Outline
Normal Transvaginal Sonographic Findings in the Early First Trimester, 83
Confirmation or Exclusion of Intrauterine Pregnancy When No Yolk Sac or Embryo Is Seen, 84
Ultrasound Demonstrates No Intrauterine Fluid Collection and No Adnexal Abnormality (No Extraovarian Adnexal Mass or Significant Free Fluid), 84
Ultrasound Demonstrates an Intrauterine Fluid Collection and No Adnexal Abnormality, 85
Ultrasound Demonstrates a Complex or Solid Adnexal Mass, 87
Assignment of Gestational Age by Early First Trimester Ultrasound, 87
Diagnosis of Failed Intrauterine Pregnancy (Miscarriage), 88
Sonographic Findings Definitive for Failed Intrauterine Pregnancy, 88
Crown-Rump Length With No Embryonic Heartbeat, 88
Mean Sac Diameter With No Embryo, 88
Time-Based Criteria for Pregnancy Failure, 89
Sonographic Findings Suspicious (but Not Definitive) for Failed Intrauterine Pregnancy, 90
Crown-Rump Length With No Embryonic Heartbeat, 90
Mean Sac Diameter With No Embryo, 90
Time-Based Criteria Suspicious for Pregnancy Failure, 90
Empty Amnion Sign, 90
Expanded Amnion Sign, 90
Large Yolk Sac, 91
Risk Factors for Impending Pregnancy Failure When Embryonic Heartbeat Is Seen, 91
Slow Embryonic Heart Rate, 92
Subchorionic Hematoma, 93
Small Gestational Sac Size in Relation to the Embryo, 93
Assessment of Pregnancy Number, 93
Summary of Key Points
- •
The progression of transvaginal sonographic findings in normal early first trimester pregnancies follows a highly predictable pattern, with a gestational age variability of approximately ±0.5 week: gestational sac at 5.0 weeks, yolk sac at 5.5 weeks, embryo with heartbeat at 6.0 weeks, and amnion at 7.0 weeks.
- •
In a woman with a positive pregnancy test and no evidence of an intrauterine or ectopic pregnancy on ultrasound (pregnancy of unknown location [PUL]), a single hCG measurement does not reliably distinguish a normal intrauterine pregnancy from a failed intrauterine pregnancy or an ectopic pregnancy.
- •
In a woman with a positive pregnancy test, any round or oval intrauterine fluid collection should be interpreted as highly likely to be a gestational sac, not a pseudogestational sac or decidual cyst, and treatments that could damage an intrauterine pregnancy should be avoided.
- •
An extraovarian mass can be distinguished from an intraovarian lesion, such as a corpus luteum, by observing its motion relative to the ovary when pressure is applied by the transvaginal transducer.
- •
Sonographic findings definitive for failed intrauterine pregnancy include crown-rump length (CRL) of at least 7 mm without cardiac activity, mean sac diameter (MSD) of at least 25 mm without an embryo, and no embryo with a heartbeat on a follow-up scan at specific time intervals after the initial scan.
- •
Sonographic findings suspicious, but not definitive, for failed intrauterine pregnancy include CRL of less than 7 mm without cardiac activity, MSD of 16 to 24 mm without an embryo, no embryo with a heartbeat 6 weeks or more after the first day of the last menstrual period (LMP), empty amnion sign, expanded amnion sign, and a large yolk sac.
- •
Risk factors for pregnancy failure when embryonic heartbeat is seen include slow heart rate, large subchorionic hematoma, and small gestational sac size.
- •
Pregnancy number (singleton, twin, triplet, and higher order multiples) assessed prior to 6 weeks of gestation may subsequently decrease owing to the vanishing twin phenomenon or may increase by one or more additional embryos that appear on a follow-up scan.
A developing pregnancy generally becomes visible on transvaginal ultrasound at 5 weeks’ gestational age, which corresponds to 3 weeks after conception and 5 weeks after the first day of the LMP in a woman with regular 28-day cycles. This chapter will address sonographic evaluation of pregnancies during the gestational age range of 5.0 to 8.0 weeks. Since the 1970s, this age range has been a major focus of ultrasound research. Improvements in ultrasound technology over the past 3 decades, especially the introduction and dissemination of transvaginal sonography, have made ultrasound an increasingly valuable tool.
During the early part of the first trimester, very careful sonographic technique and interpretation are critical because of the small size of the pregnancy-related structures in the uterus and adnexa, including the intrauterine or ectopic gestational sac and corpus luteum. If done well, ultrasound can confirm the presence and location of pregnancy and accurately determine the gestational age. If done poorly, an intrauterine pregnancy can be mistaken for an ectopic pregnancy, or a normal pregnancy in the uterus can be mistaken for a failed pregnancy (also termed miscarriage ), mistakes that can have serious consequences.
Normal Transvaginal Sonographic Findings in the Early First Trimester
Approximately 1 week after fertilization, the pregnancy implants in the decidua on one side of the uterine cavity ( Fig. 4-1 ), but it is not yet visible on ultrasound for about 2 more weeks. The progression of findings on transvaginal sonography in normal early first trimester pregnancies follows a highly predictable pattern, with a gestational age variability of approximately ±0.5 week. The gestational sac is first seen on transvaginal sonography at 5.0 weeks of gestation as a fluid collection 2 to 3 mm in diameter normally located in the central echogenic region of the uterus, which corresponds to the decidua ( Figs. 4-2 and 4-3 ). It grows at the rate of 1 mm/day over the course of the next week. The first structure that is identifiable within the gestational sac is the yolk sac, which appears as a circular structure up to 6 mm in diameter ( Fig. 4-4 ). It can be seen beginning at 5.5 weeks and remains visible for most of the first trimester. The embryo is first visible at 6.0 weeks, initially appearing as a 1- to 4-mm echogenic structure adjacent to the yolk sac with a flickering motion inside it, representing the beating heart ( Fig. 4-5 , , Table 4-1 ).





| Gestational Age (Weeks) | Structure First Appears on Ultrasound * | Mean Sac Diameter (mm) | Crown-Rump Length (mm) |
|---|---|---|---|
| 5.0 | Gestational sac | 2 | — |
| 5.5 | Yolk sac | 6 | — |
| 6.0 | Embryo with heartbeat | 10 | 3 |
| 6.5 | 14 | 6 | |
| 7.0 | Amnion | 18 | 10 |
| 7.5 | 22 | 13 | |
| 8.0 | 26 | 16 |
* ±0.5-week age range for first visibility of each structure.
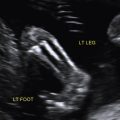
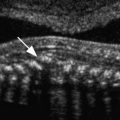
By 7.0 weeks, the embryo is approximately 1 cm in length and is still fairly featureless. At that point, the amnion first becomes visible around the embryo, as the amniotic cavity enlarges with fluid between the embryo and the amnion ( Figs. 4-6 and 4-7 ). By 8.0 weeks’ gestation, the embryo is 16 mm in length, and individual body parts can be identified on ultrasound. The embryonic head can be distinguished from the trunk, and limb buds are visible ( Fig. 4-8 ).



Confirmation or Exclusion of Intrauterine Pregnancy When No Yolk Sac or Embryo Is Seen
When a sonogram is performed on a woman with a positive pregnancy test, a fundamental question concerns where the pregnancy is located: intrauterine or ectopic. The question is answered based on the sonographic findings in the uterus and adnexa. The sonographic finding that is definitive for a gestational sac in either location is a fluid collection containing a yolk sac or an embryo with cardiac activity. In the absence of such a fluid collection, the diagnosis is less straightforward. We will consider a number of scenarios involving various potential sonographic appearances of the uterus and adnexa.
Ultrasound Demonstrates No Intrauterine Fluid Collection and No Adnexal Abnormality (No Extraovarian Adnexal Mass or Significant Free Fluid)
When the human chorionic gonadotropin (hCG) test is positive but ultrasound demonstrates neither an intrauterine nor ectopic pregnancy, the woman is said to have a pregnancy of unknown location (PUL). The diagnostic possibilities in this setting are a normal intrauterine pregnancy that is too early to be visualized, a failed intrauterine pregnancy (miscarriage), and an ectopic pregnancy. The quantitative hCG is of some value in distinguishing among these possibilities, but care must be taken not to rely on a single hCG level.
The concept of the hCG discriminatory zone was introduced by a study published in 1981. That study demonstrated that, in women with normal intrauterine pregnancies, a gestational sac was not generally identifiable on transabdominal ultrasound (the ultrasound technique in general use at that time) when the hCG was below 6000 mIU/mL, and a gestational sac was consistently seen when the hCG was above 6500 mIU/mL. Since that time, the latter of these values—the hCG measurement above which a gestational sac is consistently visible on ultrasound, or the discriminatory level—has been the focus of considerable attention. The rationale is that nonvisualization of an intrauterine fluid collection when the hCG measurement is above the discriminatory level largely excludes a normal intrauterine pregnancy, so it may be safe to undertake treatment for possible ectopic pregnancy without fear of causing harm to a pregnancy that might have a good outcome. As ultrasound technology improved, especially with the introduction of transvaginal sonography, gestational sacs could be identified earlier in pregnancy. This led to a progressive decrease in the recommended hCG discriminatory level. By the mid-1980s it dropped to 1000 to 2000 mIU/mL.
Management algorithms based on the hCG discriminatory level were put forth for women with bleeding and pain in early pregnancy, when the hCG measurement is above the discriminatory level and no intrauterine or ectopic pregnancy is identified on ultrasound. One algorithm advocates administering systemic methotrexate for suspected ectopic pregnancy in this setting. Another algorithm recommends performing a dilatation and curettage procedure (D&C) and then administering systemic methotrexate if no chorionic villi are retrieved.
Over the past several years, however, it has become clear that these management algorithms are overly simplistic and can result in serious errors. As our knowledge of PUL has increased, a number of important points have been learned:
- •
The discriminatory level does not reliably exclude a normal intrauterine pregnancy. In particular, an hCG value above 2000 mIU/mL, or even above 3000 mIU/mL, in conjunction with a sonogram demonstrating no intrauterine saclike structure, does not fully exclude a normal intrauterine pregnancy.
- •
A single hCG measurement in a woman with PUL does not reliably distinguish a normal intrauterine pregnancy from a failed intrauterine pregnancy or an ectopic pregnancy.
- •
Delaying treatment by a few days in a woman with ectopic pregnancy and no adnexal mass on ultrasound carries little risk if she is hemodynamically stable.
Ultrasound Demonstrates an Intrauterine Fluid Collection and No Adnexal Abnormality
In a woman with a positive pregnancy test, an intrauterine fluid collection without a yolk sac or embryo can represent a gestational sac, fluid (blood or secretions) in the uterine cavity, or a cyst in the decidua. Around 1980, ultrasound practitioners observed that some women with an ectopic pregnancy have fluid in the uterine cavity. Despite the fact that the location of this fluid is different from that of a gestational sac—the former is situated in the uterine cavity and the latter within the decidua—the limited resolution of ultrasound equipment at that time often made it difficult to distinguish between them. As a result, intrauterine fluid in women with ectopic pregnancy was termed a pseudogestational sac . Subsequently, it was noted that decidual cysts can also be seen in some women with ectopic pregnancy.
Because of the importance of diagnosing intrauterine pregnancies and distinguishing them from ectopic pregnancies, early practitioners sought criteria that would permit them to conclude that a fluid collection in the uterus was a gestational sac. Two signs of intrauterine pregnancy were put forth: the double sac sign and the intradecidual sign ( Fig. 4-9 ). The double sac sign refers to the presence of two concentric echogenic rings surrounding at least part of the fluid collection, hypothesized to represent the decidua capsularis and parietalis. The intradecidual sign refers to an intrauterine fluid collection eccentrically located in the decidua, anterior or posterior to a thin white line representing the collapsed uterine cavity.

The development and wide dissemination of transvaginal ultrasound in the mid- to late 1980s revolutionized early pregnancy sonography. With this technique, gestational sacs can be seen earlier in pregnancy and with different sonographic characteristics than via transabdominal sonography. In particular, normal early gestational sacs frequently display neither the double sac sign nor the intradecidual sign on transvaginal sonography ( Fig. 4-3 ). Furthermore, intrauterine fluid in women with ectopic pregnancy can often be distinguished from gestational sacs when scanning transvaginally, in that the fluid with ectopic pregnancy often conforms to the shape and location of the uterine cavity, has an irregular shape, and is filled with debris ( Fig. 4-10 ).

Despite the far greater resolution of transvaginal sonography, some practitioners continue to rely on the concepts of pseudogestational sac, double sac sign, and intradecidual sign that were defined using transabdominal sonography, even when interpreting transvaginal scans in early pregnancy. Furthermore, a misconception about these signs appears to be fairly common: “the presence of a double sac sign or intradecidual sign indicates intrauterine pregnancy” (correct interpretation) is sometimes assumed to mean “the absence of a double sac sign or intradecidual sign excludes intrauterine pregnancy” (incorrect interpretation). Such misinterpretation may lead to management errors in early pregnancy: small intrauterine fluid collections in early pregnancy, representing gestational sacs, are incorrectly diagnosed as pseudogestational sacs associated with ectopic pregnancy, leading to treatments (systemic methotrexate or D&C) that damage the intrauterine pregnancy. Reports of malpractice lawsuits for this error and the existence of online support groups for women mismanaged in this way are evidence that this is not a rare occurrence.
A straightforward calculation based on recent data is informative. Approximately half (range: 35-70%) of early intrauterine gestational sacs have a nonspecific saclike appearance: they are oval or round with no double sac sign or intradecidual sign. About 3% of women with ectopic pregnancies have an intrauterine fluid collection with a similar cystic appearance. Two percent of all pregnancies in the United States are ectopic, and 98% are intrauterine. Combining these values, it follows that, when an intrauterine saclike fluid collection without a double sac sign or intradecidual sign is seen on ultrasound in the absence of an adnexal mass or significant free pelvic fluid, the likelihood is at least 99% that it is a gestational sac and at most 1% that the diagnosis is ectopic pregnancy.
The takeaway message is that any round or oval intrauterine fluid collection in early pregnancy should be interpreted as highly likely to be a gestational sac and that treatments that would damage a desired intrauterine pregnancy should be avoided unless a potentially normal intrauterine pregnancy is subsequently ruled out.
Ultrasound Demonstrates a Complex or Solid Adnexal Mass
When an adnexal mass is seen in a woman with a positive hCG test, the crucial distinction is whether it is intraovarian or extraovarian. An intraovarian mass is almost certainly a corpus luteum (unless the flicker of a heartbeat is seen within it), whereas an extraovarian mass is highly likely to represent an ectopic pregnancy. An extraovarian mass with a “tubal ring” appearance—anechoic center surrounded by an echogenic ring—has the highest probability of representing an ectopic pregnancy, but even in the absence of such characteristics, a complex or solid adnexal mass outside the ovary in a woman with a positive pregnancy and no intrauterine pregnancy has a high probability of indicating ectopic pregnancy.
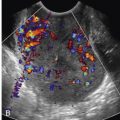
In most cases, the sonographic distinction between intraovarian and extraovarian mass is straightforward. In some cases, however, it is uncertain whether a mass is abutting the ovary or is within the ovary. A number of sonographic features of the mass have been suggested for making this important distinction, including its grayscale appearance, its Doppler characteristics, and its movement when pressure is applied by a transvaginal transducer.
One study found that a tubal ring of ectopic pregnancy is usually more echogenic than the ovarian parenchyma, whereas the echogenicity of a corpus luteum is generally less than or equal to that of the ovarian parenchyma. However, the comparison of these echogenicities is not definitive for distinguishing a tubal ring from a corpus luteum: in this series, 6 of 39 (15%) tubal rings were equal or lower in echogenicity than the ovary, whereas 3 of 45 (7%) corpora lutea were more echogenic than the ovary.
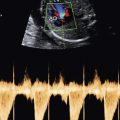
When assessed by Doppler, an adnexal mass of ectopic pregnancy typically has prominent flow on color Doppler and a low impedance pattern on spectral Doppler. When there is an adnexal mass indeterminate for being within, as opposed to abutting, the ovary, however, the presence of these Doppler characteristics in the mass does not reliably establish the diagnosis of ectopic pregnancy because a corpus luteum can have similar Doppler findings.
The most definite way to demonstrate that a mass abutting the ovary is extraovarian is to observe its motion relative to the ovary when pressure is applied by the transvaginal transducer. If the mass slides along the ovary, then it is extraovarian and the probable diagnosis is ectopic pregnancy (see Fig. 4-11 , ). If the mass and ovary move together, the mass is likely to be a corpus luteum within the ovary, and the probable diagnosis is intrauterine pregnancy. In an ultrasound facility that has the capability of storing video clips, it is good practice to store a clip of the adnexa while transducer pressure is applied.