The advent of positron emission tomography (PET) and positron emission tomography–computed tomography (PET-CT) in the diagnostic imaging arena has revolutionized the field of oncology. During the greater part of the past decade, the unique property of PET scans, which yield functional or physiologic alterations, fused with CT scans, which reveal anatomic abnormalities, has produced hybrid PET-CT images. Fused PET-CTs in the setting of multiple solid tumors have been proven to have higher specificity, sensitivity, and accuracy in the early and accurate diagnosis of various neoplastic and inflammatory conditions compared with either modality alone. This chapter will discuss the technical aspects of PET and PET-CT imaging and provide a discussion of its role in the management of various gynecologic malignancies, with a current case-based literature review.
Gynecologic malignancy is the leading cause of cancer-related morbidity and mortality in women of all ages. Worldwide it accounts for approximately 20% of visceral cancers. In 2006, in United States alone, an estimated 76,515 women were newly diagnosed with gynecologic cancers, with nearly 28,115 of them dying from it; the mean age of death ranged from 48 years for cervical cancer to approximately 62 years for other gynecologic cancers. During the past 3 decades, the incidence and deaths related to gynecologic malignancies have decreased or stabilized, in part because of the robust efforts of various taskforces in providing preventive education and screening tests, but also in part because of advances in the role of medical imaging in the care of the cancer patient. Today more than ever, various diagnostic imaging tools are available for the cancer patient, allowing early detection and diagnosis and guiding appropriate medical and surgical therapy.
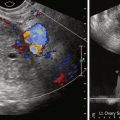
Most gynecologic cancers are staged clinically using the International Federation of Gynecologic and Obstetrics (FIGO) staging scheme. The use of conventional cross-sectional imaging modalities such as Doppler ultrasound (US), multidetector row computed tomography (MDCT or CT), and magnetic resonance imaging (MRI) in the diagnosis, staging, detecting recurrence, monitoring therapy, and long-term surveillance has shown great benefit in improving the care and outcome of the cancer patient. The role and utility of PET and PET-CT as adjuncts to conventional imaging in managing these patients has been an evolutionary process during the past decade that has shown significant clinical benefits. Unlike MDCT and MRI, which use the physical principles of transmission radiation and nuclear magnetic resonance, respectively, to provide exquisite multiplanar anatomic data sets of the body, PET and PET-CT imaging techniques primarily rely on the body’s physiologic processes. The unique property of the PET imaging agents or radioactive isotopes is that they are injected intravenously into the patient, subsequently undergo radioactive decay via an emission process, and thereby allow the detection and spatial localization of a focal aberrant or altered physiologic process (e.g., malignant or inflammatory). In essence, tumors or inflammatory processes that are visualized by fluorodeoxyglucose (FDG)-PET have glucose metabolic rates that are greater than surrounding normal cells. A transmission CT scan for attenuation correction, known as ACCT, is obtained in the same imaging session to help more accurately anatomically localize the region or focus of abnormal glucose metabolism on the corresponding PET scan. Thus a PET-CT scan combines both functional and anatomic information into a single fused data set from sequential acquired PET and CT examinations.
Although there has been substantial contribution in patient management, the utility of FDG-PET imaging in patients with gynecologic cancers is a process in evolution. The majority of the work in this arena has been done in patients with cervical cancer at initial staging, in detecting recurrence, and in monitoring therapy response. The use of PET and PET-CT in patients with ovarian cancer has been evaluated to a lesser degree, primarily in offering value in the surgically treated patient who presents with abnormal biomarkers despite a clinically benign evaluation and either a negative or inconclusive result of conventional imaging (US, MDCT, or MRI) workup. The utility of PET for other gynecologic cancers such as endometrial cancer, uterine sarcomas, vulvar cancers, and vaginal and fallopian tube cancers is less well defined and investigational.
Technical Considerations
Forming the Positron Emission Tomography Image
PET and PET-CT are three-dimensional (3D) nuclear medicine techniques that form the cornerstone of modern oncologic imaging. FDG, also referred to as 18-fluorodeoxyglucose, has a half-life of approximately 120 minutes and is currently the most ubiquitously available PET radiotracer agent in routine clinical practice. It is a glucose analog comprising a glucose molecule that has its second hydroxyl group substituted with a radioactive isotope F-18. Figure 31-1 illustrates the FDG molecule. Once injected intravenously into the patient, it competes with the glucose molecule to gain entry into cells via a number of cellular membrane glucose transporter proteins, also known as Glut proteins. Cancer and inflammatory cells, by their very nature, commonly overexpress these Glut proteins, thereby inherently having a relatively increased glucose or FDG avidity compared with other normal cells. Once intracellular the FDG molecule undergoes phosphorylation into FDG-6-phosphate (FDG-6-P). Unlike glucose-6-phosphate (G-6-P), the FDG-6-P molecule is “metabolically” trapped in the cell, neither able to undergo the normal glycolytic processing of G-6-P, nor able to be converted into a form that can exit the altered cell. Figure 31-2 illustrates the concept of “metabolic trapping.” Over time the accumulated intracellular F-18 (of the FDG molecule) undergoes radioactive decay via an annihilation reaction, resulting in emission of a pair of positrons emitted at 180 degrees. These emitted photons reach the detectors of the PET scanner by the process of coincidence detection. These events are registered, analyzed, and their origin localized by a computer. When a predetermined number of events or counts have been obtained, the information is formed into a PET image. Figure 31-3 is a pictorial representation of how the PET image is formed. Today, almost invariably, an accompanying ACCT scan is virtually always concurrently obtained in the same session after the PET scan. The ACCT is a non–intravenous contrast, low-dose transmission map, the primary purpose of which is to help accurately localize the origin of the abnormal FDG avid cell(s) or region. With the fusion of the PET scan and ACCT scan, an FDG PET-CT scan is created. Figure 31-4 shows examples of a PET, ACCT, and fused PET-CT image.




Patient Preparation
As with conventional imaging examinations, proper patient preparation, routine scanning protocols, and standard interpretation are vital components for optimal diagnostic accuracy of a PET-CT examination. Considerations specific to FDG PET-CT scans include additional measures to reduce artifact from inadequate bowel preparation, abnormal blood glucose levels, and excessive residual urinary bladder activity. Typically the patient is instructed to fast for 6 hours before the FDG PET-CT scan. A preprocedure blood glucose level is obtained to ensure a nonhyperglycemic state (<200 mg/dL)—hyperglycemic states result in scans with the majority of the FDG activity shunted away to the brain, heart, and the skeletal muscles. Patient hydration can be achieved with 1000 to 1500 mL of 0.9% isotonic saline intravenously. One hour before the scan, a weight-based dose of FDG (≈350 to 400 MBq) is administered intravenously. Thereafter the patient is placed in a quiet dimly lit room and instructed to avoid excessive talking, chewing, or any muscular activity. Depending on institutional guidelines, an oral contrast agent is administered approximately 30 minutes before the PET-CT scan to distend the bowel. At our institution, we routinely use 900 mL of a negative oral contrast agent (VoLumen; E-Z-EM Inc, Westbury, NY) because in our experience the use of a negative oral contrast agent (vs. a positive oral contrast agent) reduces artifacts related to the gastrointestinal tract. At some institutions, intravenous furosemide is administered approximately 20 minutes after FDG injection to help with diuresis. When a PET scan is obtained to evaluate known or suspected gynecologic malignancies, the patient is asked to completely void just before the scan—FDG is excreted in the urine, and the accumulation of FDG activity in the urinary bladder can obscure pelvic findings in these patients. Occasionally it is advantageous to catheterize the urinary bladder before the scan for continuous bladder irrigation.
Scanning
A PET-CT scan is obtained sequentially. The initial examination is a free breathing attenuation correction CT (ACCT) scan that is typically obtained from skull base to mid-thigh, with the patient in supine position with arms overhead. Thereafter the PET scan is obtained in a thigh to skull direction with a matching field of view (FOV) and coverage, with multiple table position stops for data acquisition. The two scans are postprocessed, and then a fused FDG PET-CT data set is formed. The scans are typically available for interpretation in multiplanar reformats (axial, coronal, and sagittal planes) at various CT window settings (such as lung, soft tissue, and bone). At most institutions each individual scan can be viewed separately or together, with both the attenuation corrected and noncorrected PET images also available to sort out artifacts related to image acquisition, misregistration, or artifacts from metal in the body. In many instances, a diagnostic contrast-enhanced MDCT is concomitantly obtained at clinical request.
Interpretation
In general, it is imperative for the PET-CT scan interpreter to be familiar with the pattern of normal and nonmalignant FDG distribution in the body to help reduce interpretive errors. Once injected intravenously, FDG distributes via the bloodstream to all glycolitically active tissues, normal and abnormal. Scanning is typically obtained 60 minutes after injection because this allows for sufficient FDG blood activity clearance and optimizes the target-to-background detection.
Physiologic FDG uptake is most striking in the brain and heart, with less intense uptake in the liver, spleen, bone marrow, the hollow bowel, muscles, and ovaries/testes, and yet lower blood pool uptake in the mediastinum. Because FDG is excreted via the kidneys, intense activity is normally seen in the kidneys and collecting system, the ureters, and the urinary bladder. Scanning the hyperglycemic patient significantly decreases the examination sensitivity as a result of physiologic shunting of glucose (and FDG) to the brain, heart, and skeletal muscles. On occasion symmetric activity can be seen in metabolically active brown adipose or brown fat, as well as in various benign infectious or inflammatory conditions, such as abscess, wounds, bowel pathology, advanced degenerative changes, and healing fractures. Specific to female pelvis imaging, in premenopausal women there can be physiologic uptake in the ovaries, uterus, and endometrium, particularly during the menstrual phase. In the postmenopausal woman, however, increased ovarian FDG uptake is much less likely to be caused by a benign process and warrants further investigation. Various other nonmalignant processes in the female pelvis, such as endometriosis and fibroids, have been shown to take up FDG. Table 31-1 shows common viscera of physiologic FDG uptake.
| Normal Viscera | Excreted Fluorodeoxyglucose |
|---|---|
| Brain | Kidneys |
| Heart | Ureter |
| Skeletal muscle | Urinary bladder |
| Blood vessels | |
| Bowel | |
| Salivary glands | |
| Thyroid | |
| Endometrium | |
| Testes and ovaries |
Although a visual qualitative assessment of PET images is generally satisfactory for routine clinical work, a semiquantitative value known as the standard uptake value (SUV) can be obtained and reported. Although dependent on multiple physiologic and instrumentation variables, the SUV provides a ratio of the concentration of FDG in the tumor compared with the average concentration of FDG in the body. In general a maximum SUV cutoff value of 2.5 is used to help differentiate normal from abnormal (e.g., neoplastic and inflammatory) processes. In many instances use of a maximum SUV value is considered useful in assessing therapy response.
Gynecologic Malignancies
Cervical Cancer
The incidence and mortality rates of cervical cancer in the United States have sharply decreased since the institution of the Papanicolaou (Pap) smear, with 11,270 reported new cases and 4070 reported deaths in the United States in 2009. Worldwide, however, it remains the third most common cancer and the second most common cause of cancer death in developing countries. The most common histology of cervical carcinoma is squamous cell cancer (69%) and adenocarcinoma (25%), with the remainder less prevalent adenosquamous carcinoma, neuroendocrine tumors, rhabdomyosarcoma, primary lymphoma, and sarcoma. The local staging of small cervical cancers is on a clinical basis using the FIGO staging system. The role of PET imaging is reserved for detecting local extent of disease and for evaluating lymphatic and systemic spread. Figure 31-5 is a case of FDG PET-CT in advanced cervical carcinoma.