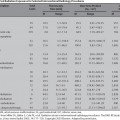
7 Uterine Fibroid Embolization and Infertility Gary P. Siskin Since the first reports of utilizing uterine fibroid embolization (UFE) as a treatment for symptomatic uterine fibroids surfaced in the early 1990s, this procedure has gained both acceptance and popularity as a nonsurgical alternative used to manage this condition. As the success of UFE in addressing fibroid-related symptoms has been established, more women have been asking their gynecologist, primary-care physician, and interventional radiologist about UFE and its potential role in their care. This includes patients who express a desire to preserve future fertility options. Therefore, most interventionalists with active UFE practices are facing decisions regarding the appropriate management of a patient with fibroids who has stated her desire to either definitely or possibly have a child in the future. To provide guidance for the interventionalists facing this dilemma in everyday practice, it is important to recognize that these patients typically fall into three very different categories characterized by the objectives of the patients. The first category includes patients who have fibroids and wish to preserve their fertility options, but do not have definite plans to have a child in the immediate future. The second category includes patients with fibroids who have definite plans for childbearing in the immediate future. Finally, the third category includes patients with fibroids who have been experiencing difficulties in becoming pregnant or carrying a pregnancy to term. The purpose of this chapter is to provide recommendations regarding the role that UFE may play in the care of all of these patients based on a current review of the literature regarding fertility issues in patients with fibroids and fertility preservation after procedures used to treat symptomatic uterine fibroids.1 Infertility is a problem affecting many women and many couples in today’s world. Based on the 2002 National Survey of Family Growth, 7.4% of married women (~2.1 million women) were infertile and 12% of women aged 15 to 44 (~7.3 million women) had difficulty getting pregnant or carrying a baby to term.2 Classically, infertility has been defined as a failure to conceive after one year of failed intercourse. With this definition in mind, however, only a minority of patients are considered to have true infertility because they can only conceive and successfully carry a pregnancy with medical assistance. These patients may have conditions such as occluded fallopian tubes, an absent uterus, absent ovarian follicles, or male partners with an inability to produce sperm. The remaining patients can be considered subfertile because there is a chance that conception could happen without medical intervention. However, fertility treatment is often recommended for these patients if it is felt that treatment can improve their situation and increase the odds of conception. There is no consensus about the impact of uterine fibroids on female subfertility.3 It is known that fibroids are present in 5 to 10% of infertility patients and may be the sole factor identified in 1 to 2.5% of patients. However, the exact role that fibroids play in recurrent pregnancy loss and infertility is uncertain. This is because it has been historically difficult to assess the direct impact of fibroids on fertility due to the following: the incidence of fibroids increases with age, fertility declines with age, and many women with fibroids conceive spontaneously. That said, there are anatomic and physiologic factors attributed to the presence of uterine fibroids over the years, which may contribute to subfertility in this patient population.4–8 As a space-occupying lesion, fibroids can be responsible for anatomic changes that can lead to subfertility, including distortion of the endometrial cavity, obstruction of the tubal ostia or cervical canal, and displacement of the cervix within the vagina. Physiologically, fibroids also have the potential to impair uterine contractility and impair implantation due to endometrial vascular disturbances resulting in inflammation, ulceration, thinning, and atrophy. The problem that is considered by most to be responsible for fibroid-related subfertility is the distortion of the endometrial cavity because it can create an abnormal site for placental implantation which, in turn, can lead to increases in the rate of both spontaneous abortion and premature labor. This is why fibroid location and size are often the most important factors in determining the impact of fibroids.3 Because of this, few dispute the fact that submucosal fibroids or intramural fibroids, which have a submucosal component, influence pregnancy rates. Even this, however, is controversial in the obstetrics-gynecology literature. When looking at this issue in the context of assisted reproductive technologies (such as in-vitro fertilization, intracytoplasmic sperm injection, etc.), some investigators have found that intramural and/or subserosal fibroids do not affect the outcome of these procedures.9–11 Others, however, have found that even small intramural fibroids that do not distort the endometrial cavity have a significant effect on pregnancy, implantation, and ongoing pregnancy rates.11–14 This debate has led to differences regarding which patients should undergo treatment for fibroids, such as myomectomy, prior to attempts with assisted reproductive techniques.15,16 Given the importance of fibroid-related distortion of the endometrial cavity, one of the first steps that an interventional radiologist can take when evaluating a patient with fibroids and fertility concerns is to participate in the imaging evaluation of these patients and render an opinion as to whether or not the fibroids may be contributing to subfertility. Therefore, patients who have had fertility problems or wish to preserve fertility options after treating their fibroids should undergo an imaging evaluation of their endometrial cavity to determine the anatomic relationship between the fibroids and the cavity. There are many imaging tests that can potentially answer this question, including transvaginal ultrasound, sonohysterography, hysterosalpingogram, and hysteroscopy.17–19 In addition, pelvic MRI, which is growing in importance as the imaging modality of choice before and after UFE, can provide this information as well.20,21 At the very least, MRI will provide the information necessary to determine if the fibroids are distorting the endometrial cavity and if any other conditions are present that may explain infertility. MRI can also help determine if a patient is a candidate for myomectomy based on the size, number, and position of their fibroids. Once the fertility status of a patient is known and her childbearing plans have been discussed, an interventional radiologist can utilize the available imaging data and confer on the patient’s treatment options. At the present time, a review of available literature supports the position that myomectomy is the preferred treatment option for a patient with symptomatic uterine fibroids and a desire to preserve fertility options. In 1998, Vercellini et al22 performed a comprehensive review of the literature that estimated the effect of abdominal myomectomy on infertility. Twenty-three studies were reviewed, all of which were noncomparative. The pregnancy rate after myomectomy, based on 138 patients, was 57%; the conception rate ranged from 58 to 65% in patients with intramural and/or subserosal fibroids. This rate was similar to that found by Campo et al,23 who evaluated 41 patients with intramural or subserosal patients and found a conception rate of 61%; Marchionni et al24 in their evaluation of 72 patients with intramural or subserosal fibroids found a conception rate of 70%. Importantly, Campo et al found that myomectomy was associated with a decrease in the rate of miscarriage from 57.1% to 13.9%, which was similar to the decrease in miscarriages from 69% to 25% found by Marchionni et al.23,24 Vercellini also found a conception rate ranging from 53 to 70% in patients with only submucosal fibroids.22 This was similar to that reported by Shokeir et al25 who found a 72.4% pregnancy rate after a hysteroscopic myomectomy was performed on 29 patients with submucosal fibroids. Similarly, they found that the miscarriage rate had dropped from 62% to 26% after myomectomy. Despite the fact that there are a reasonably large number of studies available that have reported increases in conception and pregnancy rates and decreases in miscarriage rates, there remain differences of opinion regarding the role that myomectomy should play in patients with fibroids and a desire for fertility preservation. For example, in her 2001 review of fibroids and infertility, Pritts4 stated that the only analysis of myomectomy outcomes stratified by location was for women with submucosal fibroids, with results supporting the use of myomectomy for these patients. However, given the lack of data suggesting a cause and effect relationship between intramural and subserosal fibroids and infertility, and given the potential complications of myomectomy, she felt that the use of myomectomy for these patients may be unjustified.4 This differs from the data of Campo et al, who found that performing a myomectomy in patients with subserosal and/or intramural fibroids does help to improve pregnancy rates.24 Therefore, although there certainly does seem to be data supporting the use of myomectomy in patients with symptomatic fibroids desiring future childbearing, this data certainly seems to leave room for questions and differences of opinion. It may also open the door for a possible role for UFE in the care of these patients. As more interventional radiologists are performing UFE procedures on patients with symptomatic fibroids who desire future fertility, the number of reports and studies commenting on the successes and failure of this approach has increased. There are, at the present time, several case reports26–35 and clinical studies36–42 that support the observation that patients can become pregnant and carry a pregnancy to term after UFE. The outcomes of these clinical studies are summarized in Table 7.1. These reports all enable an interventional radiologist to say that patients can successfully conceive and deliver a healthy baby after UFE is performed. Although not exactly a quantitative statement, this is meaningful given the definitive early warnings against UFE in this patient population that were issued by the American College of Obsetetrics and Gynecology in 200043 and the inclusion of “desire to maintain childbearing potential” on the list of relative contraindications to UFE by the Society of Interventional Radiology in their Quality Improvement Guidelines prepared in 2004.44
Infertility and Uterine Fibroids
Review of the Literature on Uterine Fibroid Treatment and Future Fertility
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree