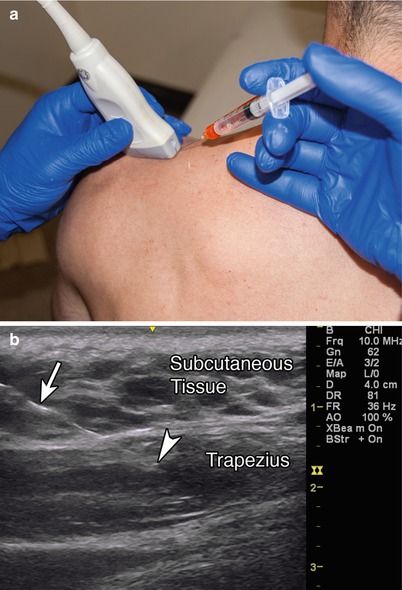
Fig. 8.2
(a) Example of coronal probe position over upper trapezius muscle with in-plane needle position. (b) Example of in-plane approach, arrowhead indicates needle tip, arrow indicates needle, subcutaneous tissue and trapezius labeled
Markings: When injecting the superior trapezius, use the color Doppler to identify the subclavian artery and vein in the supraclavicular fossa and the superficial branch of the transverse cervical artery, which lies in the fascia deep to the medial trapezius and superficial to all other musculature. The apex of the lung is approximately 2.5 cm above the medial third of the clavicle at the level of the anterior border of the SCM [31].
Needle position: The needle should be inserted parallel to the transducer for optimal visualization, with simultaneous injection of local anesthetic.
Safety considerations: There is a risk of the following: prolonged bleeding, infection, allergic reaction, increased pain and spasm, decreased functional scores, and pneumothorax.
Pearls:
Avoid pneumothorax by identifying the hyperechoic ribs and pleura between the individual ribs.
Use Doppler to identify vessels to avoid intravascular injection.
If the taut band rolls under the needle, anchor the trigger point along its length with fingers or thumb to prevent rolling.
If a referred pain pattern and local twitch response were elicited prior to injection, then once the needle enters the trigger point they should occur again.
Postinjection it is important to have the patient actively stretch each muscle injected through its full range of motion.
Equipment needed:
High-frequency linear array transducer (10 MHz+)
25G 1.5″ needle
1–3 ml local anesthetic
Scalenus Anterior
The muscles that lie directly lateral to the cervical vertebral column are the scalenes. In total there are four scalenus muscles: anterior, medius, posterior, and minimus. Trigger points in the scalenes can cause shoulder, back, or arm pain. These trigger points can be activated by pulling, lifting, coughing, musculoskeletal asymmetry, or anything that causes a disturbance in gait [4]. Contraction of the anterior and middle scalene elevates the first rib and flexes the head ipsilaterally. Activation of the posterior scalene elevates the second rib and flexes the neck ipsilaterally. These muscles also assist during respiration. They are innervated by branches off of the anterior cervical rami (C2–C8). Trigger points of the scalenes refer pain to the anterior chest, the ipsilateral upper limb, and the medial border of the scapula [4].
Scanning Techniques and Anatomy to Identify
Scalenus anterior is formed by multiple musculotendinous fascicles that originate from the anterior tubercles of the transverse processes of C3 to C6 and blend together and insert onto the scalene tubercle of the 1st rib. Place the patient supine with his neck supported and head rotated to the contralateral side about 20°. Place the transducer axially, along the posterior margin of the SCM about midway between the mastoid process and clavicle. The anterior scalene is the muscular belly just posterior to the SCM. Medial to the anterior scalene is the carotid space including the internal jugular vein, common carotid artery, and vagus nerve. At this level the carotid space lies deep to the SCM and thus easily avoided. Anterior to the scalene is the phrenic nerve, and posterior is the brachial plexus and subclavian artery and vein (Fig. 8.3).
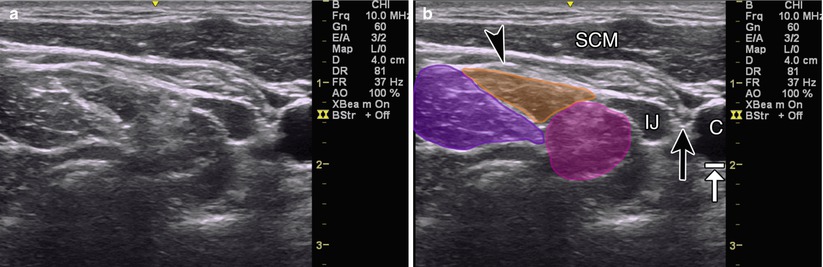
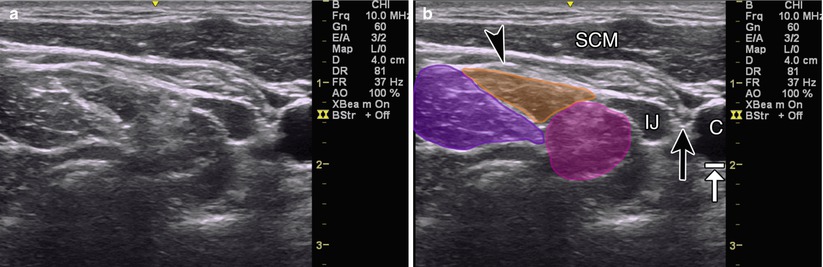
Fig. 8.3
(a) Axial view of scalene muscles. (b) Purple indicates posterior scalene, orange indicates middle scalene, magenta indicates anterior scalene, black arrow indicates vagus nerve, black arrowhead indicates phrenic nerve, SCM sternocleidomastoid muscle, IJ internal jugular vein, C carotid artery, white arrow with stop also indicates carotid artery
Injection Technique: In-Plane Axial Approach
Patient positioning: Place the patient supine with his neck supported and head rotated to the contralateral side about 20°.
Probe positioning: Place the probe in the axial plane along the posterior margin of the sternocleidomastoid muscle (Fig. 8.4a).
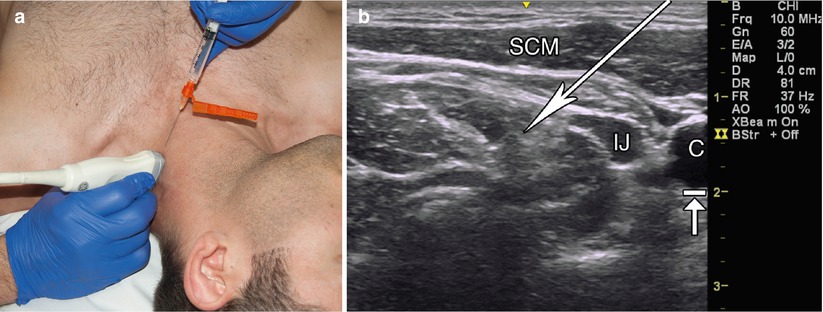
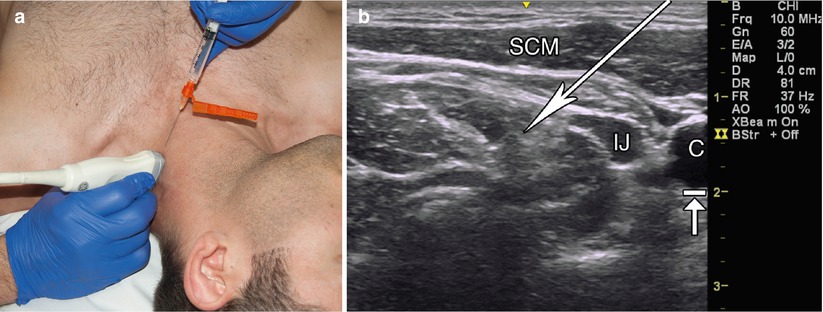
Fig. 8.4
(a) Example of probe position over the anterior scalene. (b) Example of in-plane axial approach, long white arrow indicates trajectory into the anterior scalene, SCM sternocleidomastoid muscle, C carotid artery, IJ internal jugular vein, arrow with stop also indicating carotid artery
Markings: Use color Doppler to identify the internal carotid, internal jugular, subclavian artery/vein, and external carotid artery.
Needle position: The needle should be inserted parallel to the transducer for optimal visualization, with simultaneous injection of local anesthetic.
Safety considerations:
Brachial plexus palsy: Torriani in 2009 reported 33 % incidence of brachial plexus palsy while performing US-guided anterior scalene injections with bupivacaine for thoracic outlet syndrome management [33]. In a similar study with botulinum toxin, Torriani (2010) reported no incidence of brachial plexus palsy [34]. As this evidence suggests, to avoid unintended nerve blocks in this region, it is best to use botulinum toxin.
Phrenic nerve palsy: The incidence of phrenic nerve palsy for interscalene block is reported as high as 100 % in several studies [35]. Using high-resolution ultrasonography, Kessler reports that the phrenic nerve is monofascicular with a mean diameter of 0.76 mm and was identifiable in 93.5 % of 23 volunteers [36].
Pearls:
Injections of the anterior scalene should be performed with botulinum toxin since injections with local anesthetic are likely to lead to temporary brachial plexus or phrenic nerve palsy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








