SONOGRAM ABBREVIATIONS
CFA Common femoral artery
CFV Common femoral vein
IEA Inferior epigastric artery
LA Linea alba
SP cord Spermatic cord
KEY WORDS
Aponeurosis. A sheet-like fibrous membrane, resembling a flattened tendon, which serves as a fascia to bind muscles together or as a means of connecting muscle to bone.
Fascia. Dense connective tissue layer.
Hernia. A protrusion of a part or structure through the tissues normally containing it.
Epigastric Hernia. Midline hernia superior to the umbilicus.
Femoral Hernia. Herniation of the abdominal contents though the femoral canal, leading to a bulge below the inguinal ligament.
Hypogastric Hernia. Midline hernia inferior to the umbilicus.
Incarcerated Hernia. The trapping of abdominal contents within the hernia itself, which cannot be reduced or pushed back.
Inguinal Hernia (“Groin Hernia”). The most common (75%) of all abdominal hernias. Subdivided anatomically into direct and indirect, although this distinction is generally not of surgical importance.
Direct. Acquired groin hernia, ~25% of all hernias.
Indirect. Congenital groin hernia, ~50% of all hernias.
Interstitial Hernia. Hernia contents that extend between muscle or fascial layers.
Recurrent Hernia. A hernia that has been previously repaired surgically and now has returned.
Spigelian Hernia. Protrusion of properitoneal or intraperitoneal contents through the semilunar line.
Strangulated Hernia. Injury to the blood circulation to the intestine caused by incarceration that results in dead bowel and a surgical emergency.
Umbilical/Paraumbilical Hernia. Hernia that develops in and around the area of the umbilicus (belly button or naval).
International Normalized Ratio (INR). A laboratory test that measures one aspect of the blood’s ability to clot. Commonly used to monitor patients taking warfarin (Coumadin) as a blood thinner, the INR has replaced the older prothrombin time (PT) test that was used to measure how much blood coagulation has been inhibited. Values that are too high predispose the patient to spontaneous hemorrhage.
Linea Alba. The median vertical tendinous line formed of fibers from the aponeuroses of the two rectus abdominis muscles that extends from the xiphoid process to the pubic symphysis.
Peritoneal Membrane. Inner abdominal cavity lining; it fully surrounds the intestines and abdominal organs. It lies between the muscles of the abdominal wall and intestines.
Process Vaginalis. A pouch of peritoneum that is carried into the scrotum by the descent of the testicle and which in the scrotum forms the tunica vaginalis.
Properitoneal. Lying between the parietal peritoneum and the ventral musculature of the body cavity (herniated mass, fat).
Semilunar Line. A curved line on the ventral abdominal wall parallel to the midline and halfway between it and the side of the body that marks the lateral border of the rectus abdominis muscle. Also known as the linea semilunaris.
Tunica Vaginalis. The inner covering of the spermatic cord, continuous above the deep inguinal ring with the transversalis fascia.
Valsalva Maneuver. Performed by attempting to forcibly exhale while keeping the mouth and nose closed.
Volvulus. A twisting of the bowel on itself, causing intestinal blockage.
RELEVANT LABORATORY VALUES
INR: 0.9 to1.1 (normal). When the patient is taking a blood thinner such as warfarin (Coumadin), one generally tries to maintain the INR between 2 and 3.5 (depending on the disease being treated). Values greater than 5 dramatically increase the risk of a spontaneous hemorrhage.
Clinical Problem
Abdominal wall masses are a common clinical problem. Hernias are one of the most common causes of abdominal wall masses and may be difficult to diagnose by clinical acumen alone. Sonography is an accurate means of identifying abdominal wall hernias when the clinical diagnosis is uncertain. The clinical diagnosis of hernias is particularly difficult in females, obese, and postoperative patients, and those with recurrent pain or swelling after hernia repair. Even when the physical findings alone establish the diagnosis of hernia, they cannot accurately characterize individual hernia features. Ultrasound can diagnose hernias in cases when the clinical findings are nonspecific. Additionally, it can accurately characterize the individual hernia features that impact treatment. Sonography can determine the hernia’s anatomic location, its contents, and complications such as incarceration, bowel obstruction, volvulus, and strangulation. Sonography is the only imaging modality that allows real-time evaluation of the hernia and its contents. Keep in mind that sonographic diagnosis of hernias may be difficult. Therefore, it is essential to be familiar with the sonographic anatomy, the variable appearances, and the common locations of hernias.
Other causes of abdominal wall masses include hematomas, infections, and soft-tissue tumors. Ultrasound and clinical clues permit rapid and accurate assessment of the first two of these possibilities. Although ultrasound is generally not accurate in fully evaluating true soft-tissue tumors, it alerts one to the fact that a tumor is present and may assist in performing a needle biopsy of the mass in the appropriate clinical setting.
Anatomy
Hernia type is determined by site of origin, which is limited to areas where aponeurosis and fascia are not protected by overlying striated muscle. There are two main categories: groin hernias and anterior abdominal wall hernias. Groin hernias include inguinal (both indirect and direct varieties) and femoral types. Anterior abdominal wall hernias include umbilical, linea alba (epigastric and hypogastric), Spigelian, and incisional types. The anatomy differs for each hernia type; however, the scanning principles remain the same.
Hernia contents vary. Not all hernias contain bowel. In fact, the majority of hernias diagnosed by sonography contain only fat and membranes, with only a small percentage containing bowel and/or peritoneal fluid. Preoperative recognition of the hernia contents helps to assess the risk of complications such as strangulation.
Hernias are defined as “a protrusion of a part or structure through the tissues normally containing it.” Thus, the fat within a hernia need not be intraperitoneal in origin (Fig. 13-1). Symptomatic, indirect inguinal, femoral, Spigelian, and linea alba hernias may contain only properitoneal fat. Unfortunately, it is not always possible to determine sonographically whether fat is intraperitoneal or properitoneal in origin.
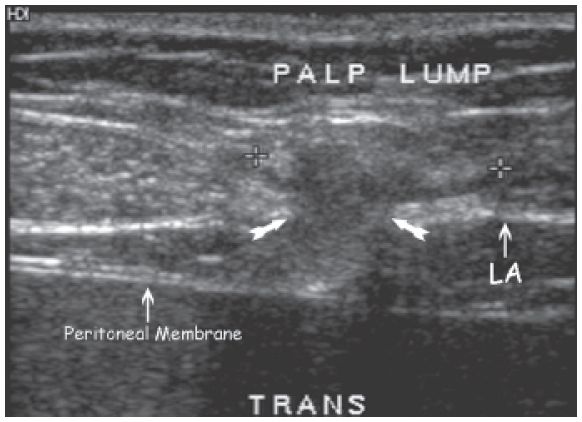
Figure 13-1. ![]() Transverse midline image demonstrates an epigastric (superior to the umbilicus) hernia containing properitoneal fat (between cursors). There is a defect (arrows) in the linea alba allowing the fat that normally lies between the peritoneal membrane and linea alba to be herniated.
Transverse midline image demonstrates an epigastric (superior to the umbilicus) hernia containing properitoneal fat (between cursors). There is a defect (arrows) in the linea alba allowing the fat that normally lies between the peritoneal membrane and linea alba to be herniated.
Technique
Because the sonographic contrast between hernia contents and surrounding abdominal wall tissues is minimal, the key to diagnosis in most cases is demonstrating the movement of hernia contents during dynamic maneuvers. During the Valsalva maneuver, hernia contents move distally, and the hernia widens. During the relaxation after Valsalva, hernia contents move back toward the abdomen, and the sac narrows. Compression with the transducer reduces the hernia and pushes contents back toward the abdomen, whereas release of the transducer results in the opposite effect. Most hernias enlarge (and some are present only) in the upright position. Therefore, when a hernia is not demonstrable in the supine position, even after Valsalva maneuvers, it is important to scan the patient in the upright position. Failure to do so will result in some hernias being missed. Additionally, many hernias are symptomatic only in the upright position. Some hernias that are completely reducible in the supine position are nonreducible in the upright position. Competing diagnostic imaging studies, like computed tomography or magnetic resonance imaging, are not capable of evaluating patients in the upright position or in real time during dynamic maneuvers.
Pathology
INGUINAL HERNIAS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


