Ultrasound Imaging of Joint Disease
Pitfalls and Limitations
If it proves difficult to maintain probe contact with the skin surface using minimal probe pressure, a thick application of sonographic jelly may help.
Disadvantages compared to MRI include a small field of view and difficulty in demonstrating cartilage and deep joints in their entirety. Contrast-enhanced MRI provides a better measure of capillary permeability and enhancement characteristics, although the advent of 3-D ultrasound may narrow this gap. At present, both ultrasound and MRI are increasingly important in the diagnosis and management of early rheumatoid arthritis with no current clear winner as the imaging modality of choice.
Techniques for Scanning the Small Joints of the Hands and Feet
Routine examination of the extensor aspect of the MCPJs, followed by the extensor, ulnar and radial aspects of the IPJs, is performed.
Coronal images of the IPJs are obtained by asking the patient to hyperextend the metacarpophalangeal of the finger being examined.
When examining the extensor surfaces of the finger joints, it is commonplace to assess the dorsal aspects of the wrist and associated tendons prior to turning to the palmar side. Whether both the extensor and flexor sides need to be examined remains debatable; however, published literature suggests that a significant proportion of synovitis would be overlooked if limited to one or the other, and it is the authors’ practice to examine the flexor aspects of the MCP and proximal IPJs at this time. Dynamic sonographic assessment by moving the joint can be useful to facilitate the detection of low-volume synovial thickening, which bunches up in the proximal extensor recess on flexion. Articular cartilage over the metacarpal and phalangeal heads can be more comprehensively demonstrated when the joint is examined in flexion as well as extension.
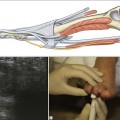
It is essential to appreciate the normal sonographic anatomy of the small joints to be able to identify pathology (Fig. 32.1). Superficial and deep flexor tendons can be identified as they pass over the MCPJs into the flexor tendon sheath of the fingers on the volar aspect of the joints. Dynamic assessment with finger movement can help identify them individually. The tendons are maintained in place by pulleys, seen as thin hypoechoic linear structures; the pulleys and other aspects of tendon pathology are discussed in Chapter 15.
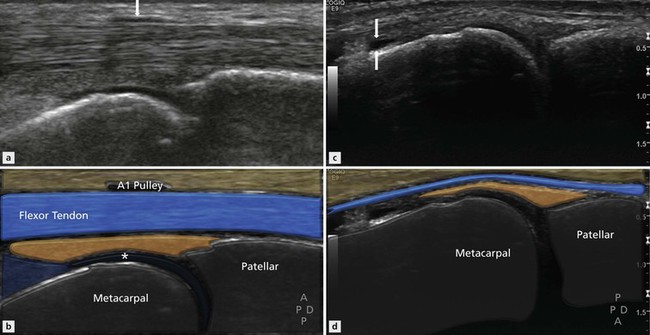
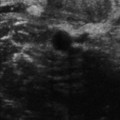
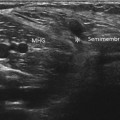
Figure 32.1 Small joint anatomy. (A, B) Sagittal view of the flexor aspect of the MCPJ. The flexor tendons lie anterior to the joint capsule. The volar plate, articular cartilage (*) and A1 pulley (arrow) are visible. (C, D) Sagittal view of the extensor surface of the middle MCPJ. The normal articular cartilage (*) is seen clearly. There is a small amount of joint fluid present that can be seen in the dorsal joint recess (arrows).
It is important not to misdiagnose intracapsular fat as synovial thickening, particularly as the proximal recess is where early and prominent synovial thickening may occur.
On the extensor surface of the joint the extensor tendon complex is identified. The joint line is evident and articular cartilage may be seen, especially over the metacarpal heads. An important recess to the MCP and IP joints is found over the dorsal aspect of the metacarpal or phalanx on the proximal side of the joint that may contain synovitis or fluid and should not be mistaken for a bursa or tenosynovitis.
Absolute measurements of normal joints remain undefined and most authors use the point of maximal joint distension for assessment of the joint; an increase in joint dimension of more than 1 mm above normal is sufficient to suggest abnormality.