Thyroid nodules can be detected in 4% to 8% of the adult population by palpation, but in 40% to 50% of the population by ultrasound. The overwhelming majority of these represent benign hyperplastic nodules or adenomas. Approximately 5% of nodules are malignant, with papillary carcinoma representing approximately 75% to 80% of primary thyroid malignancies. Although many sonographic features have been studied as a means of distinguishing benign from malignant nodules, ultrasound-guided fine-needle aspiration with cytologic evaluation remains a mainstay in the management of palpable and incidentally detected nodules. This article reviews the current techniques for sonographic evaluation of the thyroid and the imaging features of the various types of thyroid nodules.
Thyroid nodules are a ubiquitous clinical problem. In years past, when palpation was the sole method of thyroid evaluation, the prevalence of thyroid nodules was estimated at approximately 4% to 8% of the adult population and typically only those nodules 1 cm or larger in diameter were detected. With increasing use of imaging for evaluation of the carotid arteries, cervical spine, and chest, the reported prevalence of thyroid nodules has increased to as high as 40% to 50%, approaching the 50% prevalence of nodules found at autopsy. Because the risk for malignancy in these thyroid nodules is low (1.5%–10%), the issue of how best to manage the current epidemic of thyroid nodules in an increasingly cost-constrained environment is a critical one. Furthermore, the vast majority of the cancers detected are papillary carcinomas, which are often clinically occult and virtually never fatal even after spread to regional lymph nodes has occurred. A logical strategy for identifying the minority of thyroid nodules that require intervention from among the huge numbers that do not is a topic of much debate among sonographers and endocrinologists.
High-resolution ultrasound is the modality of choice for evaluation of the thyroid gland. It is painless, inexpensive, does not require the use of contrast media, and can display the internal architecture and flow characteristics of nodules as small as 1 to 2 mm. Ultrasound-guided fine-needle aspiration (FNA) with cytologic evaluation is now a mainstay in the management of palpable and incidentally detected nodules. This article reviews the current techniques for sonographic evaluation of the thyroid and the imaging features of the various types of thyroid nodules. We also explore the various strategies for management of thyroid nodules based on clinical and imaging parameters.
Anatomy and Scanning Technique
The thyroid gland is an H-shaped organ composed of two lobes joined by a narrow isthmus located just below the laryngeal cartilages. The normal thyroid weighs approximately 15 to 25 g, with each lobe approximately 4 cm in length and 2 cm in thickness. Befitting its vital role in metabolism, it is a highly vascular organ supplied by the superior thyroidal branch of the external carotid artery and the inferior thyroid branch of the subclavian artery. Microscopically, the thyroid parenchyma is organized into follicles, hollow spheres of epithelial cells enclosing a protein-rich material termed colloid. Thin fibrous septations divide the normal thyroid into lobules composed of 20 to 40 follicles each about 50 to 500 μm in size.
To visualize the thyroid gland optimally, the patient is placed in the supine position with a pillow underneath the shoulders to extend the neck slightly, allowing the head to rest on the examination table. In older patients or those who have degenerative changes in the neck, small towels can be placed under the head to the level where the patient is most comfortable while still allowing access to the neck. The thyroid gland is then imaged in transverse and longitudinal views with a high-frequency (10–15 MHz) linear transducer. The highest frequency is used while still allowing adequate sonographic penetration.
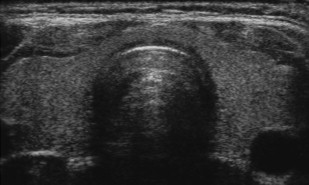
The normal thyroid gland is uniformly echogenic relative to the overlying strap muscles of the neck ( Fig. 1 ). A thyroid nodule is defined as a region of parenchyma sonographically distinct from the remainder of the thyroid and located within the confines of the echogenic thyroid capsule. When a nodule is detected, its size should be measured in three dimensions and the location within the thyroid gland (upper pole, mid-gland, lower pole) should be noted by the sonographer. Several sonographic features are helpful for differential diagnosis, including nodule echogenicity, morphology, cystic change, presence of echogenic foci with comet-tail artifact representing colloid, presence and type of calcifications, and flow pattern (peripheral or central). These are discussed in more detail later.
Instrumentation: New Technologies
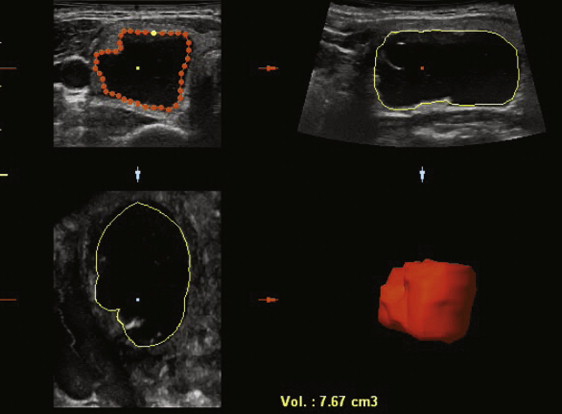
Several new sonographic technologies have been applied to the imaging of thyroid nodules. Three-dimensional (3D) ultrasound, in which a free-hand or automated sweep of the transducer generates an image volume that can be displayed in axial, coronal, or sagittal planes, can generate good-quality images of multinodular thyroids ( Fig. 2 ). In a recent study comparing volume measurements of thyroid nodules in 102 children, 3D ultrasound measurements were more accurate, with less intraobserver variability and higher reproducibility, compared with two-dimensional assessment. It may also provide greater workflow efficiency, because entire organs can be scanned in a single transducer sweep. Compound imaging is a signal-averaging technique designed to reduce speckle noise and improve contrast resolution, and has been shown to increase contrast-to-noise ratio in clinical thyroid images ( Fig. 3 ). Tissue harmonic imaging (THI) uses the first harmonic of the transmitted frequency for image formation and results in images with less noise. Its benefits in abdominal and pelvic sonography are dramatic, especially in obese patients. In a study of 144 patients who had thyroid nodules, THI improved lesion conspicuity and gray-scale contrast between lesions; however, the fundamental mode imaging was performed at 7.5 MHz, and therefore the relevance of this work is questionable given that most thyroid ultrasound is performed at 10 MHz or higher. Although these innovations have improved image clarity somewhat, they have not impacted lesion characterization significantly. Similarly, sonographic contrast agents have been used in other organ systems, but to date have not had a significant role in thyroid nodule imaging.
Elastography
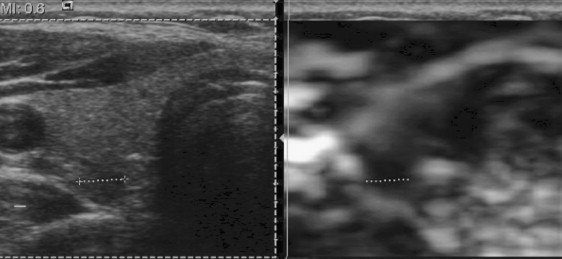
By contrast, elastography of thyroid nodules is an evolving technology with early reported promise of differentiating benign nodules from malignant nodules with 96% specificity and 82% specificity. Analogous to palpation, the rationale behind elastography is that a cancerous nodule is stiffer, with less elastic deformation compared with muscle or a benign thyroid nodule. Ultrasound elastography is a dynamic method in which an external compressive force is applied during scanning and the degree of distortion used to estimate the stiffness of the tissue of interest ( Fig. 4 ). Ultrasound elastography has already been used to differentiate cancer from benign lesions in the prostate, breast, pancreas, and lymph nodes. Different methods of identifying a stiff thyroid nodule are currently being studied, including manual compression with comparison of the lesion during a cine loop using speckle tracking in two and three dimensions, or with evaluation of the nodule under normal respiratory and cardiac pulsations. One recent study used carotid artery pulsation as the compression source and found that elastography was able to distinguish a papillary carcinoma from a benign nodule located in the same thyroid lobe. Although these implementations of elastography require off-line image processing, some newer machines are capable of real-time image processing. Recent work using a real-time elastography technique in 92 consecutive patients who had solitary thyroid nodules found that elastography scores representing the least strain (stiff lesions with little deformation) were highly predictive of malignancy with sensitivity of 97%, specificity of 100%, and 100% positive predictive value. The patients were highly selected, however, and cystic nodules, nodules with eggshell calcification, and patients who had multiple nodules were not included in the study. Although promising, elastography needs further study to determine whether the method will prove as robust when used on a larger scale.
Thyroid Nodules
Various benign and malignant nodules occur commonly in the thyroid gland ( Box 1 ). In the Framingham population study, nodules were found by palpation in 6.4% of women and 1.5% of men. By ultrasound, many more nodules are detected. In one study, 50% of patients who had apparent solitary nodules by palpation had additional nodules detected by ultrasound, and about 25% of those nodules were larger than 1 cm. Location of the nodule (anterior or posterior), size of the patient’s neck, and skill of the examiner all affect the likelihood of detection by palpation. With current ultrasound technology, however, even nodules as small as 1 mm may be evident.
Benign nodules
Colloid (hyperplastic, adenomatous) nodules
Hashimoto (chronic lymphocytic) thyroiditis
Cysts: colloid, simple, or hemorrhagic
Follicular adenomas
Hürthle-cell (oxyphil-cell) adenomas (variant of follicular adenoma)
Malignant nodules
Papillary carcinoma
Follicular carcinoma
Medullary carcinoma
Anaplastic carcinoma
Primary thyroid lymphoma
Metastatic carcinoma (breast, renal cell, others)
Hyperplastic Nodules
The most common lesion in the thyroid is the hyperplastic nodule, also termed a colloid or adenomatous nodule. The etiology of thyroid glandular hyperplasia includes iodine deficiency and disorders of hormone synthesis. Production of the thyroid hormones T3 and T4 (thyroxine) by thyroid follicle epithelial cells is regulated by release of thyroid-stimulating hormone (TSH) from the anterior pituitary gland. Impaired or deficient thyroid hormone synthesis causes TSH levels to increase, and increases in TSH then produce follicular cell hypertrophy and hyperplasia. Repetitive cycles of hyperplasia followed by involution may produce irregular thyroid enlargement and multinodular goiter. Otherwise identical-appearing follicular epithelial cells differ in their sensitivity to growth stimuli and in their intrinsic proliferative capabilities, which leads to nodule formation over time. It was formerly believed that hyperplastic nodules could be distinguished from true neoplasms by virtue of their polyclonality. More recent studies, however, suggest that both neoplasms and hyperplastic nodules are monoclonal. Despite their prevalence, therefore, the pathophysiology of thyroid nodule formation remains poorly understood.
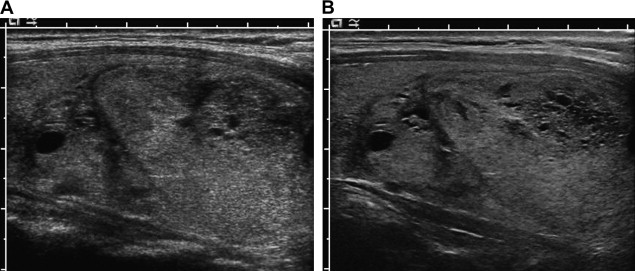
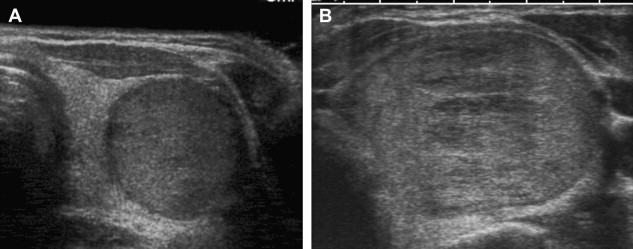
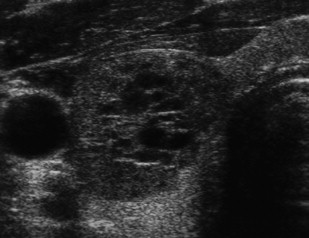
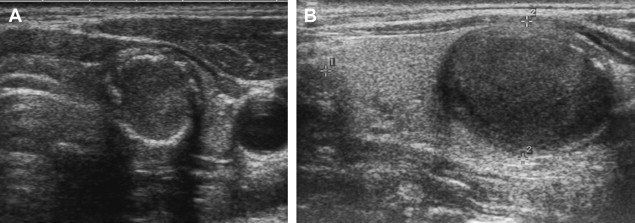
On sonography, hyperplastic nodules have a wide spectrum of appearances. They are most often isoechoic, but can also be hypoechoic and commonly undergo cystic and hemorrhagic degeneration ( Fig. 5 ). Larger solid masses may be entirely echogenic. Cystic areas may contain either serous fluid or colloid; old hemorrhage and resultant echogenic fluid may also be noted. Punctuate highly echogenic foci with ring-down artifact represent colloid crystals within colloid cysts ( Fig. 6 ). If residual strands of thyroid tissue remain within the cystic areas, a characteristic honeycomb appearance may result ( Fig. 7 ). Nonuniform patterns of degeneration may produce mural nodules, septations, or internal debris. Degeneration of hyperplastic nodules may also produce dystrophic calcification and manifest as either coarse internal calcification or peripheral “eggshell” calcification ( Fig. 8 ). The term goiter is used when hyperplasia leads to overall increase in the size of the thyroid gland. Multinodular goiter, which is composed of multiple hyperplastic nodules with varying degrees of colloid, necrosis, or hemorrhage, is generally heterogeneous in appearance with multiple masses of varying size and echo texture.

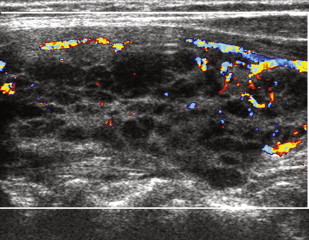
Hashimoto Thyroiditis
Hashimoto thyroiditis is a common autoimmune disease in which patients, predominantly women, develop antibodies to thyroglobulin and the thyroid peroxidase enzyme. It causes a characteristic sonographic pattern of innumerable tiny hypoechoic nodules that may become confluent, interspersed with echogenic fibrous bands ( Fig. 9 ). Vascularity may be increased, decreased, or normal, and FNA is usually not necessary for diagnosis.
Thyroid Nodules
Various benign and malignant nodules occur commonly in the thyroid gland ( Box 1 ). In the Framingham population study, nodules were found by palpation in 6.4% of women and 1.5% of men. By ultrasound, many more nodules are detected. In one study, 50% of patients who had apparent solitary nodules by palpation had additional nodules detected by ultrasound, and about 25% of those nodules were larger than 1 cm. Location of the nodule (anterior or posterior), size of the patient’s neck, and skill of the examiner all affect the likelihood of detection by palpation. With current ultrasound technology, however, even nodules as small as 1 mm may be evident.
Benign nodules
Colloid (hyperplastic, adenomatous) nodules
Hashimoto (chronic lymphocytic) thyroiditis
Cysts: colloid, simple, or hemorrhagic
Follicular adenomas
Hürthle-cell (oxyphil-cell) adenomas (variant of follicular adenoma)
Malignant nodules
Papillary carcinoma
Follicular carcinoma
Medullary carcinoma
Anaplastic carcinoma
Primary thyroid lymphoma
Metastatic carcinoma (breast, renal cell, others)
Hyperplastic Nodules
The most common lesion in the thyroid is the hyperplastic nodule, also termed a colloid or adenomatous nodule. The etiology of thyroid glandular hyperplasia includes iodine deficiency and disorders of hormone synthesis. Production of the thyroid hormones T3 and T4 (thyroxine) by thyroid follicle epithelial cells is regulated by release of thyroid-stimulating hormone (TSH) from the anterior pituitary gland. Impaired or deficient thyroid hormone synthesis causes TSH levels to increase, and increases in TSH then produce follicular cell hypertrophy and hyperplasia. Repetitive cycles of hyperplasia followed by involution may produce irregular thyroid enlargement and multinodular goiter. Otherwise identical-appearing follicular epithelial cells differ in their sensitivity to growth stimuli and in their intrinsic proliferative capabilities, which leads to nodule formation over time. It was formerly believed that hyperplastic nodules could be distinguished from true neoplasms by virtue of their polyclonality. More recent studies, however, suggest that both neoplasms and hyperplastic nodules are monoclonal. Despite their prevalence, therefore, the pathophysiology of thyroid nodule formation remains poorly understood.
On sonography, hyperplastic nodules have a wide spectrum of appearances. They are most often isoechoic, but can also be hypoechoic and commonly undergo cystic and hemorrhagic degeneration ( Fig. 5 ). Larger solid masses may be entirely echogenic. Cystic areas may contain either serous fluid or colloid; old hemorrhage and resultant echogenic fluid may also be noted. Punctuate highly echogenic foci with ring-down artifact represent colloid crystals within colloid cysts ( Fig. 6 ). If residual strands of thyroid tissue remain within the cystic areas, a characteristic honeycomb appearance may result ( Fig. 7 ). Nonuniform patterns of degeneration may produce mural nodules, septations, or internal debris. Degeneration of hyperplastic nodules may also produce dystrophic calcification and manifest as either coarse internal calcification or peripheral “eggshell” calcification ( Fig. 8 ). The term goiter is used when hyperplasia leads to overall increase in the size of the thyroid gland. Multinodular goiter, which is composed of multiple hyperplastic nodules with varying degrees of colloid, necrosis, or hemorrhage, is generally heterogeneous in appearance with multiple masses of varying size and echo texture.
Hashimoto Thyroiditis
Hashimoto thyroiditis is a common autoimmune disease in which patients, predominantly women, develop antibodies to thyroglobulin and the thyroid peroxidase enzyme. It causes a characteristic sonographic pattern of innumerable tiny hypoechoic nodules that may become confluent, interspersed with echogenic fibrous bands ( Fig. 9 ). Vascularity may be increased, decreased, or normal, and FNA is usually not necessary for diagnosis.