Normal Anatomy
The paravertebral space is a wedge-shaped region demarcated by the superior costo-transverse ligament (posterior border), parietal pleura (anterolateral border), and lateral surface of the transverse process (medial border). It should be noted that the medial aspect of the paravertebral space communicates with the epidural space. The paravertebral space contains the intercostal or spinal nerves, blood vessels, rami communicantes, dorsal rami, and the sympathetic chain.
 Scanning Technique and Ultrasound Appearance
Scanning Technique and Ultrasound Appearance
The procedure is performed with the patient in sitting, lateral decubitus, or prone positions. The ultrasound transducer can be positioned in the longitudinal parasagittal plane or transverse (axial) plane. Insertion of the needle in-plane with the ultrasound transducer is highly recommended (if not mandatory) to allow for complete visualization of the entire needle at all times and avoid puncturing the pleura.
Transverse approach
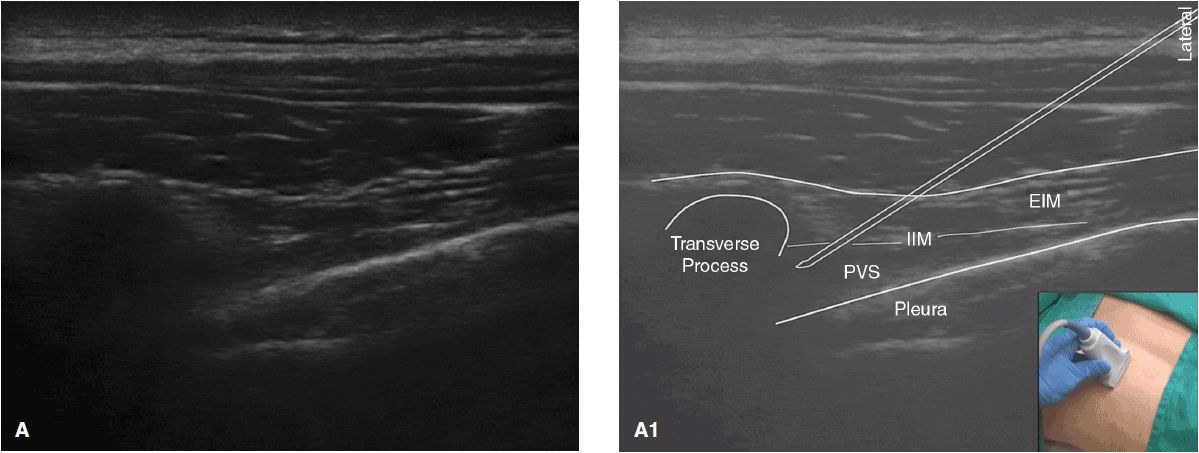
Using a linear, high-frequency (10–12 MHz) transducer, the ultrasound probe is placed parallel to the appropriate intercostal level, just lateral to the spinous process. The image is optimized by adjusting for the appropriate depth of field (usually within 3–5 cm), focus, and gain. The spinous process and the corresponding transverse process are visualized as hyperechoic lines with acoustic shadows underneath. The hypoechoic wedge-shaped paravertebral space is identified by scanning lateral to the transverse process. Care should be taken to identify the underlying pleura (Figure 15-1A, A1).
Figure 15-1. (A) Paravertebral space, ultrasound image. (A1) Paravertebral space anatomy, ultrasound probe orientation (inset). Transverse process, PVS = paravertebral space, pleura, IIM = internal intercostal membrane, EIM = external intercostal muscle.
NOTE: The pleura is distinguished as a hyperechoic line that moves with respiration and has underlying hyper-echoic air artifacts. This is to be distinguished from the rib, which contains an underlying acoustic shadow.
The use of color Doppler may aid in the identification of intercostal vessels in the paravertebral space. Care must be taken to avoid intravascular injection or injury.
In-plane needle insertion approach
The patient’s posterior midthoracic area and the ultrasound probe are prepared with standard sterile precautions. The underlying skin is infiltrated with local anesthetic. A 20- or 22-gauge needle is inserted at the lateral end of the ultrasound probe and advanced slowly into the paravertebral space under direct visualization in the lateral to medial direction. It is advisable to turn the bevel of the needle upward, toward the transducer, to reduce the risk of inadvertent puncture of blood vessels, nerves, or pleura. To facilitate better visualization of the needle tip, the hydrodissection technique may be utilized by intermittently injecting small volumes of normal saline to dissect tissue planes while under direct visualization. Once the needle tip penetrates the internal intercostal membrane and enters the paravertebral space, a test dose of local anesthetic (3 mL) can be administered after ensuring negative aspiration for blood or air.
 Clinical Pearls and Common Pitfalls
Clinical Pearls and Common Pitfalls
Injection of local anesthetic under direct visualization is highly recommended. If resistance to injection is encountered, the needle should be redirected either more laterally, or the bevel should be rotated into a different plane. Upon injection, the paravertebral space will distend and push the underlying pleura ventrally.
When performing the in-plane needle insertion approach, the needle tip should be visualized at all times in relation to the pleura to avoid the risk of pneumothorax. Frequent aspiration and incremental injection of local anesthetic are recommended to avoid inadvertent intravascular injection and systemic local anesthetic toxicity. Caution should be exercised in anticoagulated patients to avoid multiple needle passes and, thereby, decrease the risk of hematoma.
 Case Scenario
Case Scenario
A 67-year-old woman with no significant past medical history presents with right-sided chest wall pain that started approximately six months ago. The pain is described as burning, pulling sensation, worse with movement. She describes no preceding rash or blister formation or trauma to the area. Chest x-ray imaging of the ribs and thoracic spine shows no abnormalities. On physical examination, the patient reports tenderness to palpation over the right T7 and T8 dermatomes, in the anterior and midaxillary line. Differential diagnosis includes intercostal neuralgia, and the patient is scheduled for a right T7 paravertebral block. The block is performed under direct ultrasound guidance using a mixture of local anesthetic and steroid. After the procedure, the patient reports greater than 75% decrease in pain intensity and an overall improvement in the activities of daily living. She is advised to return to the pain clinic for a repeat block in the future, if needed.
INTERSCALENE BLOCK
 Normal Anatomy and Indications
Normal Anatomy and Indications
Motor, sensory, and sympathetic innervation to the upper extremity is supplied by the brachial plexus. The plexus is composed of five nerve roots (C5-T1 ventral rami), three trunks, six divisions, three cords, and five terminal nerves. The nerve roots travel through the interscalene groove, which is situated between the anterior and middle scalene muscles at the level of the cricoid cartilage (C6), superior to the subclavian artery. The vertebral artery lies anteriorly, and the phrenic nerve travels between the anterior scalene and sternocleidomastoid muscles.
The interscalene block was originally described by Winnie, and it targets the brachial plexus at the cervical root and trunk level. It is utilized mostly in regional anesthesia for operative procedures involving the shoulder and lateral clavicle to the elbow area. Continuous interscalene block with a catheter can also be used for postoperative analgesia.
 Normal Appearance on Ultrasound
Normal Appearance on Ultrasound
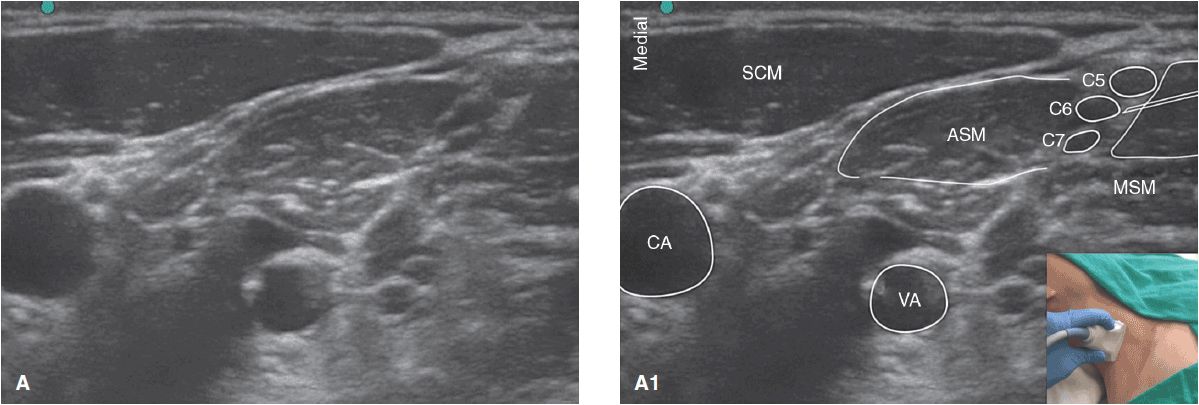
In the interscalene groove, the roots/trunks of the brachial plexus appear hypoechoic with hyperechoic fascia sheaths, often described as a “honeycomb” appearance, in the short axis. Color Doppler should be used to identify and confirm the carotid, subclavian, and vertebral arteries.
 Scanning Technique
Scanning Technique
Images are obtained using a linear, high-frequency (10–15 MHz) transducer set to 2–3 cm depth with the patient supine and the head slightly turned to the contralateral side. The interscalene groove may be visualized by scanning from identifiable anatomical landmarks superiorly or inferiorly. Starting inferiorly, the probe is placed in the supraclavicular fossa, parallel to the clavicle, where the trunks of the brachial plexus are identified along with the subclavian artery. The neurovascular bundle is followed in short-axis view up to the interscalene groove, between the anterior and middle scalene muscles. The probe should be oriented perpendicular to the interscalene groove (Figure 15-2A, A1).
Figure 15-2. (A) Interscalene anatomy, ultrasound image. (A1) Interscalene anatomy, ultrasound probe orientation (inset). CA = carotid artery, SCM = sternocleidomastoid muscle, VA = vertebral artery, ASM = anterior scalene muscle, MSM = middle scalene muscle, C5, C6, C7 = cervical nerve roots.
Alternatively, scanning superiorly, the probe may be placed in the interscalene groove at the level of the cricoid cartilage and swept laterally. Regardless of the approach, a systematic anatomical survey should always be performed with critical structures identified, including the carotid, vertebra, l and subclavian arteries, C6 transverse processes, and intervertebral foramina.
 Block Technique
Block Technique
After appropriate aseptic preparation of both the neck area and the ultrasound transducer, the injection site is infiltrated with local anesthetic, and a 22-gauge 5 cm needle is advanced either in-plane or out of plane to the ultrasound transducer. For the in-plane approach, the needle is inserted along the posterior-lateral border of the probe and is directly visualized as it advances lateral to medial through the medial scalene muscle into the interscalene groove. The out-of-plane approach may be performed on either the cranial or caudal side of the probe; this technique, however, is suboptimal as it does not allow for direct visual tracking of the needle through the tissue, and it is almost never used. Hydrodissection may be used to identify the tip of the needle, as visualization is more difficult with this approach. Injected solutions will appear hypoechoic.
 Common Findings/Abnormalities
Common Findings/Abnormalities
Although frequently described as arising from C5-T1, the brachial plexus may be prefixed, with the ventral ramus of C4 contributing, or postfixed, with the ventral ramus of T2 contributing.
 Common Pitfalls
Common Pitfalls
Complications may include nerve damage, intravascular injection, epidural and intrathecal injections, and hematoma. Pneumothorax can occur if the needle enters the cupola of the lung (block performed more distally). Local anesthetic central nervous system toxicity can occur if the needle enters the vertebral artery, and spinal or epidural anesthesia may occur if the needle enters the intervertebral foramina. Direct visualization of the needle tip should be maintained during advancement of the needle into tissue, as well as during injection of local anesthetic.
Injection too close to the transverse process may compress the roots against bony structures. The roots of C8 and T1 may be more difficult to visualize in the interscalene groove, and thus more difficult to anesthetize. If this occurs, “ulnar sparing” (or inadequate anesthesia of the medial forearm and hand) may occur with the absence of ulnar nerve blockade. If necessary, a selective ulnar nerve block may be performed, either at the infraclavicular level or at the elbow.
 Clinical Pearls
Clinical Pearls
Common side effects that can occur, especially after a large-volume interscalene block, are Horner syndrome, as the sympathetic chain may be anesthetized, and phrenic nerve palsy, with resulting diaphragmatic hemiparesis. Thus, the interscalene block should be performed with caution in patients with respiratory insufficiency, as it may result in respiratory distress. In addition, due to the risk of phrenic nerve blockade and pneumothorax, the interscalene block should never be performed bilaterally.
 Case Scenario
Case Scenario
A 72-year-old man presents for a right total shoulder replacement surgery. He has a history of obstructive sleep apnea and sensitivity to opioid medications, and is anxious about the postoperative pain control and recovery.
During preoperative anesthetic evaluation, risks and benefits of general anesthesia versus regional anesthesia using interscalene block are discussed. The benefits of regional anesthesia may include: decreased use of opioid medications and opioid-related side effects such as sedation, respiratory depression, mental status changes, nausea, decrease in anesthetic requirements during the surgery and faster recovery time, and avoidance of general anesthesia and its associated cardiopulmonary side effects.
Prior to surgery start, the patient undergoes an ultrasound-guided interscalene block with local anesthetic and catheter placement for postoperative pain control via infusion. He reports excellent pain relief after the surgery, requiring minimal amount of supplemental pain medications.
The interscalene catheter is removed on postoperative day 2, and the patient is discharged home soon after on an oral pain medication regimen.
SUPRACLAVICULAR BLOCK
 Normal Anatomy and Indications
Normal Anatomy and Indications
As described previously, the trunks of the brachial plexus exit the interscalene groove and pass under the clavicle. In the supraclavicular fossa, the superior and middle trunks lie superior to the subclavian artery, and the inferior trunk lies posterior. The neurovascular bundle is immediately superior to the first rib and 1–2 cm superior to the pleura.
The supraclavicular block was originally described by Hirschel and Kulenkampff. It targets the trunks/divisions of the brachial plexus and is ideal for anesthesia and analgesia of the arm, forearm, and hand.
 Normal Appearance on Ultrasound
Normal Appearance on Ultrasound
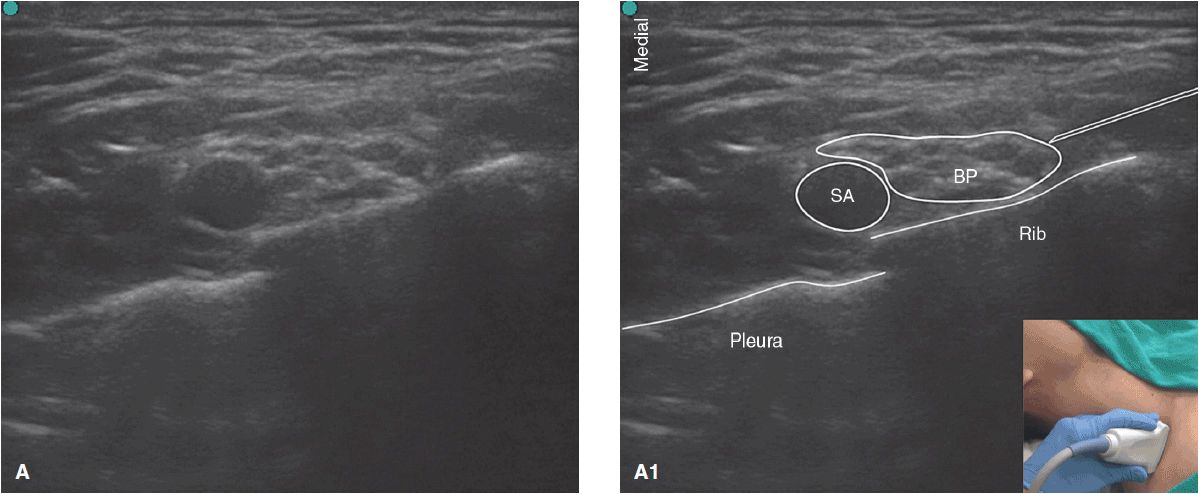
The subclavian artery can be visualized in the short axis as it passes under the clavicle. The subclavian vein is anterior and medial to the artery. The trunks, divisions, and cords appear hypoechoic, with hyperechoic surrounding fascia giving them the appearance of a “grapelike” structure. It should be noted that the number of fascicles visualized varies widely and can range from a few to as many as a dozen. Inferiorly, the first rib appears hyperechoic with an underlying acoustic shadow. Deep to it, the pleura appears as a hyperechoic line lacking an acoustic shadow. Deep to the pleura, the lung may be identified by its expansion during respiration and also by looking for the “comet tail artifact,” which occurs when two highly reflective acoustic layers of different acoustic impedance cause the echo to bounce back and forth quickly, appearing as a narrow striped band.
 Scanning Technique
Scanning Technique
The scanning technique for a supraclavicular block is similar to that of an interscalene block. The patient is positioned supine, and the head is turned slightly to the contralateral side. A linear 10–15-MHz high-frequency probe is placed in the supraclavicular fossa parallel to the clavicle and rotated into a coronal oblique position. The probe is swept medially until the subclavian artery is identified. Once this landmark is obtained, a systematic anatomical survey should be performed with the artery, first rib, pleura, and lung identified (Figure 15-3A, A1).
Figure 15-3. (A) Supraclavicular anatomy, ultrasound image. (A1) Supraclavicular anatomy, ultrasound probe orientation (inset). Pleura, 1st rib, subclavian artery, BP = brachial plexus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree