Fig. 6.1
Patient’s position for US of axillary lymph nodes
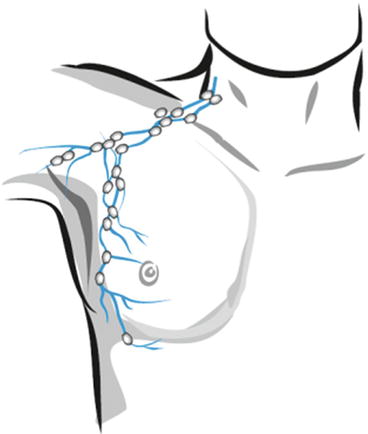
Fig. 6.2
Lymph nodes affected at breast pathology
Medially from the pectoralis minor muscle
Along axillary vessels
Between the pectoralis major and minor muscles
Axillary lymph nodes can be classified into the following levels:
Level 1 (inferior axillary) lymph nodes are located laterally from the lateral border of the pectoralis minor muscle.
Level 2 (middle axillary) lymph nodes are located between medial and lateral edges of the pectoralis minor muscle and interpectoral (Rotter’s) lymph nodes.
Level 3 (apical axillary) lymph nodes are located medially from the medial edge of the pectoralis minor muscle including subclavian and apical.
Intramammary lymph nodes are coded as axillary.
US characterization of the lymph nodes involves evaluating the following aspects:
Site, according to anatomical area
Number
Dimensions (in three planes)
Short/long axis ratio in transverse view
Similarity of changes
Shape (flat, oval, spherical, or irregular)
Echodensity of the lymph node in general (increased, medium, or decreased)
Differentiation of lymph node parts (present/absent)
Differentiation of the hilum (present/absent)
Core echodensity (high, low, or isoechoic)
Status of the cortex of the lymph node (narrow/wide)
Mobility upon compression with the probe
Vascularity
Features of stiffness evaluated with elastography
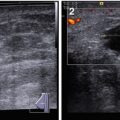
Healthy axillary lymph nodes demonstrate the following sonographic features (Fig. 6.3):
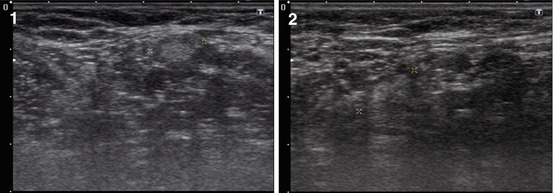
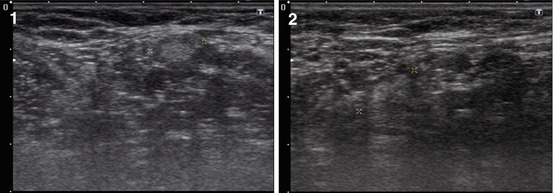
Fig. 6.3
(1, 2) Healthy axillary lymph nodes. Grayscale US
Oval (or bean-like, tape-like) shape
Length smaller than 10 mm
Regular, well-defined contours
Hypoechoic or isoechoic peripheral part and hyperechoic central part
Painless, moderately mobile upon compression with the US probe
Avascular or hypovascular in color Doppler imaging (CDI), power Doppler imaging (PDI), and vascular three-dimensional power Doppler imaging (3DPD), with predominant vascularity of the hilum (Fig. 6.4)
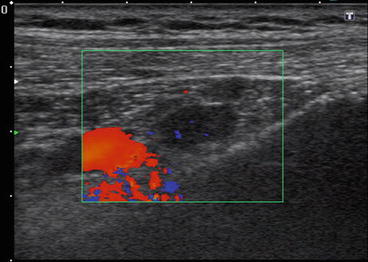
Fig. 6.4
Healthy axillary lymph nodes. CDI and PDI
Soft- or mixed-type color pattern with sonoelastography comparable with the pattern of the surrounding structures
A healthy lymph node has a width of up to 10 mm on transverse scan, although, according to a number of authors, the dimensions of healthy lymph nodes vary significantly. The Solbiati index (SI), which is the ratio of the largest to the smallest diameter of a lymph node, is normally 2.9 ± 0.13 in adults and 2.4 ± 0.05 or above in children (Solbiati and Rissato 1995).
The assessment of vascularity with CDI and PDI supplies additional data for the differential diagnosis of the origin of an enlarged lymph node. Vessels, if any are detected, are usually located within the hilum in healthy or reactive lymph nodes. Even in large benign hyperplastic lymph nodes, the vascular pattern remains regular. Vessels are normally observed along the capsule and radially from the hilum to the periphery.
Abbasova et al. (2005) classify the vascular pattern of lymph nodes into the following four categories:
1.
Hilar: individual arterial and/or venous flow signals without diffusion to the parenchyma of the lymph node and without branching
2.
Activated hilar (central) type: venous and arterial flow signals branching radially within the hilum and medulla
3.
Peripheral: flow signals along the periphery of the lymph nodes without subcapsular branches arising from the hilar vessels
4.
Mixed: presence of hilar and peripheral flow signals
(a)
One large artery in the hilum with individual dot-shaped color signals in the periphery
(b)
Fragments of afferent artery and chaotic flow signals within the solid component of the lymph node
According to Sinyukova et al. (2007), healthy lymph nodes exhibit single vessels in 58 % of cases. In the case of multiple vessels, their pattern is regular, with branching from the hilum to periphery. Doppler data, according to Abbasova et al. (2005), do not affect the differential diagnosis of enlarged lymph nodes. The enlargement of a lymph node may appear as a manifestation of a variety of diseases, such as specific or nonspecific inflammation of head and neck organs, metastases, and hemoblastoses (e.g., Hodgkin’s disease).
Nonspecific types of lymphadenitis are divided into the following groups (Trofimova 2008):
1.
According to disease severity
Acute
Subacute
Chronic
2.
According to dispersion
Isolated
Regional (in groups)
Extended
Generalized
Individual and multiple lymph nodes as well as lymph node conglomerations can be also described. Reactive hyperplasia of lymph nodes may result from different pathological processes (an inflammatory process, vaccination, injections, etc.). Lymph nodes that are close to a tumor can also present a nonspecific reaction of an inflammatory character (Trofimova 2008).
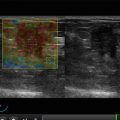
Hyperplastic lymph nodes usually exhibit the following US features (Sinyukova et al. 2007) (Figs. 6.5, 6.6 and 6.7):
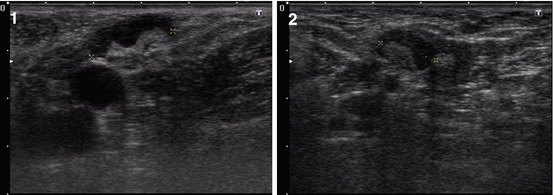
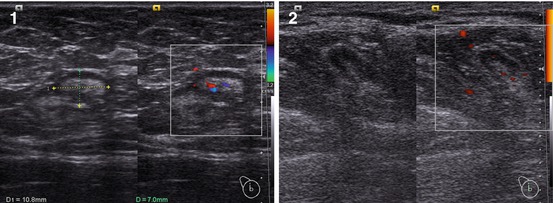
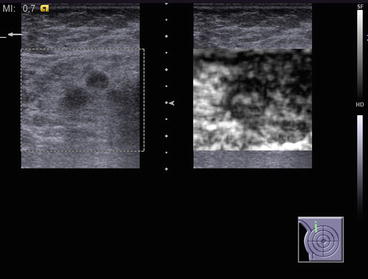
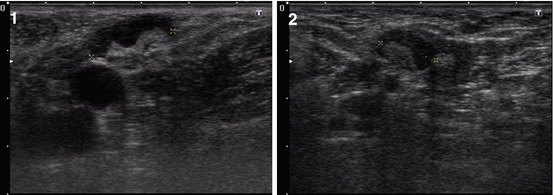
Fig. 6.5
(1, 2) Reactive axillary lymph nodes. Grayscale US
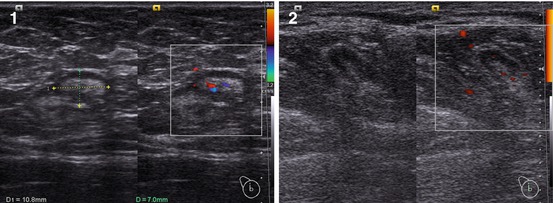
Fig. 6.6
(1, 2) Reactive axillary lymph nodes. CDI and PDI
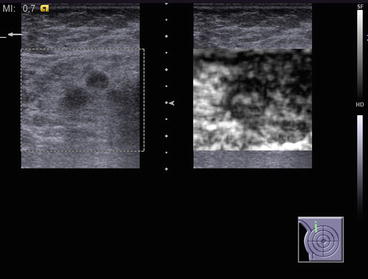
Fig. 6.7
Reactive axillary lymph nodes. US elastography
Size of >10 mm
Roundish shape
Decreased or normal general echodensity
Heterogeneous echostructure with thick regular cortex
Regular distinct margins
Avascularity or hypovascularity in CDI, PDI, and 3DPD
Low values of peak systolic blood flow velocity (PSV), end-diastolic blood flow velocity (EDV), and resistive index (RI) in pulsed-wave (PW) Doppler imaging
No difference in color pattern as compared with the surrounding tissues in US elastography
Inflammatory lymph nodes show fast dynamics. Even without therapy, they often sonographically disappear after 5–7 days. Treatment speeds up their involution, resulting in the restoration of the oval shape of the node and the sharpness of margins, an increase in the general echodensity with more accurate corticomedullary differentiation, and a decrease in blood flow intensity and morbidity upon compression.
6.2 Regional Lymph Node Metastases
Low differentiation with high malignant potential is the factor that promotes progression of breast carcinoma in men. The most unfavorable prognostic feature is invasion of tumor cells into lymphatic and blood vessels, which significantly increases the risk of remote metastases. Metastatic processes are detected in 62.5 % of men with such an invasion and only in 18.7 % of patients without it (Akimov 1992). The incidence of metastases of breast cancer in regional lymph nodes is 19–75 % (Chissov 2003; Sinyukova et al. 2007; Trufanov et al. 2009). The sensitivity of US in the detection and differentiation of malignant lymph nodes in patients with breast carcinoma ranges from 70 to 99 %, with a specificity of 83–97 % (Table 6.1). Both depend on the quality of equipment and the skills and experience of the operator (Cosgrove et al. 1990; Svensson et al. 2000; Drincovic 2002).
Table 6.1
Diagnostic value of US in the diagnosis of metastases of breast carcinoma in axillary lymph nodes
Authors | Year | Sensitivity (%) | Specificity (%) | Diagnostic accuracy (%) |
|---|---|---|---|---|
Kharchenko et al. | 88 | 80
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|