Functions
• Special visceral efferent (SVE). Branchial motor to pharyngeal and laryngeal muscles, including palatoglossus.
• General visceral efferent (GVE). Visceral motor (parasympathetic) to smooth muscles and glands of pharynx (via pharyngeal plexus), larynx, heart, esophagus, stomach, and other thoracoabdominal viscera down to the splenic flexure.
• General sensory afferent (GSA). Somatic sensory from ear, external auditory meatus, external surface of the tympanic membrane, dura of posterior cranial fossa, larynx.
• Visceral afferent (VA). Visceral sensory from pharynx, larynx, trachea, lungs, heart, esophagus, stomach, other thoracoabdominal viscera down to the splenic flexure, aortic arch baroreceptors, aortic body chemoreceptors.
• Special afferent (SA). Special sensory for taste from the epiglottis, hard and soft palates and pharynx.
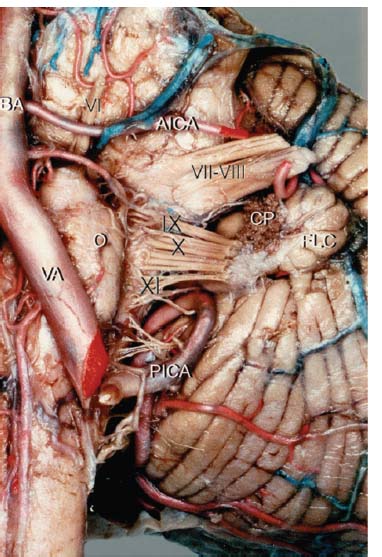
Fig. 10.1 Anterior view of the left cerebellopontine angle showing the origin of CN X at the postolivary sulcus of the medulla. (AICA, anterior inferior cerebellar artery; BA, basilar artery; CP, choroid plexus; FLC, flocculus; O, olive; VA, vertebral artery; Roman numerals, cranial nerves.) (From Ozveren MF, Ture U, Ozek MM, et al. Anatomic landmarks of the glossopharyngeal nerve: a microsurgical anatomic study. Neurosurgery 2003;52:1400–1410. Reprinted with permission.)
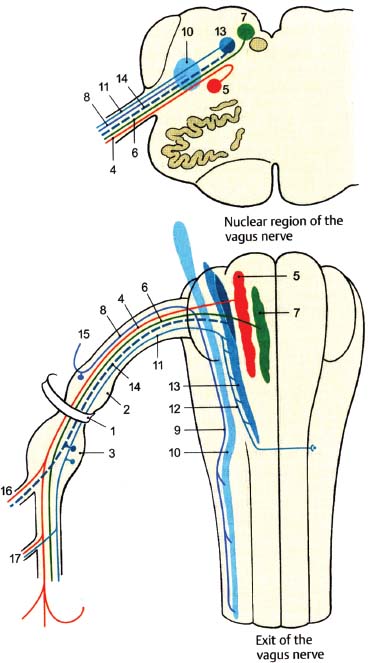
Fig. 10.2 Vagus nerve: nuclear region and exit. (1, jugular foramen; 2, superior ganglion [jugular ganglion]; 3, inferior ganglion [nodose ganglion]; 4, branchial motor fibers; 5, nucleus ambiguus; 6, parasympathetic fibers; 7, dorsal motor nucleus of CN X; 8, somatic sensory fibers; 9, spinal trigeminal tract; 10, spinal trigeminal nucleus; 11, visceral sensory fibers; 12, tractus solitarius; 13, nucleus solitarius; 14, special sensory [taste] fibers; 15, auricular branch; 16, pharyngeal branches; 17, superior laryngeal nerve.)
• The vagus nerve leaves the medulla between the olive and the inferior cerebellar peduncle (postolivary sulcus) as eight to 10 rootlets that traverse the cerebellomedullary cistern and converge into a single trunk to exit the skull via the jugular foramen (Figs. 10.1, 10.2). In the jugular foramen, it lies in the posterior part (pars vascularis) along with cranial nerve (CN) XI (Fig. 10.3).
• The superior (jugular) ganglion (~2.5 mm in length) lies within the jugular foramen, where it is joined by the accessory nerve (CN XI). The jugular ganglion contains cell bodies of sensory neurons that convey primarily somatic sensory (GSA) information.
• From the jugular ganglion CN X gives off the meningeal ramus (meningeal branch) and the auricular ramus (auricular branch or Arnold’s nerve) (see the section Distinct Branches of the Vagus Nerve).
• Following its exit from the jugular foramen, CN X enlarges into a second ganglion, the inferior (nodose) ganglion (~2.5 mm in length). The nodose ganglion primarily conveys visceral (VA) and special sensory (SA) information.
• The main trunk of the vagus nerve then descends into the neck, traveling in the carotid sheath with the internal carotid artery (ICA) and the internal jugular vein (IJV), and gives off the recurrent laryngeal and superior cardiac branches.
• The vagus nerve then enters the thorax, crossing over the subclavian artery on the right side and traveling between the common carotid and subclavian arteries on the left side. In the posterior mediastinum, both vagus nerves send fibers to pulmonary and esophageal plexuses. They then enter the abdomen via the esophageal opening of the diaphragm (left anterior to esophagus, right posterior), and terminate in the abdominal viscera.
Distinct Branches of the Vagus Nerve (Fig. 10.4)
Jugular Fossa
• Meningeal ramus (meningeal branch). GSA. Arises from the jugular ganglion, provides sensory innervation to the dura mater of the posterior cranial fossa.
• Auricular ramus (auricular branch, Arnold’s nerve). GSA. Arises from the jugular ganglion, enters the mastoid canaliculus on the lateral wall of the jugular fossa, traverses the temporal bone, and passes through the tympanomastoid fissure between the mastoid process and the tympanic part of the temporal bone. It provides sensory innervation to the ear (posterior pinna), external auditory meatus, and external surface of the tympanic membrane.
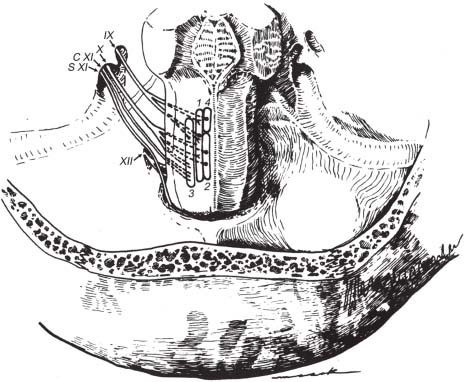
Fig. 10.3 Origin and cisternal courses of glossopharyngeal, vagus, spinal accessory, and hypoglossal nerves. Note that the glossopharyngeal nerve passes through the more anterior part of the jugular foramen (pars nervosa), whereas the vagus and spinal accessory nerves pass through the posterior part (pars vascularis) . The hypoglossal nerve passes through the more inferiorly located hypoglossal canal. (1, nucleus solitarius; 2, dorsal motor nucleus of CN X; 3, nucleus ambiguus; 4, superior salivatory nucleus; C XI, cranial root of CN XI; S XI, spinal root of CN XI.) (From Harnsberger HR. Handbook of Head and Neck Imaging (2nd ed.) St. Louis, MO: Mosby, 1995. Reprinted with permission.)
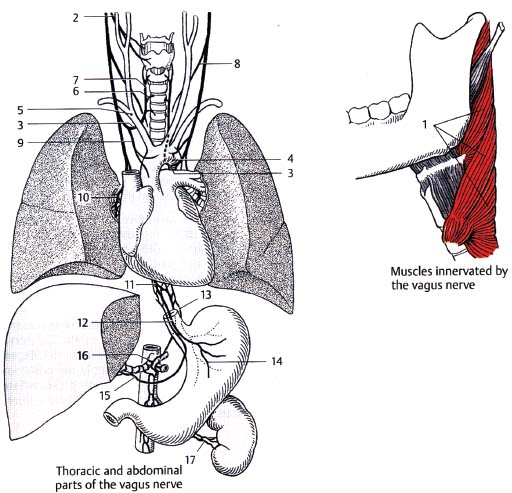
Neck
• Pharyngeal ramus. SVE. Arises from the nodose ganglion, divides into filaments to form pharyngeal plexus with branches of CN IX and external laryngeal nerve (see below). Supplies all the muscles of the pharynx and soft palate except stylopharyngeus (CN IX) and tensor veli palatini (CN V), including the superior and middle pharyngeal constrictors, levator veli palatini, salpingopharyngeus, palatopharyngeus, and palatoglossus.
• Superior laryngeal nerve. SVE and GSA. Arises just below the nodose ganglion, descends on the side of the pharynx, and divides into the internal and external laryngeal nerves. External branch (external laryngeal nerve, smaller, SVE) supplies the inferior pharyngeal constrictor and cricothyroid muscles and communicates with the pharyngeal plexus and superior cardiac branches. The internal branch (internal laryngeal nerve, larger, GSA) pierces the thyrohyoid membrane along with the superior laryngeal artery and sends sensory fibers to the epiglottis and mucous membranes of the larynx above the vocal folds.
• Recurrent laryngeal nerves (at base of neck). SVE and GSA. The right recurrent laryngeal nerve (RLN) arises in front of the subclavian artery and bends upward and medially behind the subclavian artery to ascend in the right tracheoesophageal sulcus. The left RLN arises to the left of the aortic arch and loops beneath the ligamentum arteriosum before ascending in the left tracheoesophageal sulcus. Each nerve passes under the inferior constrictor and enters the larynx. The RLNs supply all the intrinsic laryngeal muscles except the cricothyroid (supplied by the external laryngeal ramus of the superior laryngeal nerve, the cricothyroid swings the thyroid cartilage forward, thereby tensing vocal ligaments and increasing pitch). These include the lateral cricoarytenoid (draws vocal folds together, closes glottis), posterior cricoarytenoid (draws vocal folds apart, opens glottis, deepens pitch), and vocalis (fine adjustments in tension of vocal ligaments). RLNs also supply GSA to the vocal cords and the subglottis, and communicate with the cardiac plexus.
• Superior cardiac branches. Several (2–3) branches arising from vagus in the neck, which follow the ICA to the aorta to supply the cardiac plexus.
Thorax
• Inferior cardiac branches. Arise from the vagus at the side of the trachea, and from the RLN. Supply the cardiac plexus.
• Anterior bronchial branches. Small branches join with sympathetic filaments to form the anterior pulmonary plexus.
• Posterior bronchial nerve. Larger branches join with sympathetic filaments from thoracic ganglia to form the posterior pulmonary plexus.
• Esophageal branches. Ramify with branches from the opposite side to form the esophageal plexus.
• Gastric branches. The right vagus forms the posterior gastric plexus (postero-inferior surface of stomach) and the left vagus forms the anterior gastric plexus (anterosuperior surface).
• Celiac branches. From the right vagus, join the celiac plexus.
• Hepatic nerve. From the left vagus, join the hepatic plexus.
Functional Pathways of the Vagus Nerve
• SVE (branchial motor) pathway. Nucleus ambiguus (in medullary reticular formation medial to spinal trigeminal nucleus) supplies striated musculature of soft palate, pharynx (including pharyngeal constrictors), and larynx (via CN IX, X, and bulbar XI). Supranuclear innervation to the nucleus ambiguus is via corticobulbar fibers originating in the lower precentral gyri (bilateral innervation) and traveling in the genu of the internal capsule.
• GVE (visceral motor) pathway. Parasympathetic (GVE) outflow arises from dorsal motor nucleus of CN X (located in the floor of the fourth ventricle in the vagal trigone lateral to the hypoglossal nucleus). Input to the dorsal motor nucleus of CN X is from the hypothalamus, olfactory system, reticular formation, and nucleus solitarius. Sends preganglionic parasympathetics via the vagus nerve to the thorax and abdomen, innervating abdominal viscera up to the splenic flexure. Secretomotor innervation to pharyngeal mucosa (via pharyngeal plexus), laryngeal mucosa, ganglia in walls of individual thoracic organs, and esophageal, gastric, celiac, and hepatic plexi. Selective vagotomy involves partial severing of the right and left gastric nerves to treat persistent/recurrent gastric ulcers. Vagal intestinal branches increase peristalsis and secretion in small intestine, cecum, vermiform appendix, ascending colon, and transverse colon to splenic flexure. Synapses occur in the ganglia of the myenteric (Auerbach’s) plexus and submucosal (Meissner’s) plexus.
• GSA (somatic sensory) pathway. Somatic sensation from ear, external auditory meatus, tympanic membrane (via Arnold’s nerve) and posterior fossa dura (via meningeal branch) to jugular ganglion to spinal trigeminal nucleus.
• VA (visceral sensory) pathway. Visceral afferent sensations from pharynx, larynx, trachea, lungs, heart, esophagus, stomach, thoracoabdominal viscera down to the splenic flexure, aortic arch baroreceptors, and aortic body (chemoreceptors) travel via vagal branches to nodose ganglion to tractus solitarius and caudal nucleus solitarius.
• SA (special sensory) pathway. Taste information from the epiglottis, hard and soft palates, and pharynx travels to nodose ganglion to rostral nucleus solitarius.
• Nucleus solitarius (also sometimes called nucleus of the solitary tract). Rostral nucleus solitarius is gustatory with input mainly from CN VII (geniculate ganglion) and CN IX (petrosal ganglion), but also from CN X. Caudal nucleus solitarius is mainly for visceral sensation (carotid body and carotid sinus from CN IX, and visceral sensation from CN X). Efferent fibers from nucleus solitarius are distributed to thalamic ventroposteromedial nucleus (VPM) (via central tegmental tract), salivatory nucleus (for salivation with taste stimulation), dorsal motor nucleus of CN X (for increased peristalsis), nucleus ambiguus, and hypoglossal nucleus.
• Medullary respiratory center. Includes nucleus ambiguus, nucleus solitarius, and the medullary reticular formation. Responds to vagal input and CO2 accumulation (via carotid body (CN IX) and aortic arch (CN X) chemoreceptors). Medullary vasomotor center is less well defined anatomically.
Vagus Nerve: Normal Images (Figs. 10.5, 10.6, 10.7, 10.8, 10.9, 10.10)
Vagus Nerve Lesions
Evaluation
• Sensory evaluation. Difficult to assess separately from other CNs for both somatic sensation (larynx, pharynx, pinna, meninges) and taste (epiglottis) as there is considerable overlap with CNs VII and IX.
• Motor evaluation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree