Ulcerative Proctocolitis
Ho Chia Ming
FINDINGS
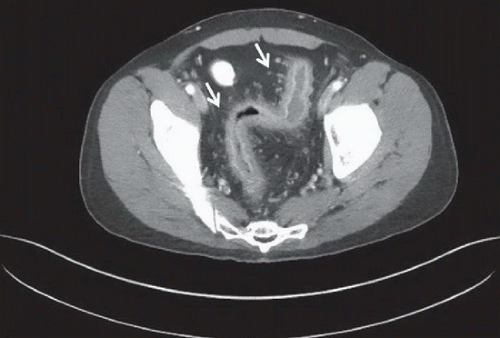
Figure 71A: Axial contrast-enhanced CT scan of the pelvis demonstrates wall thickening and stratification of the rectum, sigmoid colon, and descending colon, with increased enhancement of the mucosa, prominent vasa recta, and stranding in the adjacent fat (arrows). The remaining bowel is normal.
DIFFERENTIAL DIAGNOSIS
Inflammatory bowel disease—Crohn disease or ulcerative colitis, infectious proctocolitis, diverticulitis.
DIAGNOSIS
Ulcerative proctocolitis.
DISCUSSION
Proctocolitis refers to the inflammation of the rectum and colon. The causes of inflammation are myriad and often difficult to diagnose clinically or by imaging. Ulcerative colitis is a chronic idiopathic inflammatory bowel disease that involves the rectum and extends from the rectum to more proximal areas of the colon in a continuous fashion. Eventually, the entire colon may be involved. Typically, patients with ulcerative proctocolitis present with rectal bleeding and abdominal pain. The main role of imaging is to exclude other causes of abdominal pain at initial presentation and to exclude major complications, such as bowel perforation. Definitive diagnosis of ulcerative proctocolitis requires corroboration with clinical history, endoscopy, and histology.
In the acute to subacute phase of ulcerative colitis, erosion of the bowel mucosa may leave a residual island of regenerative tissue or pseudopolyp, which has been mistaken for a villous adenoma or polypoid carcinoma. Colonic polyposis syndrome may mimic multiple pseudopolyps related to ulcerative colitis. A constricting infiltrative or ulcerative mass indicates malignant transformation. Ulcerative colitis may also present with chronic strictures related to local sequelae of severe inflammation. Advanced cases may demonstrate diffuse loss of mucosal folds and decreased haustration, leading to a lead-pipe configuration. This may subsequently lead to recurrent pancolitis and toxic megacolon in about 5% of the patients with markedly dilated colon to at least 6 cm and associated symptoms. Backwash ileitis may also occur if the disease progresses from the cecum into the terminal ileum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree