CHAPTER 75 Venous Anatomy of the Thorax
THE VENAE CAVAE
The Superior Vena Cava
The superior vena cava (SVC) is the primary means of blood return to the heart from the upper extremities, head, and neck. It forms from the convergence of the right and left brachiocephalic veins (also known as the innominate veins) and ends at its entrance into the right atrium. The lower half of the vessel lies within the pericardium.1 The SVC has a slightly convex vertical course, with its apex to the right, beginning immediately below the first costosternal junction and ending opposite the upper border of the third right costal cartilage. It measures approximately 7 cm in length, with its midpoint near the level of the carina on a frontal chest radiograph.2
In cross-sectional imaging, the beginning of the SVC can be recognized at the junction of the brachiocephalic veins in the upper mediastinum, posterior and slightly inferior to the right clavicular head and just above the prevascular space (Fig. 75-1). The course of the SVC lies slightly to the right of midline, adjacent to the ascending aorta, and passes anterior to the right pulmonary artery before entering the heart (Fig. 75-2). When CT imaging of the chest is performed after an upper extremity injection of intravenous contrast material, the SVC can often be recognized as the densely opacified structure draining into the heart and creating some streak artifact in this area.
Variant Anatomy
To understand the duplicated and left-sided SVC variants, one must first understand the venous embryologic development. The venous system begins its development in the earliest stages of intrauterine life as a symmetrical structure of paired cardinal and subcardinal veins. Early in the intrauterine period, the paired cardinal veins run the entire length of the embryo. There is a larger and more developed dorsally positioned caudal tract (the right and left posterior cardinal veins) and a more ventrally located cranial tract (the right and left anterior cardinal veins). The common cardinal veins originate from where the posterior and anterior cardinal veins converge and reach the primitive heart, the sinus venosus, from both the right and left sides. In a normal progression of development, the inferior portion of the left anterior cardinal vein regresses, and an anastomotic channel is formed between the right and left anterior cardinal veins, which becomes the left brachiocephalic vein. This vein allows drainage from the left side to the right. The superior portion of the left anterior cardinal vein becomes the superior intercostal vein, which drains the second and third left intercostal spaces. The normal right-sided SVC forms from the right common cardinal vein and the right anterior cardinal vein.3 When the left distal anterior cardinal vein persists, a left-sided vena cava forms (Fig. 75-3). The incidence of a left-sided vena cava is 0.3% to 0.5% in the general population and 4% in patients with congenital heart disease.4
A left-sided SVC may or may not be accompanied by regression of the right anterior cardinal vein and the right common cardinal vein, which form the normal right-sided SVC. Without regression, both a right and left SVC develop, resulting in a duplicated SVC system, with an absent left brachiocephalic vein and smaller right SVC in 65% of cases (Fig. 75-4). Duplicated SVC occurs in 0.3% to 0.5% of the population and in approximately 11% of patients with congenital heart disease.5
With regression of the cardinal veins that form the right SVC, blood from the right side of the embryo drains from the right brachiocephalic vein to the left SVC, which then drains most commonly into the coronary sinus and on into the right atrium. Cross-sectional imaging of a left-sided SVC shows it coursing caudally to the left of the aortic arch and left main pulmonary artery within the mediastinum, passing medially to the left superior pulmonary vein, before emptying into the coronary sinus (Fig. 75-5). Although it is most commonly asymptomatic, the resultant dilation of the coronary sinus can rarely cause conduction abnormalities. In the absence of other congenital cardiac anomalies, a left-sided SVC with absent right SVC and visceroatrial situs solitus occurs in fewer than 0.1% of the population.6 Finally, a left-sided SVC can drain directly into the left atrium, producing a right-to-left shunt. This anomaly is rare and is usually associated with congenital cardiac anomalies.
The Inferior Vena Cava
The thoracic segment of the inferior vena cava (IVC), the suprahepatic segment, is very short; it crosses the diaphragm through the caval opening or foramen in the central tendon at approximately the level of T8. Branches of the phrenic nerve that are separated by fibrous pericardium accompany it.7 The drainage of the IVC into the right atrium is considered to be a reliable marker for determination of the atrial situs because the suprahepatic IVC almost never drains into a different cavity.8 The normal embryologic precursor to the suprahepatic IVC is the right supracardinal vein.
Variant Anatomy
Developmental anomalies of the IVC are rare, occurring in fewer than 1% of those with congenital heart disease.9 The embryogenesis of the IVC involves formation of several anastomoses of three paired embryonic veins. Variations in this development result in several important anomalous drainage patterns. The most common variation is absence of the suprahepatic IVC with azygos continuation of the IVC. It results from the involution of a segment of the supracardinal vein, leading to drainage of the infrahepatic IVC into the azygos vein; the hepatic veins continue to drain directly into the right atrium.8 The prevalence is 0.6%.10 An enlarged azygos vein will then join the SVC at the normal location in the right paratracheal space. Imaging findings include absence of the suprahepatic segment on the lateral view of a chest radiograph and a mass in the right paratracheal space on the anteroposterior view, in the expected region of the azygos vein. Cross-sectional imaging delineates the dilated azygos ascending along its normal course to drain into the SVC (Fig. 75-6).

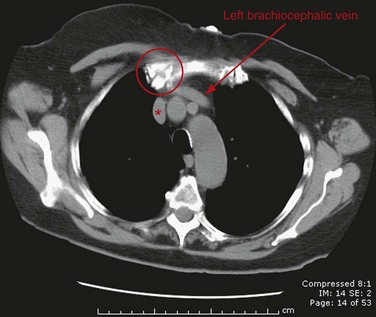
 FIGURE 75-1
FIGURE 75-1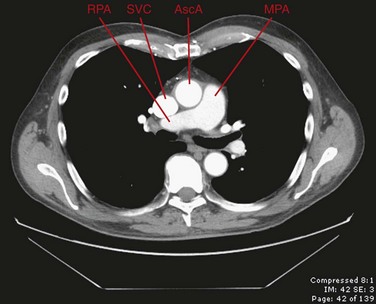
 FIGURE 75-2
FIGURE 75-2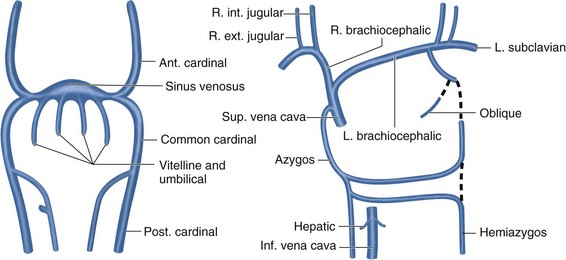
 FIGURE 75-3
FIGURE 75-3
 FIGURE 75-4
FIGURE 75-4
 FIGURE 75-5
FIGURE 75-5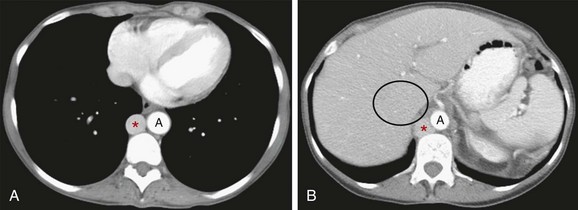
 FIGURE 75-6
FIGURE 75-6

