- •
Location of defect on the ventricular septum.
- •
Size of defect in relation to aortic annulus.
- •
Direction of shunting across the defect.
- •
Presence or absence of valve tissue (i.e., tricuspid valve) through the defect.
- •
Any associated findings such as outflow tract obstruction, semilunar valve narrowing, or coarctation of the aorta.
Anatomy and Anatomical Associations
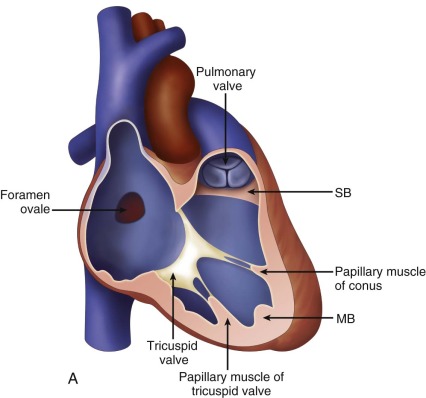
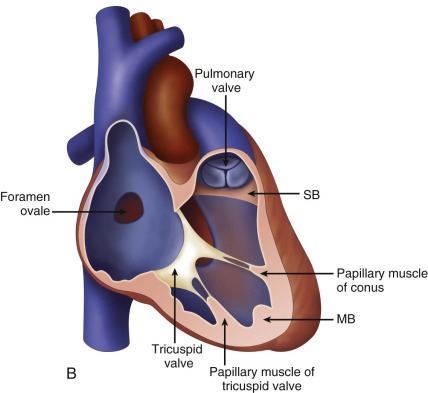
The ventricular septum is a helical structure that separates the right and left ventricles. More than simply a wall of separation, it is a complex structure made up of many different components. It is predominantly made up of a small thin membranous septum and a larger muscular septum. The membranous septum is bounded superiorly by the aortic valve at the junction of the right and noncoronary cusps and inferiorly by the muscular septum. The muscular septum is further divided into a posterosuperior inlet septum contributing to the separation between the mitral and the tricuspid valves, a trabecular septum in the middle and extending to the apex, and an anterosuperior smooth-walled outlet or conal septum. Endocardial cushion tissue further contributes to the ventricular septum between the two atrioventricular (AV) valves, the “atrioventricular (AV) canal” septum. Looking at it geographically, the “inlet” portion of the septum adjacent to the AV valves is composed of the AV canal septum and the posterior muscular septum. The “outlet” portion of the septum is composed of the muscular conal septum. A ventricular septal defect (VSD) is a communication between the right and the left ventricles due to a defect in the ventricular septum.
Postnatally, the most common type of VSD involves the membranous septum and typically extends into the surrounding structures. This is referred to as a conoventricular or perimembranous VSD ( Figure 7-1 ) and accounts for up to 80% of cases. This defect lies below the aortic valve when viewed from the left ventricle and underneath the septal leaflet of the tricuspid valve when viewed from the right ventricle. It can be covered by tricuspid valve tissue leading to partial or complete closure of the defect. Conoventricular VSDs can be associated with other forms of congenital heart disease. Additionally, subaortic membrane, prolapse of the aortic cusp with development of aortic insufficiency, and right ventricular muscle bundles are some of the associations that can develop postnatally but are rarely, if ever, seen before birth.




Defects in the muscular trabecular septum account for 5% to 20% of all VSDs. They are further classified depending on location: apical, central, posterior, and anterior muscular defects, with apical defects being the most common subtype of muscular defects. Multiple defects in the trabecular septum can give it a “Swiss cheese” appearance and can be particularly challenging to manage after birth. The incidence of muscular defects is significantly higher in the prenatal period and declines after birth owing to a high rate of spontaneous closure of small muscular VSDs in utero. In fact, some consider the presence of a muscular defect in the fetus to be so common as to be considered a variant of normal because, on subsequent scanning, many are no longer seen and are thought to spontaneously close. This, however, raises the question of whether there is simply a high rate of “false-positive” identification. Small jets noted along the septum on color Doppler imaging may be spuriously suspected of being a tiny muscular defect.
The inlet septum is located between the two AV valves, inferior to the membranous septum and posterosuperior to the trabecular septum. A VSD in the inlet septum is often referred to as an inlet or AV canal type VSD and is found in approximately 5% to 8% of patients with VSDs.
The outlet or the conal septum is located anterosuperior in relation to the trabecular septum and inferior to the aorta and the pulmonary artery. The conus is the region beneath the pulmonary valve that lifts the pulmonary valve above the level of the other three heart valves. The conal septum separates the outlet portion of the right ventricle on the right side from the region beneath the aortic valve on the left side. Defects in this region can be of either the conal septum malalignment type or an actual deficiency in conal tissue referred to as conoseptal hypoplasia type. Conal defects constitute 5% to 7% of all VSDs. The conal malalignment type involves varying degrees of displacement or malalignment of the conal septum with respect to the remainder of the ventricular septum. In a patient with normally related great arteries, anterior malalignment of the conal septum can cause subpulmonary obstruction. This type of VSD is typically seen in association with tetralogy of Fallot and is associated with aortic override. Posterior malalignment of the conal septum can cause subaortic stenosis and may be associated with coarctation of the aorta or interruption of the aortic arch.
Frequency, Genetics, and Development
Aside from a bicuspid aortic valve, VSDs are the most common of all congenital heart defects. The incidence has been reported to be 1% to 2% among live-born infants. Prenatally, however, VSDs are only the fifth most common congenital heart defect to be identified echocardiographically. Over the years, possibly due to improved diagnostics, the incidence of children diagnosed with a VSD is rising.
In utero, partitioning of the primitive heart tube starts at the beginning of the fourth week of gestation and is completed by the eighth week. The right and left ventricles are formed with the septation of the primordial ventricle and the bulbus cordis (see Chapter 2 ). Initially, development of the muscular septum starts as a ridge in the floor of the primordial ventricle. The free wall of the ridge is concave and is separated from the endocardial cushions posterosuperiorly and the bulbus cordis anterosuperiorly by a crescent-shaped interventricular foramen. Meanwhile, there is active proliferation of mesenchymal cells in the endocardial cushions as well as in the right and left bulbar ridges within the walls of the bulbus cordis. The membranous part of the interventricular septum is derived from an extension of tissue from the endocardial cushions. Closure of the interventricular foramen and completion of the membranous septum results from fusion of tissue derived from the endocardial cushions, the bulbar ridges, and the muscular septum. A VSD can result either from maldevelopment or failure of fusion of one of the components or from excess resorption of myocardial tissue in the formation of the trabeculae in the muscular septum.
Although a majority of VSDs are isolated lesions, they are associated with other cardiac anomalies in 18% of fetuses and extracardiac and chromosomal anomalies (e.g., trisomy 21, 13, and 18) in as many as 47% of cases. VSDs are also one of the most common teratogen-associated cardiac defects and are known to occur with prenatal exposure to alcohol and marijuana. The exact etiology of VSDs, however, does not follow a fixed genetic pattern and is believed to be multifactorial. When one parent has a VSD, the risk in the fetus is increased to 3% to 4%. The risk in the fetus is increased to 2% to 5% when a previous sibling has a VSD and to 10% to 15% with two affected siblings.
Prenatal Physiology
In the fetus, the right ventricle pumps against a high resistance in the pulmonary vascular bed and into the systemic circulation through a patent ductus arteriosus. The right ventricular pressure is, thus, equal to the left ventricular pressure throughout fetal life. An isolated VSD usually does not cause any significant hemodynamic effects prenatally. Application of color Doppler imaging onto a VSD may not demonstrate much shunting of flow on fetal echocardiography. Nevertheless, because the left ventricle normally contracts a few milliseconds before the right ventricle, one may see left-to-right shunting across a VSD during systole.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








