TUMORS OF THE SUBLINGUAL GLAND AND SPACE AND TUMORLIKE AND INFLAMMATORY CONDITIONS
KEY POINTS
- Computed tomography and magnetic resonance imaging can help to determine whether a submucosal mass presenting in the floor of the mouth or suprahyoid neck is of intrinsic or extrinsic origin to the sublingual gland or sublingual space.
- If a primary sublingual neoplasm is identified, imaging will help to establish its local extent, including its relationships to the mylohyoid muscle and mandible.
- Computed tomography and magnetic resonance imaging may be used for surveillance imaging following treatment for sublingual gland tumors.
There is an unavoidable overlap between the conditions discussed in this chapter and in those considering oral cavity pathology since the sublingual space (SLS) is an important component of the floor of the mouth. This chapter will discuss both problem-based and etiologic framework disease that may originate or primarily affect the sublingual gland (SLG) and/or space.
INTRODUCTION
A Dilemma: Sublingual Gland and Space Mass of Glandular or Nonglandular Origin
Mass lesions in the SLG region may be intrinsic or extrinsic to the SLG. Infiltrating systemic disease such as sarcoidosis, manifestations of autoimmune sialoadenitis, and rarely lymphoma can mimic an SLG epithelial-origin tumor if those conditions are not otherwise known to be present (Fig. 183.1). Diagnostic imaging may have a significant impact on sorting out these possibilities and thereby alter medical decision making. The contributions are equally important in some cases of intrinsic glandular epithelial-origin neoplasms.
Sublingual Gland Tumors
Major salivary glands contain several different groups of functioning and support cells that lead to the variety of possible histologic diagnoses that were discussed in Chapter 22. Precise histologic diagnosis by frozen section and needle biopsy may be difficult, especially with regard to distinguishing between benign and malignant neoplasms. Those planning care must be very aware of this limitation. Imaging features can sometimes help to anticipate malignancies. The main problem is that benign-appearing masses may be malignant and malignant-appearing masses are sometimes histologically benign. Because of this dilemma, both benign and malignant tumors are discussed in this chapter along with some of their more common potential mimics. However, predicting in advance whether a mass is benign or malignant most often does not alter the initial, usually surgical, approach to care (Figs. 183.2 and 183.3).
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
The development of the SLG is such that tumors may arise within contiguous accessory tissue that extends far anteriorly in the SLS, where it may then be contiguous with submandibular gland (SMG) salivary tissue in the submandibular space (SMS) via anatomic defects in the anterior aspect of the mylohyoid muscle. Similar contiguity of the SLG with the SMG may occur over the back edge of the mylohyoid muscle.
Applied Anatomy
The anatomic relationships important to medical decision making in SLG and SLS disease are reviewed in more detail in Chapter 175 and summarized here. That anatomy includes the following:
- Relationships of the SLG to other structures in and around the floor of the mouth, including the mandible, mylohyoid muscle, genioglossus and hyoglossus muscles, and the deep portion of the SMG
- Relationship of the SLS and SMS and adjacent parapharyngeal space
- Anatomy of the lingual and hypoglossal nerves within the floor of the mouth and more proximally
- Sublingual and level 1 lymph node drainage patterns (Chapters 149 and 157)
IMAGING APPROACH
Techniques and Relevant Aspects
Computed Tomography and Magnetic Resonance Imaging
Specific computed tomography (CT) protocols for various indications appear in Appendix A and are discussed in more detail in Chapters 175 and 182.
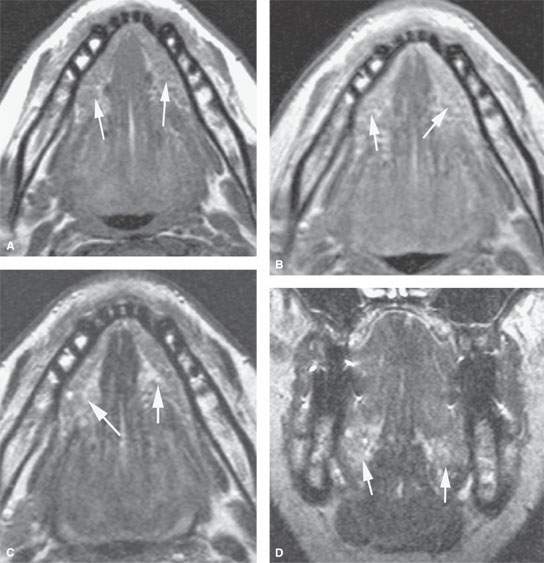
FIGURE 183.1. Magnetic resonance (MR) study of a patient with bilateral sublingual space swelling shown on MR to be due to sialoadenitis and subsequently shown to be due to autoimmune disease. The arrows point out the bilaterally enlarged submandibular glands in all images. T1-weighted (T1W) image without contrast (A) and a T1W image with contrast (B) showing more than the usual amount of enhancement within the sublingual glands. The T2-weighted (T2W) image in (C) shows no clearly demonstrable difference between normal glands and these abnormally inflamed glands. This is also true on the T2W coronal image in (D), which only suggests that the glands are somewhat enlarged and perhaps slightly more intense than usual.
Specific magnetic resonance (MR) protocols for various indications appear in Appendix B and are discussed in more detail in Chapters 175 and 182.
Diffusion-weighted imaging (DWI) may be obtained since it may contribute information about the likely benign or malignant nature of the mass; however, it is unlikely that any serious clinical decision will be based on such data relative to that from the clinical setting, anatomic imaging, and biopsy.
Since it is not predictable when contrast might be useful, a magnetic resonance imaging (MRI) study of the SLG and SLS is generally done with acquisitions before and after contrast injection. Contrast-enhanced MR studies are clearly useful when there are associated neuropathies that must be evaluated, if the lesion is aggressive, and/or if the cervical nodes are to be evaluated.
Ultrasound
Standard scanning techniques as described in Chapter 4 are used.
Radionuclide Studies
Radionuclide studies are not used routinely for the evaluation of salivary gland masses. The reasons are discussed subsequently.
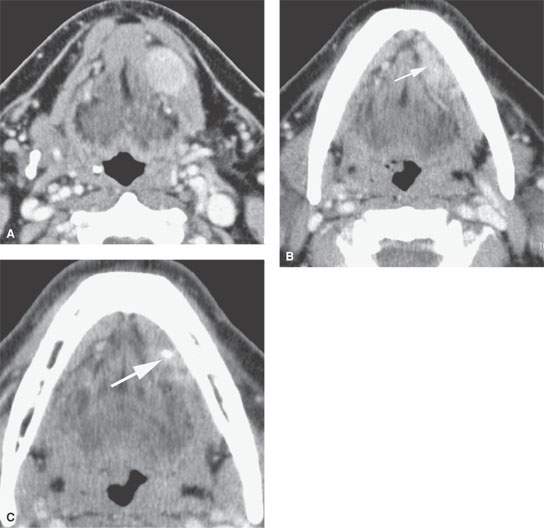
FIGURE 183.2. Computed tomography study of a patient with low-grade mucoepidermoid carcinoma. The well-circumscribed mass is seen in (A) and would be indistinguishable from a benign tumor such as a benign mixed tumor of the sublingual space. In (B), there is some secondary sialoadenitis in the sublingual gland (SLG) (arrow), which is also visible in (C) where a stone is present (arrow). It is likely that the tumor obstructed the SLG, resulting in the presence of the stone and also in the complete atrophy of the submandibular gland on that side.
Pros and Cons
General Approach
Magnetic Resonance and Computed Tomography
MR and CT are the most used imaging studies to evaluate SLG/SLS disease. Such expensive studies are not usually necessary if the mass is discrete and freely mobile. If there is a hint of an inflammatory condition of salivary gland or other origin clinically in the presence of a mass, then CT is preferred over MR.
Ultrasound
SLG tumors are usually not studied definitively with ultrasound in most practices. Some find an ultrasound useful in the initial evaluation of a mass in the floor of the mouth; in some instances, this may triage a patient to a definitive plan without the need for more advanced imaging.
Radionuclide Studies
Radionuclide studies are not used routinely for the evaluation of salivary gland masses. The constraints on its utility are discussed in more detail in Chapter 5 in general and with regard to glandular neoplasms in Chapter 22. Technetium, iodine, and fluorine-18 2-fluoro-2-deoxy-D-glucose (FDG) activity is frequently seen in normal glands (Fig. 5.9). FDG uptake is quite variable in both benign and malignant salivary gland neoplasms, somewhat limiting the utility of fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) studies in patients with salivary gland masses.
Specific Indications
- Define the origin and extent of an SLG/SLS mass: Is it likely of SLG origin? If the margins or nature of a mass are not clear after physical examination, then CT or MR may be done. This will first help to determine whether the mass point of origin is intrinsic or extrinsic to the SLG. This factor alone may markedly alter the course of management (Figs. 183.4–183.8) since submucosal floor of the mouth masses are frequently of nonglandular origin. Imaging can quickly narrow the diagnostic possibilities by excluding extrinsic causes of SLG/SLS masses.
MR or CT is almost always capable of differentiating an intrinsic SLG neoplasm from an extrinsic mass. Other submucosal masses, such as a ranula, dermoid cyst, or rare lesions of neural or mesenchymal origin, are fully capable of mimicking an intrinsic SLG lesion (Figs. 183.9–183.15). Inflammatory disease will usually manifest some degree of intrinsic surrounding inflammatory-appearing change (Figs. 183.16–183.24 and Chapter 13).
If the mass is intrinsic to the gland, it may be malignant and the study should be extended to include cervical lymph nodes and potential paths of perineural extension (Fig. 183.5).
- Define the relationship of an intrinsic SLG mass to the surrounding structures, including the mandible, SLS, and mylohyoid muscle.
- Characterize the type of intrinsic or extrinsic lesion present and the degree of invasiveness both within and beyond the SLG.
- Evaluate the full extent of the lesion, and determine whether it has a morphology or associated findings suggestive of an invasive and/or malignant process. This includes the margins of the lesion, internal signal characteristics on T2-weighted images, and perhaps behavior on DWI. Metastatic adenopathy and perineural spread are almost sure signs of a malignant tumor (Figs. 183.4–183.8).
- If extrinsic to either gland, determine whether it is a unilateral or bilateral process and whether it is multifocal on one side and/or both. This determination helps to identify whether the process is likely due to a systemic process.
- Determine the extent of perineural tumor spread in patients with known or suspected malignancies and deficits of the lingual, hypoglossal, or mandibular nerves.
- Identify regional metastatic disease.
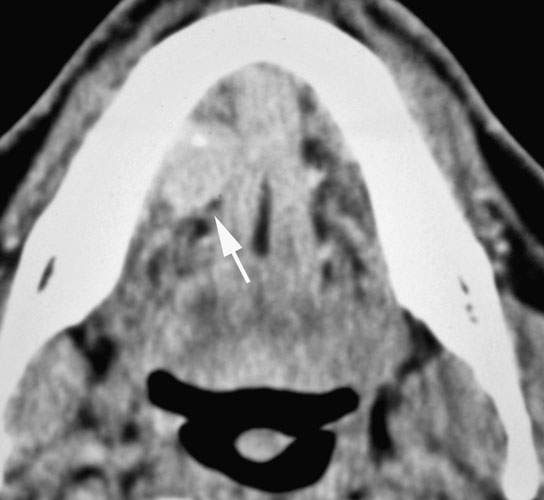
FIGURE 183.3. Adenoid cystic carcinoma of the sublingual space. The mass is very well circumscribed and contains a calcification (arrow). This mass cannot be differentiated on the basis of its appearance from a low-grade cancer of some other histology or even a benign mixed tumor. The tumor was removed, and there was no evidence of perineural spread.
Controversies
DWI data may differentiate benign and malignant salivary gland tumors with reasonable accuracy. This ability would seem to be limited by the size of the mass to some extent. Moreover, it is unlikely that any critical decision making would result from DWI data. It costs nothing and can add information, so there is no harm in doing the analysis. There is only harm in relying on the data from DWI as a critical point in the management pathway.
SPECIFIC DISEASE/CONDITION
Benign and Malignant Epithelial-Origin Tumors of the Sublingual Gland and Space
Etiology
Benign and malignant epithelial-origin tumors of the SLG and SLS are spontaneous tumors without a particular etiology.
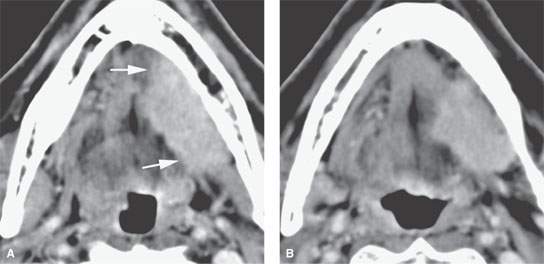
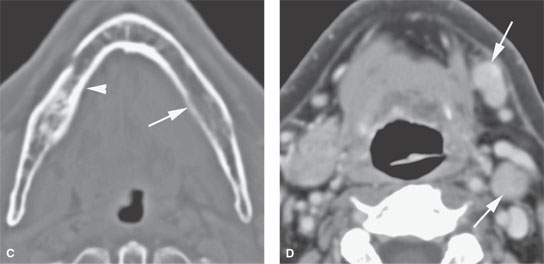
FIGURE 183.4. Computed tomography study of a patient with high-grade mucoepidermoid carcinoma of the sublingual gland. The mass has very infiltrative margins (arrows in A). In (B), the tumor invades the soft tissue of the neck (arrows). In (C), the mandibular lingual plate is eroded (arrow) compared to the normal side (arrowhead). In (D), metastatic lymph nodes are present in level 1 and level 2 (arrows).
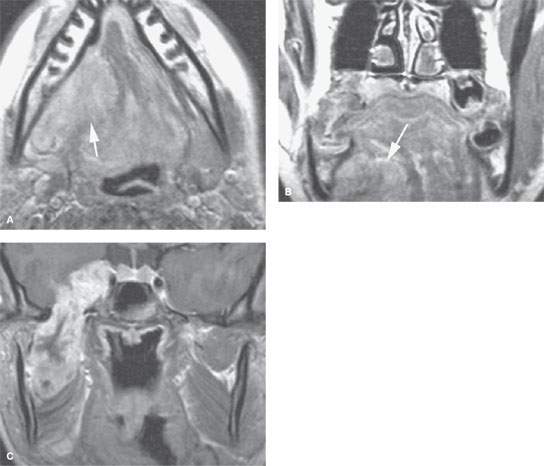
FIGURE 183.5. A young adult with rhabdomyosarcoma originating in the sublingual space, as seen on the contrast-enhanced T1-weighted images in (A) and (B) (arrows). The tumor resulted in perineural spread along the mandibular division of the trigeminal nerve, with gross disease involving the cavernous sinus region (C).
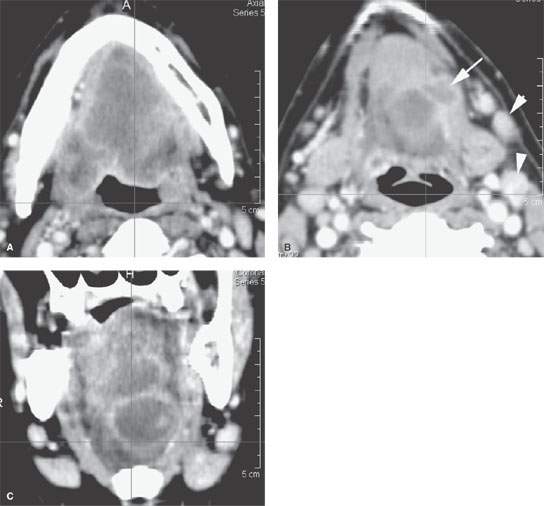
FIGURE 183.6. A–C: Computed tomography study of a patient with an entirely submucosal high-grade undifferentiated carcinoma involving the floor of the mouth and sublingual space with wide spread infiltration of those areas and the tongue. In (B), there is either direct extension into the soft tissues of the neck or a metastatic lingual lymph node (arrow). Metastatic nodes to level 2 are also present (arrowheads).
Prevalence and Epidemiology
Tumors of the major salivary glands account for 3% to 4% of all head and neck tumors. The parotid accounts for about 80% of all major salivary gland tumors. Approximately one half of SMG and SLG tumors are malignant.
Major salivary gland tumors most commonly present in adults over 20 years of age. The average age at presentation is about 55 years for cancers and 40 years for benign tumors. Cancers and benign tumors are uncommon in pediatric patients, but when they occur, they are usually of parotid origin.
Clinical Presentation
History
Most patients with either benign or malignant tumors present with a solitary, painless palpable SLS mass. Occasionally, mild pain may be present, but it does not discriminate benign and malignant lesions. A nearly constant, progressive pain is often associated with malignant neoplasms or inflammatory disease and may herald nerve invasion. Benign mixed tumors may be stable for a long period of time with an abrupt increase in size that brings the patient for physician evaluation.
Physical Examination
Reduced mobility including minimal to moderate fixation may occur in both benign and malignant SLG and SLS neoplasms (Figs. 183.2–183.8). Tumors can produce a bulge in the floor of the mouth.
The mandibular division of the trigeminal nerve (V3) may be involved or at least threatened by tumor (Fig. 183.5). The hypoglossal and lingual nerves may be involved by SLG tumors in the floor of the mouth.
Pathophysiology and Patterns of Disease
Pathology: Benign Tumors
The most common benign SLG tumor is benign mixed tumor, also known as pleomorphic adenoma. It generally presents in patients who are no younger than 20 years of age, being seen most commonly in patients around age 40 years. These tumors uncommonly present in children (Figs. 22.1, 22.2, and 22.4–22.8). The lesions are variable with respect to internal morphology due to relative amounts of connective tissue, cartilage, vascular stoma, and cystic degeneration. This results in an equally variable appearance on CT and MRI as described in Chapter 22.

FIGURE 183.7. A highly infiltrating although entirely submucosal mass as seen on non–contrast-enhanced computed tomography. The mass was due to an angiosarcoma originating in the sublingual space with extensive infiltration out of the floor of the mouth and into the oral tongue and other surrounding areas.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








