Vascular Lesions
Vascular lesions of bone constitute a spectrum of pathologic entities. These range from congenital vascular malformations, that is, errors of morphogenesis with nonproliferative capacity, which growth is parallel with growth of the patient (such as angiomatosis), to benign neoplasms that may be present at birth, and to highly malignant tumors that widely metastasize and have a low survival rate (such as angiosarcoma). In the past decade, immunohistochemistry studies have been conducted in attempts to discriminate between malformations and true tumors. The formers have been found to be negative for WT1 (a transcription factor initially isolated from a hereditary Wilms tumor encoded by the so-called Wilms tumor 1 [WT1] gene) and GLUT1 (an erythrocyte-type glucose transporter protein not present in normal vasculature and vascular malformations but found at sites of blood-tissue barriers and in vascular tumors). Furthermore, some investigators found somatic mutations in genes coding for the receptors VEGFR2 and VEGFR3 of the vascular endothelial growth factors, which play an important role in angiogenesis and vascular formation.
Benign vascular lesions are of either endothelial or pericytic origin. The first group includes hemangiomas, cystic angiomatosis, Gorham disease of bone, lymphangiomas, and lymphangiomatosis. The second group includes glomus tumor and its variants, glomangioma and glomangiomyoma. Hemangiomas are classified according to the type of vessels in the lesion as capillary, cavernous, venous, and mixed. Diffuse involvement of bones by hemangiomatous lesions is defined as hemangiomatosis or angiomatosis. When bone is extensively involved, particularly if there is formation of intramedullary cystic lesions, the term cystic angiomatosis is applied. Gorham disease of bone, also known as massive osteolysis, phantom bone disease, or disappearing bone disease, is characterized by progressive, localized bone resorption, probably caused by multiple or diffuse cavernous hemangiomas or lymphangiomas of bone or both. Lymphangioma is a rare disorder consisting of the lesion composed of sequestered, noncommunicating lymphoid tissue lined by lymphatic endothelium. Glomus tumor and its variants are rare lesions composed of rounded uniform cells often arranged in a brickwork-like pattern.
The locally aggressive and malignant tumors are quite uncommon and are mostly of endothelial origin, such as hemangioendothelioma and angiosarcoma. The existence of hemangiopericytoma as a distinct tumor is still a matter of debate. World Health Organization (WHO) classifies this lesion in the category of fibrous tumors changing its name to “myopericytoma.”
A. BENIGN VASCULAR LESIONS
Intraosseous Hemangioma
Definition:
Hemangioma is a benign lesion composed of newly formed blood vessels of capillary or cavernous type.
Epidemiology:
Wide age distribution, ranging from the first to eighth decade of life, with nearly 70% of the cases diagnosed in patients between 30 and 60 years.
They are rare in newborns and infants, and in reported cases, they have arisen in the skull bones.
There is no sex predilection.
The lesions are usually solitary, although multifocal involvement has been described (most commonly in the vertebral column).
Sites of Involvement:
Craniofacial bones, predominantly calvaria (frontal and parietal regions)—50%, followed by the spine—20%.
Clinical Findings:
Commonly asymptomatic.
In the vertebrae may cause neurologic symptoms.
Imaging:
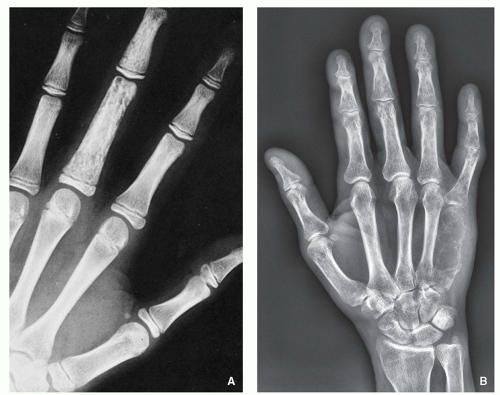
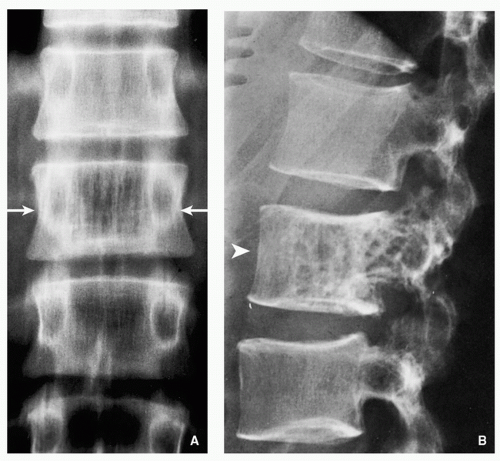
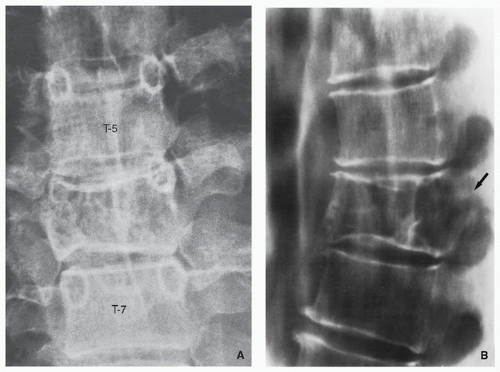
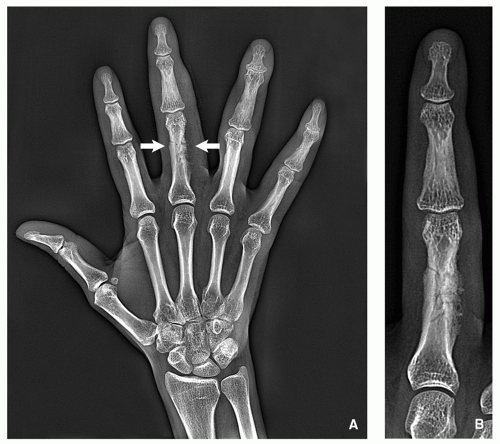
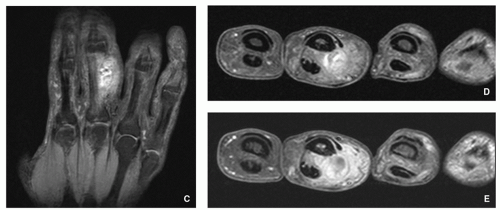
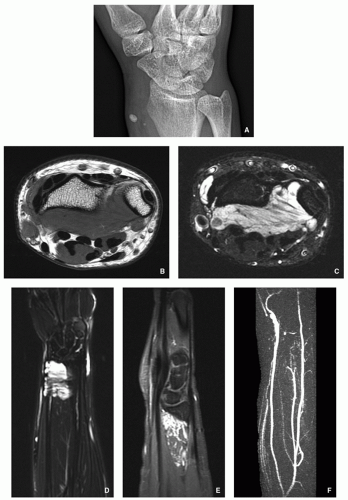
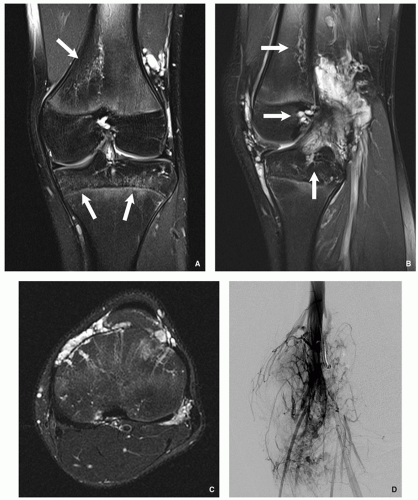
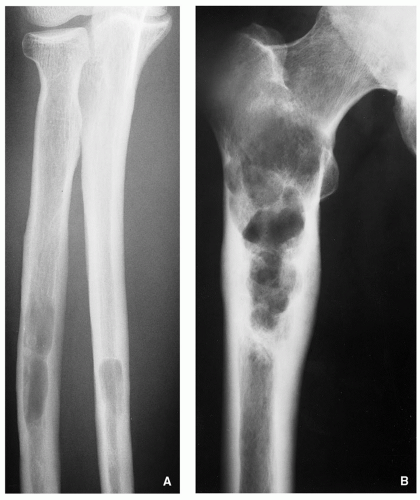
On radiography, an osseous hemangioma in a long or short tubular bone is characterized by lace-like pattern, by coarse striations, or by focal lytic area (Fig. 6.1). In flat bones, they commonly expand the bone contour and produce rarefaction with radially oriented striations; overlying cortex is expanded and thinned, but complete cortical disruption and invasion into soft tissue are generally not present. In the vertebral body, hemangioma is characterized by either vertical striations (corduroy cloth pattern) or multiloculated lytic foci (honeycomb pattern) (Figs. 6.2 and 6.3). Characteristic sunburst appearance is seen in skull lesions with thickened trabeculae arranged in a spoke-wheel or web-like pattern. In concomitant involvement of the soft tissues, the hallmark is the phlebolith (see Fig. 6.8).
Scintigraphy shows either photopenia or only moderate increase of uptake of radiopharmaceutical tracer.
On computed tomography, “honeycomb” pattern may be observed in the long tubular and flat bones (Fig. 6.4), whereas vertebral hemangiomas characteristically exhibit pattern of a multiple dots (“polka-dot” appearance) (Fig. 6.5).
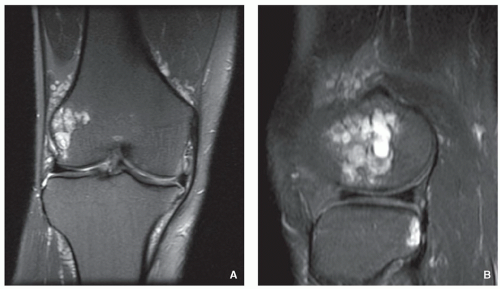
Magnetic resonance imaging (MRI) generally reveals a high signal on T1-weighted and T2-weighted images (blood content of tumor vessels), with areas of trabecular
thickening imaged in low signal intensity regardless of the pulse sequence. After intravenous administration of gadolinium, there is always significant enhancement of the lesion (Figs. 6.6, 6.7, 6.8, 6.9 and 6.10).
Pathology:
Gross:
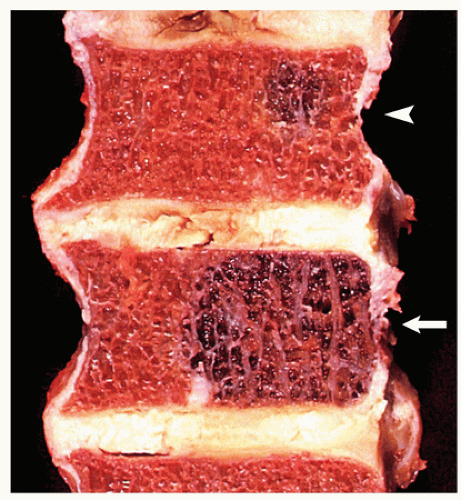
Brown-red or dark red, well demarcated, medullary lesion (Fig. 6.11).
It may have a honeycomb appearance with sclerotic bone trabeculae interspersed among hemorrhagic cavities.
Histopathology:
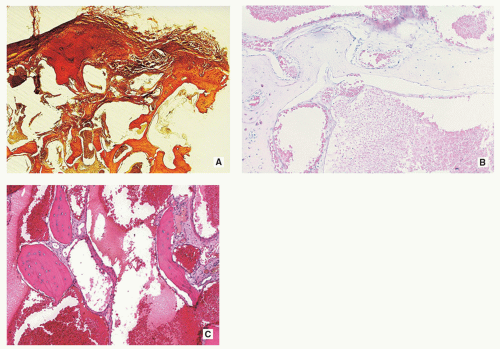
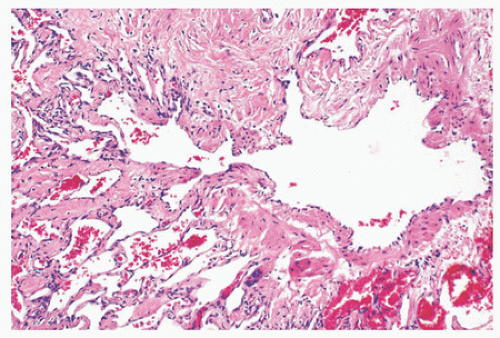
Hemangiomas are composed of conglomerate of thinwalled blood vessels (Fig. 6.12A,B).
Vascular channels are lined by a single layer of flat endothelial cells (Fig. 6.12C).
Vessels can have dilated open channels (cavernous hemangioma) or less commonly may be composed of capillarysized vessels (capillary hemangioma).
Majority of bone hemangiomas are of cavernous or mixed types (Fig. 6.13).
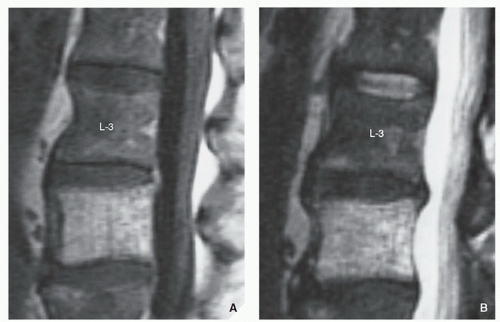
FIGURE 6.7 Magnetic resonance imaging of intraosseous hemangioma. (A) Sagittal T1-weighted and (B) T2-weighted MR images show high intensity signal of hemangioma of L4 vertebra.
Intercellular tissue is composed of loose connective tissue that may show myxoid change.
Bone may be completely resorbed in affected area.
Vascular channels of hemangioma are complete, are separate, and do not show anastomosing pattern.
Immunohistochemistry:
Endothelial cells are positive for CD31, CD34, and factor VIII-related antigen.
Prognosis:
Asymptomatic small hemangiomas require no treatment; some may undergo spontaneous regression.
Symptomatic lesions or those that are large and may cause pathologic fracture or vertebral collapse require treatment; curettage and bone grafting usually is sufficient.
Differential Diagnosis:
▪ Aneurysmal bone cyst
Imaging shows the lesion ballooning out of the cortex, associated with periosteal reaction, usually in the form of well-defined buttress. Scintigraphy shows increased uptake in a ring-like pattern around the periphery of the lesion. MRI shows fluid-fluid levels.
Histopathology showing blood-filled spaces alternating with solid areas composed of fibrous; richly vascular connective tissue containing clusters of giant cells is diagnostic.
Epithelioid Hemangioma (Angiolymphoid Hyperplasia with Eosinophilia)
Definition:
A benign but locally aggressive vascular neoplasm with endothelial phenotype and epithelioid morphology.
Epidemiology:
Rare bone tumor (most common in skin and subcutis).
Patient age range from 10 to 90 years with average age of 35 years.
Male-to-female ratio of 1:1.4.
Sites of Involvement:
Most common involvement of long tubular bones (40%), short tubular bones of lower extremities (18%), flat bones (18%), vertebrae (16%), and small bone of the hands (8%).
Multifocal distribution can be seen.
Clinical Findings:
Pain localized to involved anatomical site.
Imaging:
Identical imaging features as of hemangioma (see above).
Pathology:
Gross (Macroscopy):
Well-defined nodular, soft, solid, hemorrhagic mass.
Most tumors less than 7 cm in size.
May expand bone and extend into soft tissue.
Histopathology:
Lobular architecture, infiltrates preexisting bone trabeculae.
Periphery of the lobules may show small vessels lined by endothelial cells.
Center of the lobules are more cellular and contain epithelioid cells with abundant eosinophilic cytoplasm.
Epithelioid cells are large, plump, and have oval or kidney bean-shaped nuclei with uniformly distributed chromatin.
Abundant eosinophilic cytoplasm with occasional one or two vacuoles.
Cells with vacuoles may aggregate.
Most tumors contain small well-formed vessels with open lumina surrounded by epithelioid cells sometimes arranged in tombstone-like pattern.
Infrequent mitoses can be seen but without atypia.
Loose connective stroma that may contain inflammatory component, mostly eosinophils.
Intralesional hemorrhage may be seen.
Osteoclast-type giant cells can be seen.
Immunohistochemistry:
Positive for factor VIII, CD31, CD34, Fli-1, EGR, and ulex europaeus.
May be positive for cytokeratin and epithelial membrane antigen (EMA).
Prognosis:
Locally aggressive lesion, successfully treated with curettage or marginal bloc excision.
Local recurrence rate of about 9%.
Differential Diagnosis:
Same as for hemangioma (see above).
Cystic Angiomatosis
Definition:
Rare condition, characterized by disseminated multifocal cystic in appearance hemangiomas affecting the skeleton, commonly associated with visceral involvement.
Epidemiology:
Most cases are recognized in the first three decades of life.
Male-to-female ratio of 2:1.
Sites of Involvement:
Skull, spine, ribs, long bones (femur, tibia, fibula, humerus), and pelvic bones.
Extraskeletal involvement includes soft tissues, lung, liver, and spleen.
Clinical Findings:
Most of the time the patients are asymptomatic, the lesions detected incidentally by imaging studies obtained for other reasons (trauma).
Patients may be symptomatic if there is concomitant visceral involvement.
Imaging:
Radiography shows well-defined lytic lesions (Fig. 6.14), often with honeycomb or lattice work (“hole-withinhole”) appearance (Fig. 6.15); the lesions may exhibit sclerotic border, and cortex may be thickened; periosteal reaction is rare.
MRI shows the lesions to be of intermediate signal intensity on T1-weighted sequences, whereas T2 weighting shows mixture of high, low, and intermediate signal intensities.
Pathology:
Gross (Macroscopy):
Resemble simple bone cyst with multiple communicating cavities lined by a dull, yellowish-gray membrane, separated by thickened bone trabeculae.
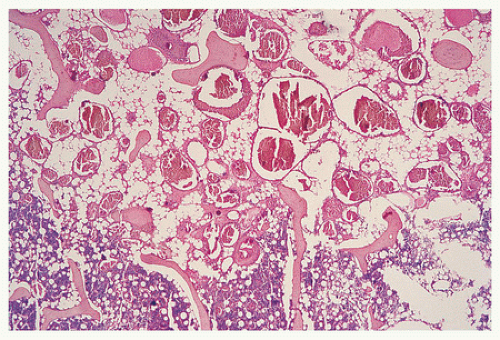
Histopathology:
Indistinguishable from cavernous hemangiomas.
Multiple dilated, thin-walled vascular channels lined by flat endothelial cells (Fig. 6.16).
Occasionally osteoid and immature woven bone formation with osteoblasts rimming may be present.
Admixture of dilated lymphatics can be seen.
Sclerotic variant may show vessels with perivascular thick sclerotic bone.