CHAPTER 118 Venous Sonography of the Upper Extremities and Thoracic Outlet
Upper extremity deep venous thrombosis (DVT) was historically considered an uncommon, benign, and self-limited condition.1 As such, thrombi involving the upper extremities were thought to be of little clinical significance and often undertreated because the risk of propagation was also believed to be low. More recent studies have found this not to be the case. The incidence of upper extremity DVT is far more common than previously thought, especially with the increased use of central venous catheters and placement of cardiac pacemakers, and in patients with cancer and hypercoagulable states. Upper extremity DVT is also seen to be associated with significant complications, including pulmonary embolism, superior vena cava syndrome, postthrombotic venous insufficiency, and loss of venous access.
VENOUS ANATOMY
The relevant venous anatomy of the upper extremities and thoracic inlet includes the deep venous system composed of the internal jugular, brachiocephalic (or innominate), subclavian, axillary, and paired brachial veins. The superficial basilic and cephalic veins are also usually included in the examination (Fig. 118-1).
The axillary vein lies medial and inferior to the axillary artery. The subclavian vein is anterior and inferior to the subclavian artery (Fig. 118-2). Knowing these relationships will aid in identification of these vessels and help in distinguishing possible large collaterals from the native vessels.
PREVALENCE, ETIOLOGY, AND RISK FACTORS
The exact prevalence of symptomatic upper extremity DVT in the general population is unknown but is estimated to be approximately 0.2%.2 In patients with deep venous thrombosis, approximately 90% involve the lower extremity and the remaining 10% involve the upper extremity.3
With the increasing use of central venous catheters, the prevalence of upper extremity DVT has increased (Fig. 118-3). Earlier studies documented thrombosis in 2% to 12% of patients with central venous catheters.4 In more recent studies, upper extremity DVT has been documented in 50% to 60% of patients with central venous catheters. The most powerful independent predictor of upper extremity DVT was the presence of a catheter, with the risk factor increasing sevenfold in these patients.5,6 The position of the catheter tip has been found to correlate with the incidence of upper extremity DVT. Catheters at the junction of the right atrium and the superior vena cava and those in the mid superior vena cava (SVC) have the lowest incidence of associated thrombosis and those with the catheter tip in the brachiocephalic vein have a higher incidence.4 The ideal position for the catheter tip is at the cavoatrial junction. Catheter material and diameter have also been found to affect the incidence of thrombus. The lowest rates have been for polyurethane and silicone catheters and for those with an external diameter less than 2.8 mm.7,8 In the pediatric population, two thirds of DVT cases occur in the upper extremity, in contrast to adults, and are usually secondary to catheter placement.6
Cancer is a significant risk factor for upper extremity DVT secondary to alterations in coagulability factors, low-grade disseminated intravascular coagulation, and stasis secondary to tumor compression.9 Bilateral upper extremity DVT was found to be more common in patients with malignancy. The risk of thrombosis increases significantly in patients with both cancer and central venous catheters.11
Hypercoagulability (e.g., antithrombin, protein C, and protein S deficiencies; presence of antiphospholipid antibodies) is found to be prevalent in idiopathic upper extremity DVT in which no obvious associated disease or triggering factor is present. In patients with idiopathic upper extremity DVT, 42% to 56% of patients have been found to have clotting abnormalities in recent studies.6,13,14 Transient causes of hypercoagulability such as estrogen use, pregnancy, and ovarian hyperstimulation have also been observed in women with idiopathic upper extremity DVT.11,12
Additional predisposing factors for upper extremity DVT include venous stasis, trauma, surgery, sepsis, and thoracic outlet obstruction secondary to anatomic anomalies. Interestingly, conventional risk factors associated with lower extremity DVT, including obesity, advanced age, and surgery were not significant risk factors for patients with non–catheter-related upper extremity DVT.3 Patients with upper extremity DVT were found to be more often male, younger, leaner, and more likely to smoke than those with lower extremity DVT. Recent immobility and prior venous thromboembolism also play less of role in patients with upper extremity DVT; however, cancer was more common.13
COMPLICATIONS
The most serious complication of upper extremity deep venous thrombosis is pulmonary embolism (PE). Once thought to be uncommon, PE is now reported to have a prevalence of 7% to 36% in patients with upper extremity DVT.2,13,14 Clinically, the prevalence of symptomatic PE at presentation has been reported to be fourfold less common in patients with upper extremity DVT when compared with patients with lower extremity DVT. However, after 3-month follow-up, the incidence of major or fatal bleeding, recurrent DVT, recurrent PE, or fatal PE was the same. Not surprisingly, patients with cancer were found to have the worst prognosis. Mortality from PE ranged from 11% to 34%.13
CLINICAL PRESENTATION
Clinically, the most common presentation of upper extremity DVT is upper extremity and face swelling and pain. The edema is typically nonpitting. Less common signs and symptoms include skin discoloration, a sense of coldness in the hand and forearm, tenderness over the affected vein, paresthesia, and numbness. Malfunction of a central venous catheter may also be an indication of thrombosis. Collateral veins can develop over the shoulder and chest wall. A tender cord may be palpable, especially in the axillary region. These signs and symptoms, however, are nonspecific and confirmation of the diagnosis by objective testing is necessary.14 In addition, many cases of upper extremity DVT are asymptomatic, especially when related to catheter placement.4
IMAGING TECHNIQUE
Color Doppler duplex ultrasonography with compression technique has become the imaging modality of choice for the diagnosis of upper extremity DVT and is highly accurate for making this diagnosis.15 Sonography has the advantage of being noninvasive, requiring no venipuncture, ionizing radiation, or contrast agent. It is a potentially portable examination and can be performed at the bedside for critically ill patients. It can be performed regardless of renal function and serial follow-up examinations are easily done. Unlike venography, the internal jugular and peripheral brachiocephalic veins can be evaluated, despite the presence of thrombus in the more peripheral vessels. Limitations of duplex sonography include inability to visualize the superior vena cava and more central portions of the brachiocephalic veins. In addition, small nonocclusive thrombus may be missed in the subclavian vein secondary to the inability to compress this vessel because of the overlying clavicle.16 Furthermore, differentiation of a large collateral from the native vein may be difficult in patients with chronic deep venous thrombosis.
The reported sensitivity of color Doppler sonography for the diagnosis of upper extremity DVT has ranged from 78% to 100%, with a specificity of 82% to 100%.17,18 False-positive examination results are thought to be rare. False-negative results can occur secondary to limitations in the ability to compress vessels (see earlier).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


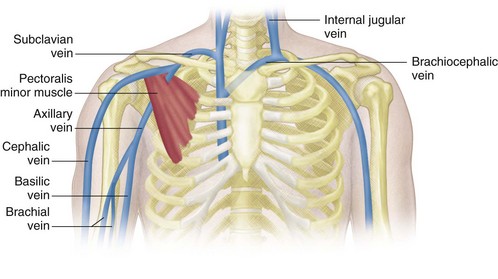
 FIGURE 118-1
FIGURE 118-1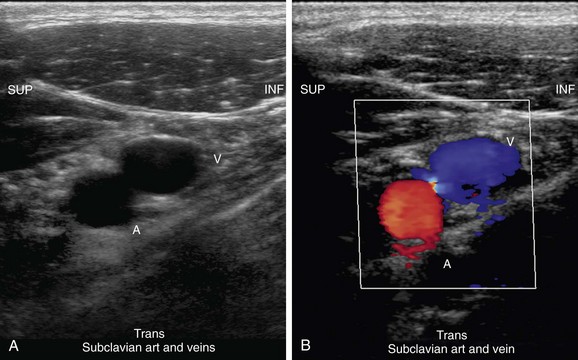
 FIGURE 118-2
FIGURE 118-2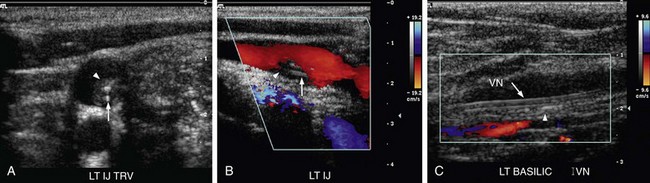
 FIGURE 118-3
FIGURE 118-3