In children, tumors of the spine are much rarer than intracranial tumors. They are classified into intramedullary, intradural-extramedullary, and extradural tumors. Magnetic resonance imaging provides crucial information regarding the extent, location, and internal structure of the mass, thus critically narrowing the differential diagnosis and guiding surgery.
In children, tumors of the spine are much rarer than intracranial tumors (approximately 1:10). They are classified into intramedullary, intradural-extramedullary, and extradural tumors. In our experience, extradural tumors account for about two thirds of cases, intramedullary tumors for one fourth, and intradural-extramedullary tumors for the remainder.
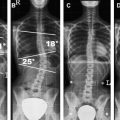
Because of an aspecific clinical presentation, most children are initially imaged with conventional x-rays. Intradural (intra- and extramedullary) tumors cause enlargement of the spinal canal and vertebral scalloping, but these signs are not early indicators of the underlying disease. Conversely, extradural tumors usually produce more evident involvement of bone already in the early stages. Magnetic resonance (MR) imaging provides crucial information regarding the extent, location, and internal structure of the mass, thus critically narrowing the differential diagnosis and guiding surgery . The MR imaging technique ideally includes the use of phased-array surface coils and must include unenhanced sagittal T1- and T2-weighted images and contrast-enhanced T1-weighted images in all three planes of space; axial T2-weighted images are used to detect spinal cord compression from extrinsic tumors. Computerized tomography (CT) plays an important role in the assessment of bone tumors and in detecting calcifications; spiral volumetric acquisitions improve the quality of multiplanar reformatting. The clinical role of advanced MR imaging modalities, including MR spectroscopy, diffusion-weighted imaging, diffusion tensor imaging, and functional MR imaging, has not been extensively researched.
Intramedullary tumors
Intramedullary tumors account for 4% to 10% of all primary central nervous system (CNS) neoplasms and for 25% of pediatric spinal tumors . They prevail in children between 1 and 5 years of age without gender prevalence. Astrocytomas are the most common intramedullary tumor in the pediatric age group (82% of cases) , followed by gangliogliomas. Ependymomas are uncommon in children outside the setting of neurofibromatosis Type 2.
The presentation, duration, and course of the disease may be variable. Affected patients may have a prolonged duration of symptoms before a diagnosis is established. Symptoms may be elicited by trauma or efforts. Back pain is often the earliest and most persistent complaint and should prompt to MR imaging to rule out intraspinal pathology. Rigidity and contracture of the paravertebral muscles may result from thecal sac enlargement, involvement of adjacent bone, and impaired of cerebrospinal fluid (CSF) dynamics. Progressive scoliosis may cause delays in the diagnosis if underestimated. Head tilt and torticollis and lower cranial nerve palsies with dysphagia, dyspnea, and dysphonia may represent early signs of cervico-medullary neoplasms due to involvement of the spinal roots of the accessory nerve innervating the trapezius and sternocleidomastoid muscles. Sensorimotor disturbances generally occur later in the course of disease and may be difficult to evaluate, especially in small children. Long-lasting weakness and spinal or limb muscle atrophy may be found with slowly growing tumors . Hydrocephalus with raised intracranial pressure may rarely represent the clinical presentation of intramedullary tumors and is caused by obstruction of the spinal subarachnoid spaces, CSF seeding, or increased CSF protein content .
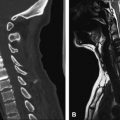
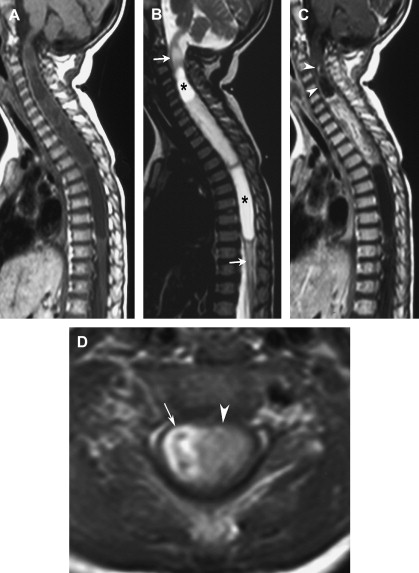
On MR imaging, intramedullary neoplasms produce enlargement of the spinal cord, giving heterogeneous signal intensity. They may be solid or associated with neoplastic or non-neoplastic cysts. Neoplastic cysts are located within the tumor mass, result from necrosis and degeneration, show peripheral enhancement on gadolinium-enhanced sequences, and must be removed surgically. Non-neoplastic cysts are located at the cranial and caudal poles of the tumor, result from reactive dilatation of the central canal due to tumor fluid secretion or mechanical blockage of the ependymal canal, have unenhancing margins, and can be drained and aspirated but not resected . Swelling of the spinal cord cranial and caudad to the tumor can result from edema. Discrimination of tumor from nonneoplastic areas such as polar cysts and edema is crucial for surgical planning.
Astrocytoma
In the pediatric age group, astrocytomas account for the vast majority of intrinsic spinal cord neoplasms, with most tumors being low grade (ie, pilocytic and fibrillary) . In our experience, pilocytic astrocytomas account for 75% of all intramedullary tumors in the pediatric age group and typically affect children between 1 and 5 years of age, whereas fibrillary astrocytomas account for 7% and tend to occur in older children (around 10 years of age) .
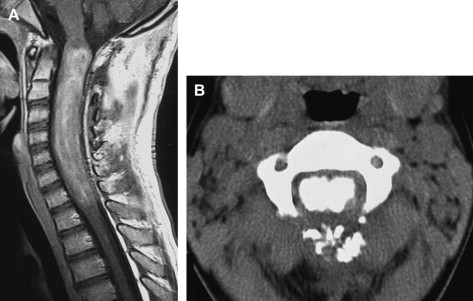
On MR imaging, pilocytic astrocytomas are characterized by enlargement of the spinal cord within a widened spinal canal. They frequently involve a large portion of the cord, spanning multiple vertebral levels in length. True “holocord” tumors are rare; in most cases, involvement of the whole length of the spinal cord is caused by extensive spinal cord edema rather than by a tumor. The cervico-medullary junction and the cervico-thoracic cord are the most common locations. Tumors can show areas of necrotic-cystic degeneration (60% of cases), can have a “cyst with mural nodule” appearance ( Fig. 1 ), or can be structurally solid (about 40% of cases) ( Fig. 2 ). The solid components are iso- to hypointense on T1-weighted images and hyperintense on T2-weighted images, whereas necrotic-cystic components display higher relaxation times on T1- and T2-weighted images. Some degree of contrast enhancement is present in the majority of spinal cord pilocytic astrocytomas. The pattern of enhancement is variable and does not define tumor margins .
Ganglioglioma
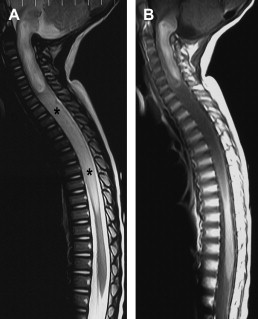
Gangliogliomas are the second most common intramedullary tumor in the pediatric age group (15% of cases) and mostly affect children between 1 and 5 years of age, as do pilocytic astrocytomas Although they typically are low-grade tumors (Grade I-II) with a low potential for malignant degeneration, they have a significant propensity for local recurrence , and the glial element may progress to high grade. Their preferential location is in the cervical and upper thoracic cord with extension to the medulla through the foramen magnum. Holocord involvement has been described to be more frequent than in other spinal cord tumors, probably as a result of low growth rate , but we have not had similar results . Although propensity for cyst formation has been reported to be common , all gangliogliomas in our series were predominantly solid .
On imaging, calcification is probably the single most suggestive feature of gangliogliomas ( Fig. 3 ) . In the absence of gross calcification, the MR imaging appearance of gangliogliomas is nonspecific and does not allow differentiation from astrocytomas. Solid portions have mixed iso-hypointensity on T1-weighted images and heterogeneous iso-hyperintensity on T2-weighted images . Perifocal edema can vary from limited or absent to extensive ( Fig. 4 ). Contrast enhancement can be focal or patchy, and it rarely involves the whole tumor mass; absence of enhancement has also been described in a minority of cases .
Ependymoma
Spinal cord ependymomas are virtually nonexistent in the pediatric age group outside the setting of neurofibromatosis Type 2. While they may extend over large portions of the cord, most neurofibromatosis Type 2–related ependymomas are small intramedullary nodules that may be multiple. These markedly vascularized tumors frequently show intralesional hemorrhages, which constitute their hallmark also on neuroimaging, producing the so-called “cap sign,” a T2 hypointense rim surrounding the cranial or caudal poles of the lesion that results from magnetic susceptibility effects .
Intradural-extramedullary tumors
In the pediatric age group, most intradural-extramedullary tumors are leptomeningeal metastases from primary brain tumors. Primitive tumors in this location are the least common among spinal tumors and are mostly represented by schwannomas and neurofibromas in neurofibromatosis patients. A host of other neoplasms, including filar ependymomas, meningiomas, and atypical teratoid rhabdoid tumors, can be found in this location. Other lesions include dysontogenetic masses and other non-neoplastic masses. Clinical features are represented by pain and signs of cord or nerve root compression, depending on the location of the mass. Only primitive intradural-extramedullary tumors are discussed in this article.
Myxopapillary ependymoma
Myxopapillary ependymomas account for 13% of all spinal ependymomas in the general population; however, they are more frequent in the pediatric age group. They are thought to arise from the ependymal glia of the filum terminale and typically present as intradural extramedullary lesions involving the lumbar and sacral canal . Rarely, myxopapillary ependymomas involve the sacrococcygeal region, arising from vestiges at the distal portion of the neural tube . Affected patients present with lower back, leg, or sacral pain; weakness or sphincter dysfunction ; and occasionally subarachnoid hemorrhage .
On MR imaging, the lesion is iso- to hyperintense on T1-weighted images and hyperintense on T2-weighted images. Contrast enhancement is moderate to marked and may be inhomogeneous. It is not uncommon for large masses to envelope or infiltrate the outer surface of the conus medullaris ( Fig. 5 ). Large masses may extend into the neural foramina, expand the spinal canal, and erode the adjacent vertebrae . The main differential diagnosis is with nerve sheath tumors, such as schwannomas.
Nerve sheath tumors
Schwannomas
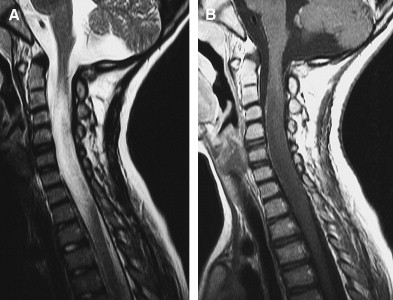
Schwannomas, or neurinomas, originate from Schwann cells in the sheaths of spinal root and nerves and grow extrinsically with respect to the axon. They are separated from the adjacent tissues by a thin capsule, which facilitates surgical removal. Isolated spinal schwannomas are rare in the pediatric population, whereas multiple schwannomas in the setting of neurofibromatosis Type 2 are more frequent. They may be intradural, extradural, or both, depending on where they originate along the course of the spinal root; however, intradural tumors are more common. Within the lumbar thecal sac, they may attain a considerable size before becoming clinically manifest, causing enlargement of the spinal canal, scalloping, and bone erosion. On MR imaging, schwannomas are iso- to hypointense on T1-weighted images and iso- to hyperintense in T2-weighted images. Contrast enhancement is moderate to marked and essentially homogeneous ( Fig. 6 ).
Neurofibromas
Neurofibromas are composed of an admixture of Schwann cells and fibroblasts and tend to infiltrate, rather than dislocate, the root or nerve from which they originate. Therefore, radical surgery is usually much more difficult to attain than with schwannomas. Neurofibromas are typically found in patients with neurofibromatosis type 1. They may be solitary or multiple ( Fig. 7 ) and may resemble a string of beads when they affect multiple nerve roots in the thecal sac. On MR imaging, their behavior is similar to that of schwannomas, with iso- to hypointensity on T1-weighted images, hyperintensity on T2-weighted images, and marked contrast enhancement.
Meningioma
Meningiomas are uncommon tumors in the pediatric age group outside the setting of neurofibromatosis type 2. Isolated spinal meningiomas typically belong to a particular histologic variant called “clear cell meningioma.” Clear cell meningiomas are typical of younger patients, are prevailingly located in the spinal canal and cerebellopontine angle, and show a more aggressive behavior with higher recurrence rate and propensity for leptomeningeal dissemination than adult subtypes .
On MR imaging, clear cell meningiomas are round to ovoid, well demarcated masses that are isointense to the spinal cord on T1- and T2-weighted images. Contrast enhancement is moderate to marked and homogeneous ( Fig. 8 ). As with conventional meningiomas, the presence of a dural tail sign is not mandatory .
Atypical teratoid rhabdoid tumor
Atypical teratoid rhabdoid tumors (ATRT) are highly malignant neoplasms that are ubiquitous in the CNS. Although most affect the brain, they may primitively involve the spine . Owing to their marked aggressiveness, primitively extra-axial lesions may infiltrate the spinal cord and vice versa, so that the origin of the tumor may be difficult to assess on neuroimaging. ATRTs predominate in the first 2 years of life and may be congenital.
Neuroimaging features ( Fig. 9 ) are similar to those of intracranial ATRTs . These tumors are structurally heterogeneous due to often extensive hemorrhage and necrotic-cystic change. Solid portions are hypointense on T1- and T2-weighted images due to marked cellularity with high nuclear-to-cytoplasmatic ratio. Contrast enhancement is inhomogenous. MR imaging of the whole neuraxis must be performed to identify possible secondary spread or multicentric disease.
Primitive neuroectodermal tumors
Primitive neuroectodermal tumors (PNETs) are composed by undifferentiated or poorly differentiated cells and belong to a category of infantile, aggressive neoplasms, including neuroblastomas and Ewing sarcomas, which are characterized histologically by a monotonous hypercellularity composed by small, round cells with hyperchromatic nucleus and scant cytoplasm . Intraspinal PNETs are rare and more often occur in older children than in intracranial PNETs .
Neuroimaging features of intraspinal PNETs are nonspecific. Our experience is that of a single case originating from an intradural-extramedullary location in the cervical spine and causing spinal compression ( Fig. 10 ). This lesion was isointense with the spinal cord on T1- and T2-weighted images and enhanced homogeneously.
Dysontogenetic and non-neoplastic masses
(Epi)dermoids
Dermoids account for 10% of all spinal tumors in the pediatric age group and are often associated with dermal sinuses ; they may be primitive or iatrogenic (ie, secondary to inadvertent inclusion of skin debris during surgical interventions, such as myelomeningocele repair). Epidermoids are relatively infrequent in the pediatric age group.
Structurally, dermoids have a cystic structure lined by squamous epithelium containing dermal appendages (eg, hair, sweat glands, and sebaceous glands), whereas epidermoids are lined by squamous epithelium lacking cutaneous appendages. The fluid within both lesions contains cutaneous debris with variable concentrations of keratin, whose accumulation causes them to enlarge slowly. Complications include abscess formation and rupture of the cyst into the subarachnoid spaces, causing chemical meningitis.
(Epi)dermoids may be difficult to identify on conventional MR imaging because their signal intensity is similar to that of CSF ( Fig. 11 ). Proton-density and fluid attenuated inversion recovery (FLAIR) sequences are usually more sensitive than T1- or T2-weighted images. Diffusion-weighted imaging is useful, showing restricted diffusion within the cyst. Contrast enhancement is usually absent, except in case of superinfection.
Neurenteric cysts
Neurenteric cysts have a congenital origin from remnants of the primitive streak during early embryonic development. They are lined with a mucin-secreting, cuboidal or columnar epithelium that resembles the alimentary tract . Their content is variable, and the chemical composition may be similar to CSF, which is reflected into a variable pattern of signal intensity on MR imaging. They are more frequently located in the cervicothoracic spine anterior to the cord.
Arachnoid cysts
Arachnoid cysts are CSF collections housed within a splitting of the arachnoid membrane that do not communicate with the subarachnoid space. In the spine, arachnoid cysts may be located in the subdural or, less often, in the epidural space dorsal to the cord. They may be congenital or may result from adhesions provoked by previous infection or trauma. As such, they may complicate surgery for spinal dysraphism and may cause subsequent neurologic deterioration with signs of cord tethering. On MR imaging, the signal intensity of arachnoid cysts parallels that of CSF in all sequences. Some arachnoid cysts may contain proteinaceous fluid or blood, thereby resulting in increased T1 and T2 relaxation times, which may pose diagnostic problems. They may cause enlargement of the spinal canal and mild compression of the posterior aspect of the cord. Cine-MR imaging is useful to demonstrate exclusion of the cyst from the surrounding subarachnoid spaces and to monitor surgical results.
Intradural-extramedullary tumors
In the pediatric age group, most intradural-extramedullary tumors are leptomeningeal metastases from primary brain tumors. Primitive tumors in this location are the least common among spinal tumors and are mostly represented by schwannomas and neurofibromas in neurofibromatosis patients. A host of other neoplasms, including filar ependymomas, meningiomas, and atypical teratoid rhabdoid tumors, can be found in this location. Other lesions include dysontogenetic masses and other non-neoplastic masses. Clinical features are represented by pain and signs of cord or nerve root compression, depending on the location of the mass. Only primitive intradural-extramedullary tumors are discussed in this article.
Myxopapillary ependymoma
Myxopapillary ependymomas account for 13% of all spinal ependymomas in the general population; however, they are more frequent in the pediatric age group. They are thought to arise from the ependymal glia of the filum terminale and typically present as intradural extramedullary lesions involving the lumbar and sacral canal . Rarely, myxopapillary ependymomas involve the sacrococcygeal region, arising from vestiges at the distal portion of the neural tube . Affected patients present with lower back, leg, or sacral pain; weakness or sphincter dysfunction ; and occasionally subarachnoid hemorrhage .
On MR imaging, the lesion is iso- to hyperintense on T1-weighted images and hyperintense on T2-weighted images. Contrast enhancement is moderate to marked and may be inhomogeneous. It is not uncommon for large masses to envelope or infiltrate the outer surface of the conus medullaris ( Fig. 5 ). Large masses may extend into the neural foramina, expand the spinal canal, and erode the adjacent vertebrae . The main differential diagnosis is with nerve sheath tumors, such as schwannomas.